 by Amy Huang, MD; Arianna Phillips, BS; Tony Adar, MD; and Andrea Hui, MD
by Amy Huang, MD; Arianna Phillips, BS; Tony Adar, MD; and Andrea Hui, MD
Drs. Huang, Adar, and Hui are with the Department of Dermatology at the State University of New York Downstate Medical Center in Brooklyn, New York. Ms. Phillips and Dr. Hui are with Bay Area Cosmetic Dermatology in San Francisco, California.
Funding: No funding was provided for this article.
Disclosures: The authors have no conflicts of interest to relevant to the content of this article.
Abstract: Background. The eye is a vulnerable and commonly injured organ in cosmetic laser procedures of the face. Treatment of the eyelids and periorbital areas increases this risk, especially when ocular protection devices are not used or are removed during the procedure. A study has shown that injury from laser epilation of the periocular areas is one of the most common causes of litigation in cutaneous laser surgery.
Objective. The goal of this review is to determine the causes of ocular injury in cosmetic laser procedures and derive lessons on critical safety elements to prevent future injury.
Methods. We conducted a review of the current literature through a PubMed search on case reports of ocular injury in cosmetic laser treatments of the face. Twenty-one cases are examined. Results. In more than 62 percent of cases, ocular protection was not used or protection was used but removed during the procedure to treat areas close to the eye. However, despite the proper use of intraocular corneal shields and wavelength-specific goggles, accidents occurred in 33 percent of cases.
Conclusion. Ocular protection devices are essential to prevent most cases of laser-induced eye injury. Use of high fluence and long wavelength lasers increases the risk of ocular injury due to deeper penetration of the organ by radiation. Inadequate cooling between pulses also predisposes to injury by cosmetic lasers.
Keywords: Lasers, injury, cosmetic, safety, periorbital, eyelid, laser hair removal, resurfacing
J Clin Aesthet Dermatol. 2018;11(2):15–18
Introduction
Lasers have been used in dermatology for over 50 years. Specific to cutaneous lasers, the technique of selective photothermolysis damages a specific target, such as a blood vessel, while sparing surrounding tissue. Three essential requirements must be met in cases of selective photothermolysis: 1) a wavelength that penetrates deeply enough and is preferentially absorbed by the chromophore or target, 2) an exposure duration (pulse width and pulse duration) less than or equal to the thermal relaxation time (TRT) of the target, and 3) sufficient energy (fluence) to cause irreversible damage to the target.1 In the treatment of vascular lesions, target vessel damage by heated oxyhemoglobin yields vascular injury, which includes coagulation, perivascular collagen damage, and vessel wall necrosis with minimal damage to surrounding epidermis, capillaries, and dermal tissue.2 Selective photothermolysis allows clinicians and trained aestheticians to treat pigmented and vascular lesions, perform facial resurfacing, and remove hair in select areas.
Although one report was clearly against periocular use of lasers, in practice, laser treatments are frequently performed in the eyelid and periocular regions, especially in laser epilation.3 The eyes are susceptible to injury due to the thinner eyelid skin. In addition, there are several pigment-rich chromophores, such as retinal pigment epithelium and the iris, that can also absorb laser energy.4 Previous research shows that melanin in the retinal pigment epithelium absorbs more energy at shorter wavelengths than at longer wavelengths.5 Due to this anatomical limitation, precautions must be taken when treating periorbital areas to decrease the risk of thermal injury and blindness. Patients who are not given ocular protection devices, such as wavelength-specific goggles or spectacles, are often instructed to close their eyes during laser treatment of periorbital areas. However, the eyelids are too thin to sufficiently protect the eye from injury.5 In addition, Bell’s phenomenon, when the eyes naturally roll upwards upon eyelid closure, can cause the pigmented iris to enter the laser’s penetration range and absorb the incident radiation, leading to injury of the iris and posterior structures.6 Patients with light-colored eyes are especially prone to injury in the posterior eye structures, as the pigmented retinal epithelium, and not the iris, tends to absorb the incident radiation.6
Laser Injuries of the Eye
Mechanisms of injury. Short wavelength lasers, such as potassium titanyl phosphate (KTP) and pulsed dye (PDL) lasers, produce photocoagulation (photothermal) damage, while long wavelength, infrared, and near-infrared lasers (e.g., diode, Nd:YAG lasers) produce either photodisruption (photomechanical) or photocoagulation damage.7 In photocoagulation, the tissue generates enough heat to denature proteins, and increases in retinal temperature of 40°C to 60°C can be observed.5 In photodisruption, an explosive acoustic shock is generated that shears, fragments, and perforates tissue.
