 J Clin Aesthet Dermatol. 2022;15(11):37–39.
J Clin Aesthet Dermatol. 2022;15(11):37–39.
by Christian Gronbeck, MD* and Ashley M. Hine, BS*; Jeffrey M. Cohen, MD; and Hao Feng MD, MHS
*Dr. Gronbeck and Ms. Hine share co-first authorship on this article. Ms. Hine is with the University of Connecticut School of Medicine in Farmington, Connecticut. Drs. Gronbeck and Feng are with Department of Dermatology at University of Connecticut Health Center in Farmington, Connecticut. Dr. Cohen is with the Department of Dermatology at Yale University School of Medicine in New Haven, Connecticut.
FUNDING: No funding was provided for this article.
DISCLOSURES: Dr. Feng is a consultant at Cytrellis Biosystems, Inc and Soliton Inc.
ABSTRACT: Objective. Photodynamic therapy (PDT) is a useful treatment modality for premalignant skin lesions. We sought to describe PDT utilization on a national level in the Medicare population post-CPT code revision in 2018 to better understand trends in volume and distribution as well as what factors may influence service performance.
Methods. We used the 2018–2019 Medicare Physician and Other Supplier Public Use File to assess PDT services performed during this period.
Results. We found that there was an increasing trend of PDT utilization in the Medicare population. While there was less PDT performed without direct involvement of a healthcare professional, an increasing number of PDT services requiring debridement were performed for severe lesions. Although the majority of PDT volume was attributable to dermatologists, non-physician clinicians assumed greater involvement in PDT services. Dermatologists practicing in academic and non-metropolitan settings were less likely to be directly involved with PDT delivery.
Conclusion. There is a considerable volume of PDT performed among Medicare beneficiaries, with several utilization trends that may be explained by geographic location and practice setting, among other factors. These findings provide insight to PDT service distribution on a national level and highlight practice patterns that may influence PDT delivery.
Keywords: Photodynamic therapy, dermatology, debridement, non-physician clinicians, Medicare
Photodynamic therapy (PDT) is a field-directed therapy for premalignant actinic keratoses and is an effective treatment modality for certain superficial keratinocytic carcinomas (KCs).1 Despite its increasing utilization in the Medicare population2, the volume and distribution of PDT services performed by dermatologists and other providers have not been characterized since the implementation of revised Current Procedural Terminology (CPT) codes in 2018, which now capture direct healthcare professional involvement in PDT delivery as well as any preceding debridement.3
Methods
We analyzed the 2018–2019 Medicare Physician and Other Supplier datasets to describe the overall volume and relative proportion of PDT services performed with and without direct involvement of a healthcare professional (e.g., dermatologist, non-physician clinician [NPC]), and with preceding debridement.4 We summarized aggregate utilization statistics and also stratified our assessment across specific subsets of dermatologists and NPCs. We further assessed the relative utilization of each PDT service type at the state level.
