 J Clin Aesthet Dermatol. 2022;15(4):36–38.
J Clin Aesthet Dermatol. 2022;15(4):36–38.
by Giulio Gualdi, MD; Manfredo Bruni, MD; Federica Giuliani, MD; Paolo Gisondi, MD; and Paolo Amerio, MD
Drs. Gualdi, Giuliani and Amerio are with the Dermatologic Clinic, Department of Medicine and Aging Science, at University D’Annunzio Chieti-Pescara in Chieti, Italy. Dr. Bruni and Prof. Gisondi are with the Department of Medicine, Section of Dermatology and Venereology, at the University of Verona in Verona, Italy.
FUNDING: No funding was provided for this article.
DISCLOSURES: There are no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Epidermal barrier defects have been described in psoriatic lesions. Transepidermal water loss (TEWL) is the measure of steady-state water vapor flux crossing the skin to the external environment, and it has been used extensively to characterize skin barrier function. We evaluated how biological treatments impact TEWL in with psocratic patients.
Methods. TEWL measurements were collected from psoriatic lesions and from adjacent unaffected skin areas before introducing a biological anti-tumor necrosis factor (TNF) alpha treatment and after six months of therapy.
Results. Our data show that the skin barrier function is restored after biologic therapy. Analysis of healthy skin values, indicated significant increases in TEWL.
Conclusion. A restoration of TEWL on psoriatic lesions was coupled with an alteration of this parameter in nonlesional skin of all patients, underscoring the general homeostatic effect of an anti-TNF on the integrity of skin barrier. These results suggest the need of an emollient therapy in patients with psoriasis undergoing systemic biological treatment.
Keywords. TEWL, Psoriasis, Biologics, TNF-alpha, Epidermal barrier
Psoriasis vulgaris is a chronic immune-mediated disorder, stemming from a combination of environmental factors and genetic susceptibility. Psoriasis affects 1 to 3 percent of the world population. Its association with other inflammatory disorders, such as psoriatic arthritis, inflammatory bowel disease, and coronary artery disease, is well known.1 Psoriasis may have a great impact on patients quality of life due to symptoms (such as pruritus) and psychological distress.2 The interplay of innate and adaptive immunity with epidermal keratinocytes is central in the pathogenesis of psoriasis.3 An approximate function of the epidermal barrier necessitates a set of complex interactions between genetic and immunological factors regulating the expression of proteins and enzymes controlling lipid metabolism required for appropriate skin function. The permeability barrier of the skin resides largely in the stratum corneum (SC), which depends upon a two-compartment system —corneocytes (cellular) and lipid-rich matrix (intercellular). Given the nature of psoriasis pathogenesis, it is not surprising that epidermal barrier defects have been linked in psoriatic lesions.4 The main changes reported in psoriatic skin are a reduction of ceramide levels and an alteration of the quality and composition of ceramide species.5 Changes in the extracellular matrix lipid quantity and quality have been described as well, with the levels of sphingosine markedly elevated in psoriatic lesional skin.4 A modification of cholesterol and fatty acid levels was also observed in psoriatic lesions as well as a modification of the cornified lipid envelope (LCE) structure and its components.6 Transepidermal water loss (TEWL) is a measure of the steady-state water vapor flux crossing the skin to the external environment, and it has been used extensively to characterize skin barrier function. TEWL is directly related to the reciprocal of the diffusional permeation path length through the SC.7 TEWL is significantly increased in psoriasis, and its increment is direcly dependent on the severity of the lesions. Moreover, topical treatments have been shown to restore TEWL in patients with psoriasis.8 We assessed the effects of etanercept, an anti-tumor necrosis factor-alpha (TNF-alpha) biological therapy on TEWL in psoriasis lesional and non-lesional skin.