Clinically, the 1064nm Nd:YAG laser, which is implicated in the majority of laser-induced ocular injuries, is capable of causing retinal hemorrhage, vitreous hemorrhage, scarring, preretinal membrane formation, and retinopathy when the radiation is absorbed by the melanin-rich retinal pigment epithelium.5 The Nd:YAG laser can cause significant injury to the eye and surrounding skin, compared to shorter wavelength lasers, because it can penetrate deeper layers of the skin. Longer wavelength lasers (e.g., 755–795nm alexandrite to 1064nm Nd:YAG lasers) also tend to be weakly visible, compared to the highly visible, shorter-wavelength lasers (e.g., KTP laser), and can pose a hazard when the beam goes unnoticed.8 Various mathematical prediction models have been created to predict the temperature distribution in laser radiation of the human eye to evaluate the risk of ocular damage by lasers.9–12
Components of the eye injured by lasers. Various parts of the eye can be injured by lasers, and the damage can be minor to severe. Minor thermal injury to the cornea results in severe pain, as the cornea has a high density of pain receptors.13 However, corneal injury seldom produces significant vision impairment when confined to the corneal epithelium.14 When injured, the lens and retina are two components that can significantly impact organ function. Injury to the lens can lead to decreased vision in the affected eye through cataract formation. The retina, which is responsible for converting light stimuli into a visual image in the brain, is particularly vulnerable to lasers in the visible to near-infrared spectrum (400nm–1400nm), known as the retinal hazard region.7 Light in this spectrum is focused by the lens onto the retina, leading to 105 times greater retinal irradiance than corneal irradiance.15 As many of the lasers used in dermatology fall within this spectrum, caution should be undertaken when operating cosmetic lasers, especially on the upper face.
Reports in the literature. As cosmetic laser procedures of the face have become more popular in the past decade, there has been an increase in the number of reported injuries to the eye. The most highly reported injury stems from laser hair removal of the periorbital areas.3, 6,16–22 Commonly used lasers for this procedure include the 755nm alexandrite and various diode (800–983nm) lasers. All are long wavelength lasers that are capable of causing severe injury to the eye. In fact, from 1985 to 2012, one study found that laser hair removal was the most common litigated procedure in cutaneous laser surgery, with four reported claims of eye injury.23 For other cosmetic treatments of the face, laser injury to the eye was reported during the treatment of periorbital vascular lesions,24 laser skin resurfacing,25 and other unspecified cosmetic procedures.7,26,27 Eye injury from facial treatment by intense pulse light (IPL) has also been reported.28
In the 21 case reports analyzed from the literature (PubMed), the patients experienced a variety of ocular injury, including iris atrophy, cataracts, anterior uveitis, glaucoma, visual field defects, posterior synechiae, and pupillary defects (Table 1). In all cases, ocular injuries were immediately apparent after treatment with the laser. Common immediate signs and symptoms included severe eye pain, temporary loss of vision, and conjunctival erythema. In 13 of the 21 (62%) case reports examined in this review, proper eye protection was either not provided to the patient or the patient was asked to remove the protection device during the procedure to treat areas near the eye that could not be reached over the shield. This highlights the critical need for clinicians and aestheticians to provide proper eye protection to patients when treating the face, and for them to ensure that such devices stay on the eyes for the duration of treatment.
