 J Clin Aesthet Dermatol. 2019;12(5):11–18
J Clin Aesthet Dermatol. 2019;12(5):11–18
by Nima Milani-Nejad MD, PhD; Catherine Chung, MD; and Jessica Kaffenberger, MD
All authors are with the Division of Dermatology in the Department of Internal Medicine at The Ohio State University Wexner Medical Center in Columbus, Ohio.
Funding/disclosures. Dr. Kaffenberger is a principal investigator for AbbVie, AnaptysBio, Bristol-Myers, Cara Therapeutics, Celgene, Corrona, Eli Lilly, Janssen, Novartis, Pfizer, Regeneron, Xbiotech. The other authors have no conflicts of interest relevant to the content of this article.
Dear Editor:
Pemphigus foliaceous (PF) is an autoimmune blistering disorder in which antibodies targeting desmoglein-1 result in the formation of crusted erosions and flaccid blisters.1 This disorder typically involves the scalp, face, and upper trunk in a symmetrical distribution pattern. Here, we describe a patient with a history of generalized PF in remission after treatment with rituximab who developed localized PF on her leg following a knee replacement.
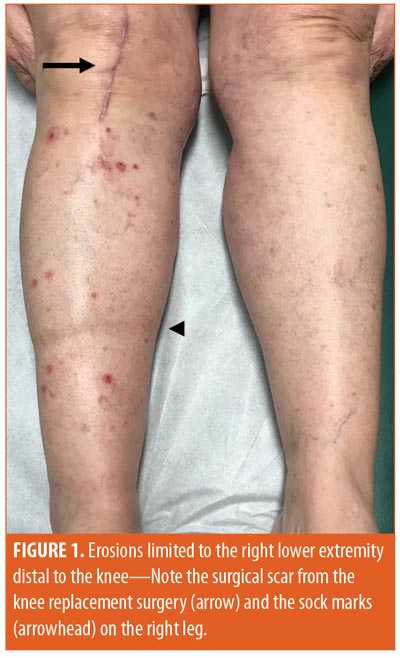
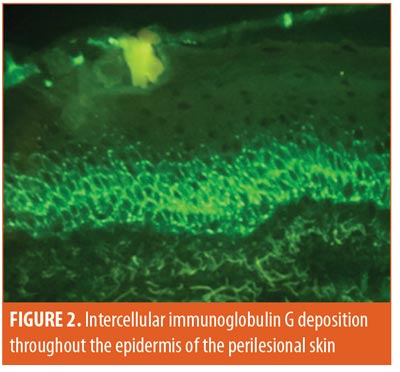
Case report. A 68-year-old woman originally presented to our clinic with a diagnosis of PF that was previously treated with prednisone, mycophenolate mofetil, dapsone, hydroxychloroquine, and rituximab. She was noted to have eroded, crusted plaques and papules in multiple areas, including the scalp, face, chest, back, and upper extremities. Due to persistent disease activity, she was treated with a second course of rituximab and subsequently achieved remission without any disease activity. One year later, she underwent surgical replacement of the right knee for osteoarthritis and developed flaccid blisters and erosions limited only to the right lower extremity (Figure 1). She also reported numbness and swelling in this area. No other areas were involved. Direct immunofluorescence studies of perilesional skin showed prominent intercellular immunoglobulin G and C3 deposition throughout the epidermis (Figure 2), consistent with pemphigus foliaceous. She was started on potent topical corticosteroids, with subsequent rapid improvement of her lesions.
Discussion. To our knowledge, this is the first case of localized recurrence of PF in a patient with a history of generalized PF. This unique presentation can present a diagnostic challenge, and our observations might help shed light on the pathogenesis of this disorder.
Localized PF, although rare, has been previously described in the literature; however, all reported cases were limited to the scalp and face area.2 Furthermore, the initial presentation of these cases was the localized form of PF, without any history of classical PF in a more widespread distribution. Given the sun-exposed distribution, it is postulated that ultraviolet radiation has a role in these localized cases of PF.2
Interestingly, a patient with breast cancer developed pemphigus vulgaris lesions in the mouth and on the breast that underwent radiation therapy, further highlighting the possible role of radiation in such cases.3 However, our patient had no history of radiation therapy or sun exposure; furthermore, she had a documented history of classical presentation of PF with a more widespread involvement of the scalp and trunk.
There are several reports of unilateral bullous pemphigoid (BP), another autoimmune blistering disorder, in which BP lesions are localized only to the affected limb after a cerebrovascular accident or venous stasis.4,5 These unilateral BP presentations are often explained by the concept of an immunocompromised district.6 In this model, alterations of neuromodulators and the trafficking of immune cells induced by nerve damage and disruption in circulation result in a localized altered immune response.6 Our patient might have had a limited number of antibodies and thus was unable to induce generalized PF. The right lower-extremity edema and possible nerve injury secondary to surgery might have resulted in an immunocompromised district whereby there was a buildup of immunoglobulins and immune cells, resulting in localized presentation of pemphigus.
Conclusion. This case highlights the complex pathogenesis of autoimmune blistering disorders and their associated triggers, which warrants further investigation.
References
- Pollmann R, Schmidt T, Eming R, et al. Pemphigus: a comprehensive review on pathogenesis, clinical presentation and novel therapeutic approaches. Clin Rev Allergy Immunol. 2018; 54(1):1–25.
- Walker A, Favreau T. Localized pemphigus foliaceus. Cutis. 2017; 99(1):E23–E26.
- Tang HKC, Lee DYH, Thompson I, et al. Delayed and localized pemphigus vulgaris after breast cancer radiotherapy. Breast J. 2017;23(6):747–749.
- Dreyer S, Aleshin M, Young L. Bullous pemphigoid localized in a primarily hemiplegic distribution. JAAD Case Rep. 2017;3(2):113–115.
- Shi CR, Charrow A, Granter SR, et al. Unilateral, localized bullous pemphigoid in a patient with chronic venous stasis. JAAD Case Rep. 2018;4(2):162–164.
- Ruocco E, Russo T, Piccolo V, et al. Unilateral bullous pemphigoid in a patient with a previous ipsilateral cerebellar hemorrhage. Int J Dermatol. 2014; 53: e344–e346.