Methods
Ten patients affected by chronic moderate plaque psoriasis and 35 voluntary healthy subjects acting as control group were enrolled in the study. The control group was recruited from patients attending the clinic for noninflammatory skin conditions; none of the patients in the control group had a family history positive for psoriasis. Patients in the study group were all eligible for biological therapy and were treated with etanercept. Patients with psoriasis conditions that could alter skin barrier Function such as advanced renal or liver disease, erythrodermia, or psoriasis covering a body surface area (BSA) greater than 50 percent were excluded from the study.
From each patient in the case group, TEWL measurements were collected on a target psoriatic lesion on the upper limbs and on an adjacent clinically unaffected skin area (4cm away from the target lesion). This procedure was performed before the treatment and after a six-month period. Measurements in the control group were taken from the distal part of the forearm surface. Measurements guidelines for TEWL were followed. Measures were assessed using the SkinLab Combo DermaLab® evaporator (Cortex Technology, Denmark) at the same environmental conditions, (temperature of 21± 2.6 ° C and humidity of 41.3±10.7%). To standardize data, measurements were performed by the same operator, and all patients were allowed to acclimatize for 15 to 20 minutes in the room before proceding with testing. Windows and doors were closed and the ventilation systems were turned off to reduce air convection which can alter open chamber systems. To reduce intradaily TEWL variability, all measurements were made at the same time in the morning. In all subjects, three TEWL measurements were performed per site, and, the average of the three values was used.
Photographic images was collected after obtaining the patients consent to exactly identify the site to be tested before and after therapy. For all patients, Psoriasis Are Severity Index (PASI) values were collected. All subjects gave written informed consent, and that the study protocol was approved by the institute’s committee on human research.
Results
There were 10 patients (5 male; 5 female; mean age 53.7±7.85 years) in the active treatment group. There were 30 patients (15 male; 15 female; mean age 46.14 ± 4.22 years) in the control group)
The mean TEWL measurement was higher in the active treatment group before the treatment compared to the control group. Among the treatment group, TEWL mean values were higher on lesional skin compared to nonlesional skin. (Figure 1).