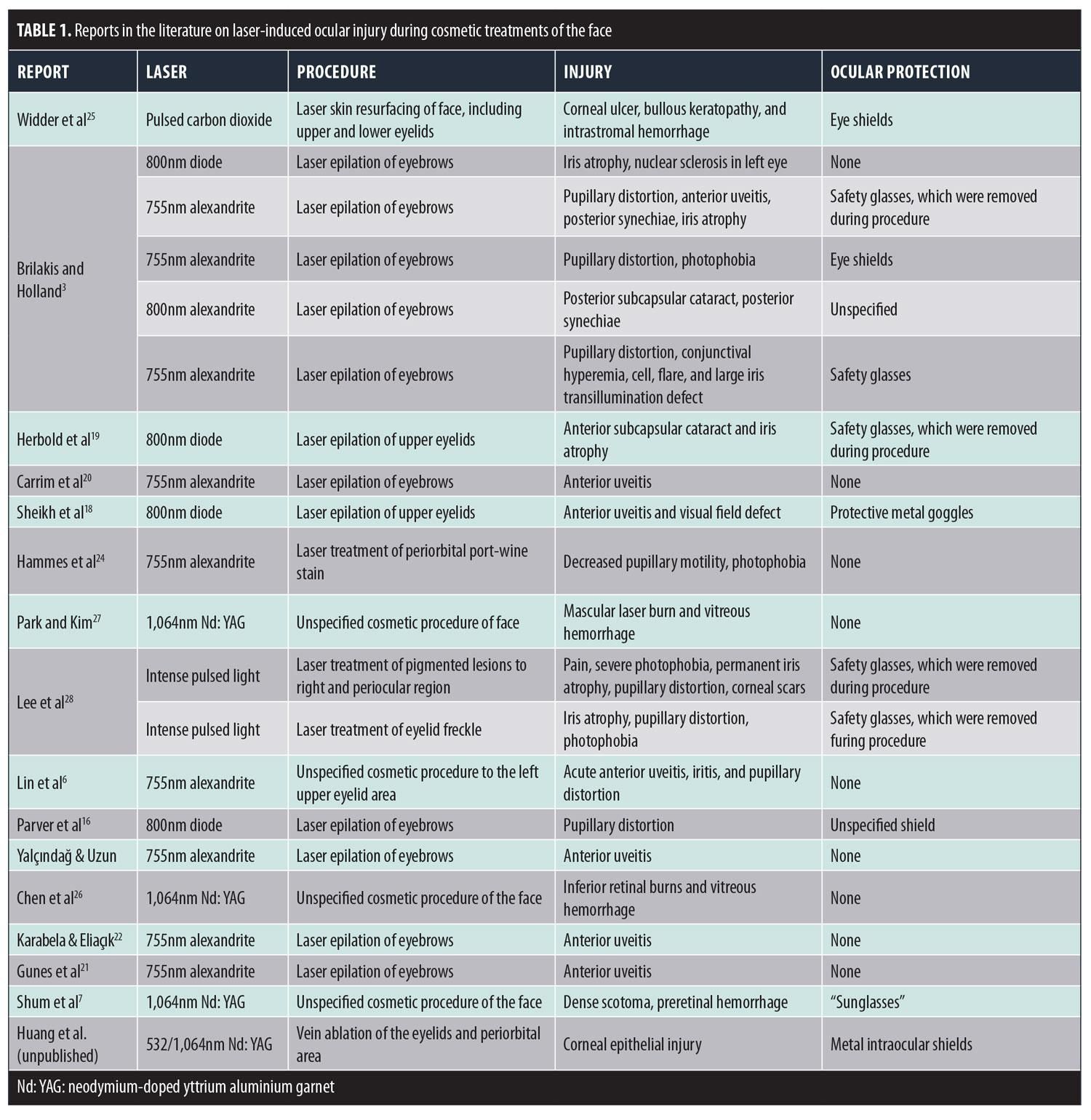
However, ocular protection devices are not fail-safe. In 33 percent of cases in which eye protection was provided,16,25 such as metal corneal shields and wavelength-specific glasses, severe injury to the eye also occurred, including bilateral bullous keratopathy in a patient who underwent carbon dioxide laser facial resurfacing.25 Mechanism of injury was likely due to overheating of the metal corneal shields during the long procedure and inadequate cooling between laser pulses.25
Ocular Protection and Laser Safety Mechanisms
Laser goggles and eyewear. Different safety measures ensure that the eye and other vulnerable parts of the body are protected from injury by lasers. One of the most basic eye protections is the use of wavelength-specific goggles or spectacles during procedures. In one study of 40 patients with ocular injury, only six (15%) patients were wearing protective eyewear during the use of lasers; five of the six were not wearing proper wavelength-specific eyewear.14 Eyewear should be snugly fitting and comfortable, and should not be removed during treatment, especially during laser alignment. For treatments involving Nd:YAG lasers, it is possible for laser radiation to be reflected back from shiny mucosal surfaces into the observer’s eye, potentially causing injury to the user.29 Thus, eye protection is also essential for observers and operating personnel.