Results
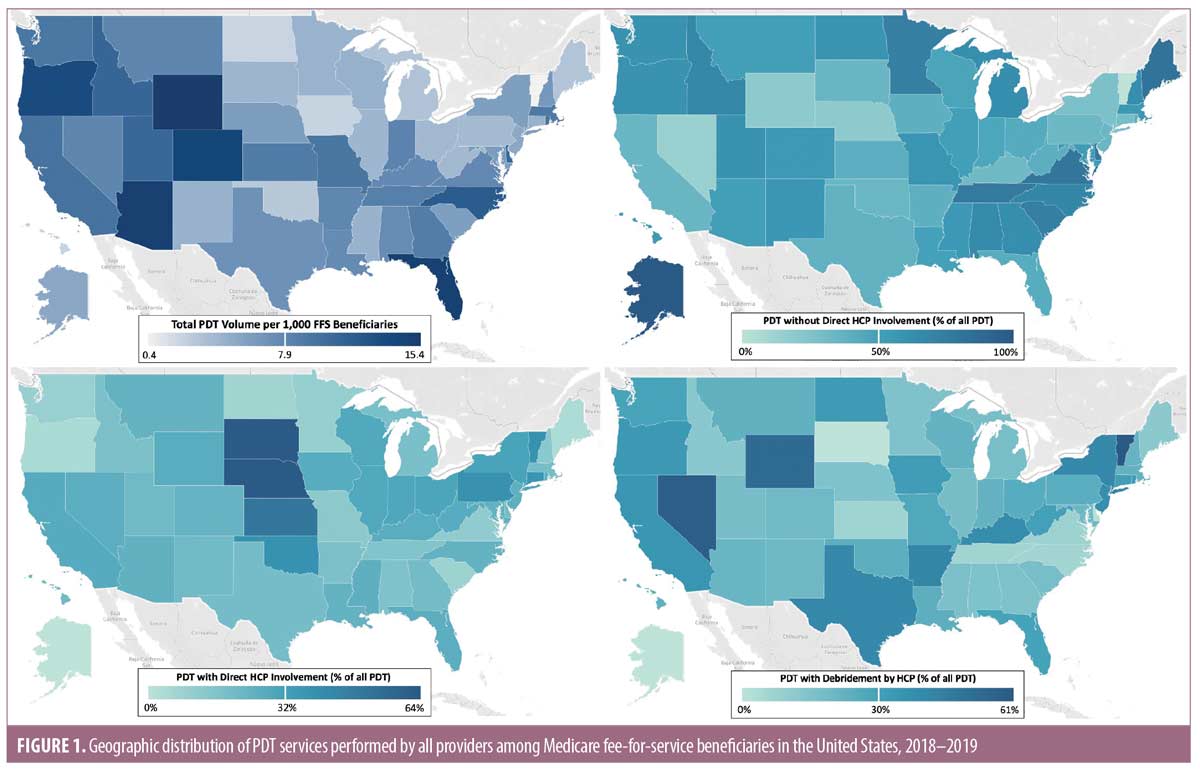
Across all providers, 152,310 PDT procedures were performed in 2019, representing an increase of 5.9 percent from 2018. Geographically, total PDT volume was highest in the Pacific, Mountain, and South Atlantic states (Figure 1). The proportion of PDT services performed without direct involvement of a healthcare professional decreased from 55.7 percent to 43.9 percent in 2019, primarily due to a significant increase in PDT services requiring preceding debridement (Table 1).
Discussion
These findings support increasing healthcare professional direct involvement in delivery of PDT, primarily in cases with more severe premalignant lesions requiring debridement. However, regions with classically high sun exposure and overall greater PDT volume (South, Pacific) exemplified a relatively high proportion of services performed without direct physician involvement, which might be due to physician time constraints relative to demand, challenges in changing existing processes directed by other office staff, or lack of knowledge regarding CPT code changes.
Dermatologists still billed for the vast majority of PDT services in 2019, although independently-billing NPCs assumed a growing role over the study period, including more direct involvement in PDT relative to dermatologists and in cases requiring debridement. Dermatologists in non-metropolitan regions were less likely to be directly involved with PDT services in their clinics, which could be related to the lower density of dermatologists and other providers in these regions.2 The frequent direct involvement in PDT by solo practice dermatologists may be explained by fewer resources and ancillary staff capable of delivering PDT at these practices. By comparison, continuing medical education and training activities at academic centers may foster PDT proficiency among office staff, potentially enabling less frequent direct involvement exhibited by dermatologists in these settings.
Limitations. This analysis has several limitations. Findings from Medicare data may not be generalizable to patients with commercial insurance. Furthermore, providers performing fewer than 11 annual PDT procedures are excluded, leading to slight underestimations at the provider (not aggregate) level. Nevertheless, this study supports an increasing trend in PDT services and provides greater insight into PDT service distribution among Medicare beneficiaries. Further studies assessing the reasons for these practice patterns are warranted.
References
- Ozog DM, Rkein AM, Fabi SG, et al. Photodynamic Therapy: A Clinical Consensus Guide. Dermatol Surg. 2016;42(7):804–827.
- Cheraghlou S, Feng H, Cohen JM. Trends in the Access and Cost of Photodynamic Therapy Among Medicare Beneficiaries in the United States, 2012-2017. JAMA Dermatol. Sep 1 2020;156(9):1021–1022.
- Siegel DM. Let there be light: update on coding for photodynamic therapy and lasers. Cutis. Mar 2018;101(3):180–182.
- Centers for Medicare and Medicaid Services. Medicare Physician & Other Practitioners – by Provider and Service. Accessed September 29, 2021. https://data.cms.gov/provider-summary-by-type-of-service/medicare-physician-other-practitioners/medicare-physician-other-practitioners-by-provider-and-service.