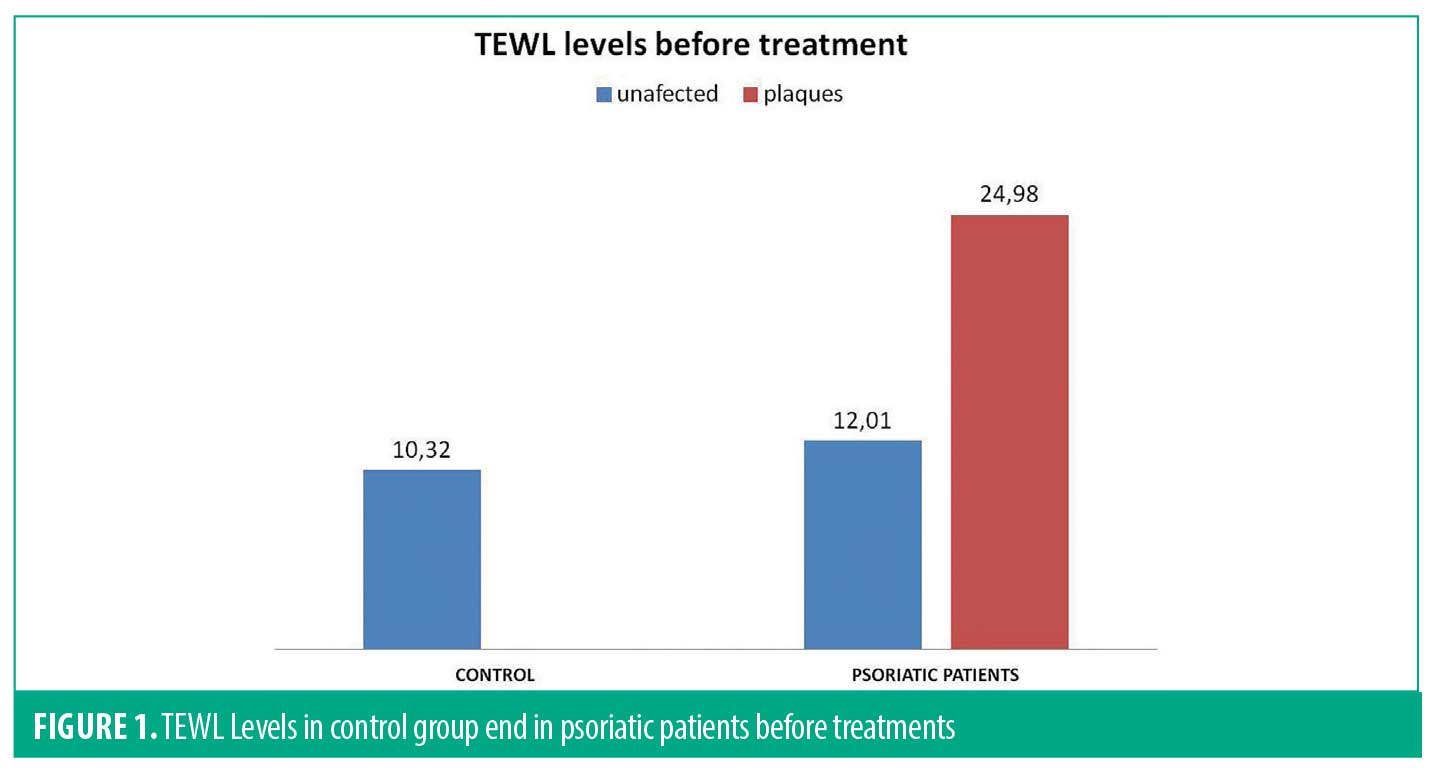
The TEWL values in patients with psoriasis of uninvolved skin before treatment did not show significant differences if compared to the samples collected from the control group.
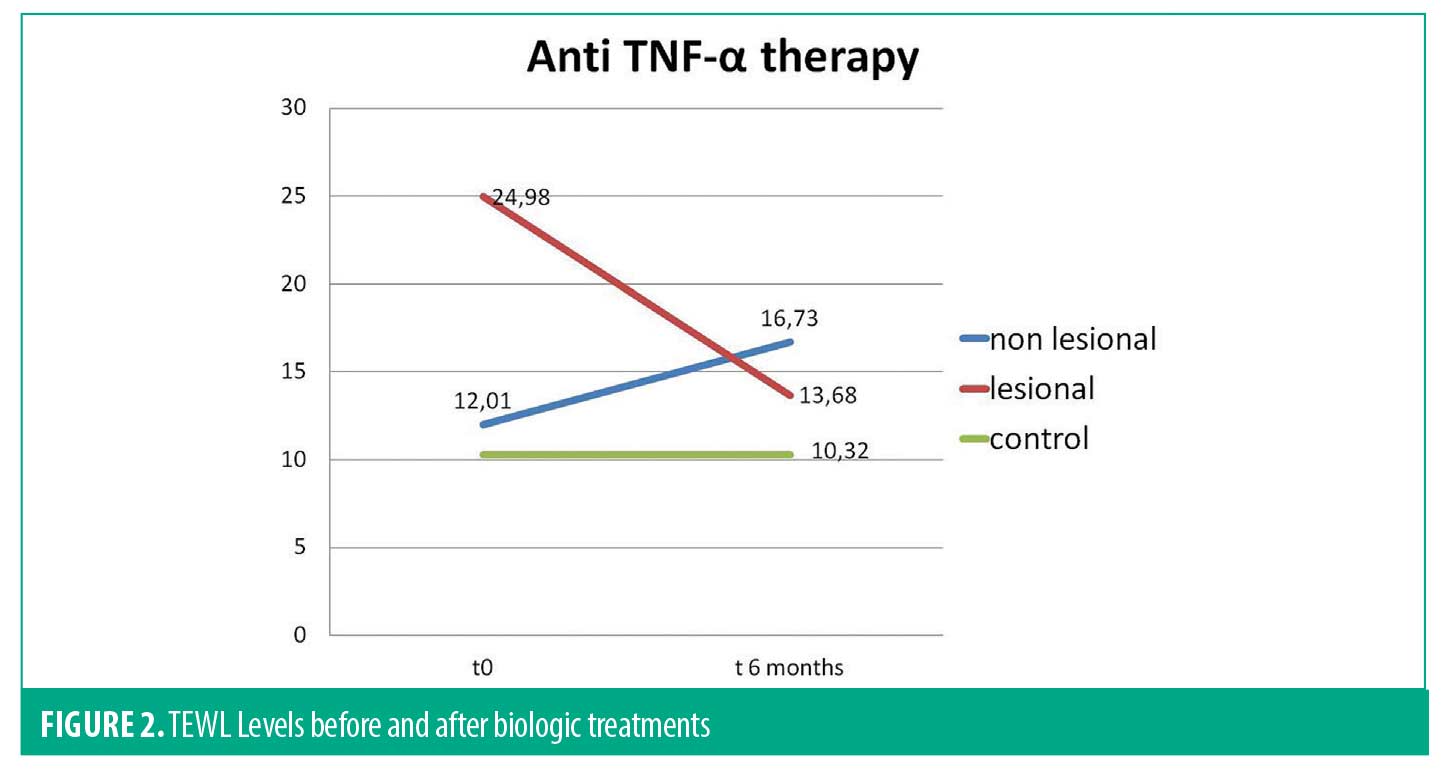
After biological anti-TNF-alpha treatment, mean TEWL value was reduced with an average of 16.75±4.75g/m²/ h becoming closer to the on observed in healthy subjects. We concomitantly recorded an elevation of TEWL values in uninvolved skin of psoriasis patients to 16.73±5, 21 (Figure 2).
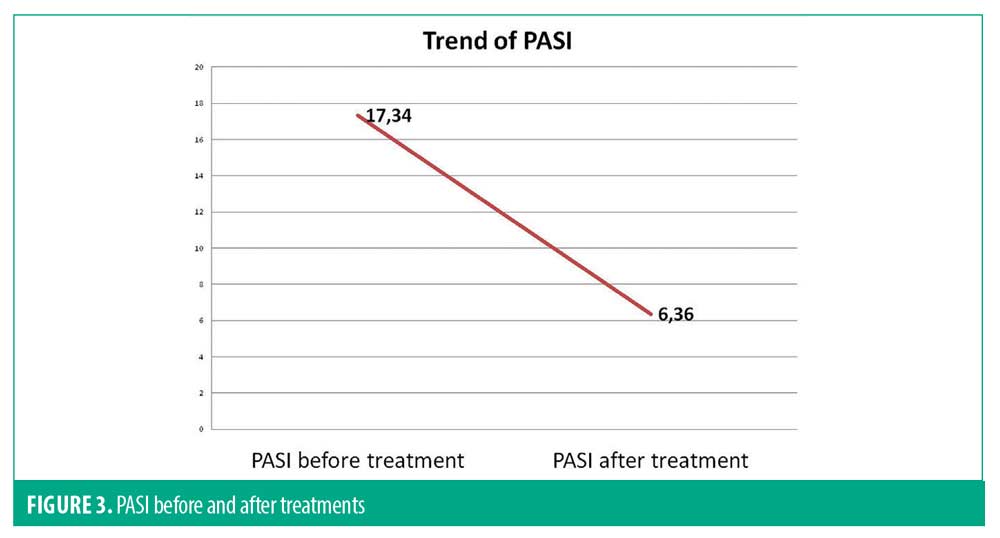
PASI of all patients significantly decreased after treatment, from an average of 17.34 to 6.36. (Figure 3).
Conclusion
Psoriasis pathogenetic hypothesis has changed in the last decades from a keratinocyte centred disease to an immune-mediated disease. However, the complex interplay of keratinocytes with immune cells and the evidence that keratinocytes play an important function in the innate immune system suggests they play an important role in psoriasis. Keratinocytes are an important part of the skin barrier, and there is evidence of a skin barrier defect in patients with psoriasis.