Corneal eye shields. Corneal eye shields, made of various colors and materials, are designed to fit directly on the patient’s eyes, just like contact lenses. When treating the areas around the eyes, laser-impenetrable metal ocular shields must be worn for the duration of treatment. The recommended corneal shields fit behind the eyelids, as they are less likely to shift during treatment.30 There are many types of metal corneal shields available, including the Cox II shield (Oculo-Plastik; Montreal, Canada), the Stefanovsky shield (Bernsco; Seattle, Washington), and the Khan shield (Storz; St. Louis, Missouri). The Cox shield is thinner than the Stefanovsky shield, leading to higher temperature changes on laser pulses that can cause thermal injury of the cornea at higher fluences and longer wavelengths due to heat conduction on the underlying tissues.31 This might be the mechanism of injury in reports of patients who suffered corneal thermal injury after laser treatment, despite intact and properly placed metal corneal shields. We recommend applying one pulse at a time and moving on to a different area, which will allow the treated area to cool sufficiently and prevent heat retention on the thin corneal shields. Cooling gel and ice packs should also be applied to treated areas in between pulses. Metal eye shields can also be irritating to the eye and might leave certain parts of the eye vulnerable, such as the superior conjunctival fornix.32 To prevent injury to this part of the eye, a large metal blade can be placed between the upper eyelid and the globe, then fixed to a toothed clamp, such as the David Baker (Oculo-Plastik) and Khan-Baker (Storz) eyelid clamps, on the upper eyelid.30 Use of these clamps might be uncomfortable to the patient and can cause mild crush injury to the upper eyelid.30
Two studies have examined the safety of corneal eye shields in facial laser treatments. One study found that, when irradiated by a 585nm PDL, the temperature rise at the surface of the shields, whether metal or plastic, was no more than 0.2°C.33 The authors noted that while the metal corneal shield (Stefanovsky) did not allow light transmission or have an appreciable temperature rise, the reflective potential of the metal shield posed a risk to operating personnel. In addition, the rough, sharp edges of the metal shield could potentially cause corneal abrasions in the patient. There has only been one published case of bilateral corneal abrasions from the use of metal eye shields after laser skin resurfacing.34 In a different study, however, all plastic shields melted or caught fire when exposed to radiation by Nd:YAG and carbon dioxide lasers.31,35 Thus, long wavelength lasers could potentially cause severe thermal injury to patients, when using plastic shields.
Cooling devices. Cooling devices integrated into most laser modalities offer a protective mechanism against epidermal injury and pain during laser procedures. Cooling of the epidermis before, during, and after treatment can protect against thermal damage in darker skinned patients, who are more susceptible to dyspigmentation, blistering, scarring, and pain.36 Two types of cooling methods are employed: contact cooling and non-contact cooling. Contact cooling is achieved by either active (copper or sapphire tips) or passive (ice or cold gels) methods, of which cooling by aqueous gels is the least effective and often discouraged method.36 Non-contact cooling is achieved by cold air or cryogen (liquid nitrogen or R-134a) spray. These cooling devices are difficult to maneuver around the eye. Contact cooling is exceedingly difficult to use in the periorbital areas, due to the contours of the eye and difficulty in maintaining constant, complete contact with the skin. Non-contact cooling is also challenging, as the intense blasts of cold air might accidentally injure the eye.
There are currently no studies in the literature that mention the use of cooling devices in cosmetic laser procedures in the periorbital and eyelid areas. However, corneal cooling is occasionally used in ophthalmologic laser procedures to prevent corneal injury. In these procedures, the surgeons irrigate the eye with chilled balanced salt solution either between ablation passes and immediately after the end of ablation or continuously.37, 38 Corneal cooling has been found to prevent ocular injury.39 While corneal cooling by cool water irrigation might not necessarily be practical in cosmetic eyelid procedures, the use of non-contact cooling, together with ocular shields, might be feasible.
Treatment of Ocular Injury
Treatment of the eye after laser injury is largely determined by the extent of injury and can include medical and/or surgical management. Superficial lesions to the corneal epithelium can be treated with topical antibiotics and contact lenses or patching.14 Corneal endothelial injury leading to bullous changes, corneal thickening, or vision loss requires surgical intervention with corneal transplantation. Topical steroids (e.g., methylprednisolone) at varying treatment lengths are also the preferred medical treatment for ocular injury and reduce the damaging inflammatory response to injury.15 Steroid-treated retinas have been shown to have rapid reestablishment of retinal and choroidal vasculature, healing of the retinal pigment epithelium, less macrophage activity, and reduced photoreceptor damage.40,41 Treatment of laser-induced ocular injury can involve a combination of topical antibiotics, topical or systemic steroids, and vitamins, although there are currently no guidelines on dosing and preferred medications. Vitamins include topical and oral ascorbic acid (vitamin C) to promote fibroblast activity.42 All patients with laser-induced eye injuries need to be referred to an ophthalmologist for detailed evaluation.
Conclusion
Lasers are effective modalities for facial cosmetic treatments, but can cause injury to the eye when used periorbitally or on the eyelids. Several safety measures can prevent laser ocular injury. First, the treating physician must be properly trained to operate the laser, and should have basic knowledge in laser physics and safety. Second, lesions around the eye or on the eyelids should not be treated without metal ocular shields or wavelength-specific glasses, including eye protection for operating personnel. Care must be taken to ensure eye protection is not removed or moved, especially during long procedures. Third, frequent and sufficient cooling of the treated areas must be ensured to prevent thermal injury and overheating of the metal corneal shields. And finally, we recommend that only core physicians administer laser treatment to periorbital or eyelid regions (e.g., board-certified dermatologists, plastic surgeons, ophthalmologists, or otolaryngologists with advanced training in cosmetic surgery and medicine). Despite these precautions, laser ocular injury might still occur, though rarely. Superficial injury to the cornea can be treated with topical antibiotics. topical steroids, and contact lens or patching. More severe corneal damage requires corneal transplantation. All patients described in the 21 case reports we reviewed were treated with topical steroids and antibiotics, and some with systemic steroids. Patients should always seek immediate consultation from an ophthalmologist.
References
- Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. 1983;220(4596):524–527.
- Adamic M, Troilius A, Adatto M, et al. Vascular lasers and IPLS: guidelines for care from the European Society for Laser Dermatology (ESLD). J Cosmet Laser Ther. 2007;9(2):113–124.
- Brilakis HS, Holland EJ. Diode-laser-induced cataract and iris atrophy as a complication of eyelid hair removal. Am J Ophthalmol. 2004;137(4):762–763.
- Vukicevic M GT, Keel S. Laser Pointer Retinal Injury: A Case Report. Australian Orthoptic Journal. 2014;46:1.
- Mainster MA, Stuck B, Brown J. Assessment of alleged retinal laser injuries. Arch Ophthalmol. 2004;122(8): 1210–1217.
- Lin CC, Tseng PC, Chen CC, et al. Iritis and pupillary distortion after periorbital cosmetic alexandrite laser. Graefes Arch Clin Exp Ophthalmol. 2011;249(5): 783–785.
- Shum JW, Lu LP, Cheung DN, Wong IY. A case of accidental ocular injury from cosmetic laser burn. Retin Cases Brief Rep. 2016;10(2):115–120.
- Sliney DH. Eye safety of laser and light-based devices. In: Ahluwalia G, editor. Cosmetics Applications of Laser and Light-Based Systems: Elsevier; 2008. p. 506.
- Mirnezami SA, Jafarabadi MR, Abrishami M. Temperature distribution simulation of the human eye exposed to laser radiation. J Lasers Med Sci. 2013;4(4):175–181.