Psoriasis harbours a defective late cornified envelope (LCE)6 and alterated fatty acid, ceramides, and extracellular lipids quantity and quality.5 Skin barrier alteration leads to defects of skin permeability which can be measured through transcutaneous water loss (TEWL). In our study we have evaluated, for the first time, TEWL modifications on psoriatic plaques and on uninvolved skin before and after biological systemic treatment with etanercept.
We found a significative difference in TEWL measurements between lesional skin, nonlesional skin, and skin from healthy subjects. We also showed that nonlesional skin from patients with psoriasis presents values similar to skin of healthy individuals.
As expected, after biological treatment in patients with psoriasis, there was an improvement of PASI. TEWL values also improved as it has been already reported for other topical and physical therapies.8 However, we unexpectedly recorded a deterioration of the skin barrier of nonlesional skin from patients with psoriasis. Although not statistically significant, this trend has been confirmed for all patients.
We think that this can be considered strictly linked to the mechanism of action of etanercept on uninvolved skin. It has been demonstated, in fact, that TNF-alphja plays a physiological role in skin-related processes, such as keratinocytes differentiation, in particular for an efficient formation of cornified envelope development,9 and is important in the recovery of barrier integrity in animal models.10 TNF-alpha is capable of inhibiting the expression of filaggrin and loricrin, leading to a weakened skin barrier function.10
We hypothesize that TEWL values in psoriatic plaques decrease mainly due to reduction in TNF-alpha, but at the same time, the drug may act also in noninvolved skin, leading to an unwanted alteration of skin barrier permeability. For this reason, a more rational management of the patient with psoriasis treated with anti-TNFs-alpha suggests the strong need and the importance of a concomitant emolient treatment on complete body surface.
References
- Burden DA, Kirby B. Psoriasis and related disorders. 142 In: Griffiths C,Barker J, Bleikar T, Chaimers R, Creamer D, editors. Rook’s Textbook of Dermatology. 9th ed. West Sussex: Wiley Blackwell; 2016. pp. 35–1
- Ciuluvica C, Fulcheri M, Amerio P. Expressive Suppression and Negative Affect, Pathways o. Emotional Dysregulation in Psoriasis Patients.Front Psychol,10, 1907 2019 Aug 21 eCollection
- Nestle F.O.,Kaplan D.H.,Barker J:Psoriasis N.Engl. J. Med. 2009; 361:496–509
- Motta S, Monti M, Sesana S, et al.Abnormality in water barrier function in psoriasis: role of ceramide fraction Arch Dermatol Res1994;130:452–6.
- Lew, BL, Cho, Y, Kim, J, et al. Ceramides and cell signaling molecules in psoriatic epidermis: Reduced levels of ceramides, PKC155 alpha and JNK. J. Korean Med. Sci. 2006, 21, 95–99.
- JM Jensen, E Proksch. The Skin’s Barrier. G Ital Dermatol Venereol. 2009;144(6):689–700.
- Machado M, Salgado TM, Hadgraft J, et al. The relationship between transepidermal water loss and skin permeability. Int Pharmaceutics. 2010;384:73–7
- Brazzelli V, Barbagallo T, Prestinari F, et al. Non-Invasive Evaluation Of Tacalcitol Plus PUVA Versus Tacalcitol Plus UVB-NB In the Treatment Of Psoriasis “RIGHTLEFT INTRA164 INDIVIDUAL – PRE/POST COMPARISON DESIGN”. International Journal Of Immunophatology and Pharmacology, 2005:18(4):755–760.
- Jens-Michael Jensen, Stefan Schütze, Michael Förl, et al. Roles for tumor necrosis factor receptor p55 and sphingomyelinase in repairing the cutaneous permeability barrier. J. Clin Invest., 1999: 104, p.1761–1770.
- Ettehadi P, Greaves MW, Wallach D et al. Elevated tumour necrosis factor 171 alpha (TNF-alpha) biological activity in psoriatic skin lesions. Clin Exp Immunol, 1994: 96, p.146–51.