- Shibib KS. Finite element analysis of cornea thermal damage due to pulse incidental far IR laser. Lasers Med Sci. 2013;28(3):871–877.
- Milsom PK, et al. The effect of ocular aberrations on retinal laser damage thresholds in the human eye. Health Phys. 2006;91(1):20–28.
- Heussner N, Vagos M, Spitzer M, et al. A prediction model for ocular damage – experimental validation. J Therm Biol. 2015;52:38-244.
- Sliney DH, Mellerio J, Gabel VP, et al. What is the meaning of threshold in laser injury experiments? implications for human exposure limits. Health Phys. 2002;82(3):335–347.
- Thach AB. Laser injuries of the eye. Int Ophthalmol Clin.1999;39(2):13–27.
- Barkana Y, Belkin M. Laser eye injuries. Surv Ophthalmol. 2000;44(6):459–478.
- Parver DL, Dreher RJ, Kohanim S, et al. Ocular injury after laser hair reduction treatment to the eyebrow. Arch Ophthalmol. 2012;130(10):1330–1334.
- Le Jeune M. Ocular complications after laser epilation of eyebrows. Eur J Dermatol. 2007;17(6):553–554.
- Sheikh A, Hodge W, Koupland S. Diode laser-induced uveitis and visual field defect. Ophthal Plast Reconstr Surg. 2007;23(4):321–323.
- Herbold TM, Busse H, Uhlig CE. Bilateral cataract and corectopia after laser eyebrow [corrected] epilation. Ophthalmology. 2005;112(9):1634–1635.
- Carrim ZI, Chohan AW, Devlin HC. Iris damage and acute pigment dispersion following photo-epilation. Eye (Lond). 2006;20(12):1486–14888.
- Gunes A, Yasar C, Tok L, Tok O. Two cases of anterior uveitis after laser eyebrow epilation. Cornea. 2015;34(1):101–102.
- Karabela Y, Eliacik M. Anterior uveitis following eyebrow epilation with alexandrite laser. Int Med Case Rep J. 2015;8:177–179.
- Jalian HR, Jalian CA, Avram MM. Common causes of injury and legal action in laser surgery. JAMA Dermatol. 2013;149(2):188–193.
- Hammes S, Augustin A, Raulin C, et al. Pupil damage after periorbital laser treatment of a port-wine stain. Arch Dermatol. 2007;143(3):392–394.
- Widder RA, Severin M, Kirchhof B, et al. Corneal injury after carbon dioxide laser skin resurfacing. Am J Ophthalmol. 1998;125(3):392–394.
- Chen SN, Lu CW, Zhou DD. A case of accidental retinal injury by cosmetic laser. Eye (Lond). 2014;28(7): 906–907.
- Park DH, Kim IT. A case of accidental macular injury by Nd: YAG laser and subsequent 6 year follow-up. Korean J Ophthalmol. 2009;23(3):207–209.
- Lee WW, Murdock J, Albini TA, et al. Ocular damage secondary to intense pulse light therapy to the face. Ophthal Plast Reconstr Surg. 2011;27(4):263–265.
- McKenzie AL. Aspects of laser safety in surgery and medicine. J Radiol Prot. 1988;8(4):209–219.
- Biesman BS, Khan JA. Current concepts in aesthetic and reconstructive oculoplastic surgery. Faulkner Clafarr, editor. The Hague: Kugler Publications; 2000.
- Ries WR, Clymer MA, Reinisch L, et al. Laser safety features of eye shields. Lasers Surg Med. 1996;18(3):309–315.
- David LM, Baker SS. David-Baker eyelid retractor. American Journal of Cosmetic Surgery. 1992;9: 141–145.
- Russell SW, Dinehart SM, Davis I, et al. Efficacy of corneal eye shields in protecting patients’ eyes from laser irradiation. Dermatol Surg. 1996;22(7):613–616.
- Litzinger TC, Vastine D. Bilateral corneal opacities in a LASIK patient after the use of titanium eye shields. J Cataract Refract Surg. 2011;37(6):1160–1164.
- Riley J. Safety considerations in the use of the CO2 laser in facial skin resurfacing. Laser Surg Med. 1997;9(Suppl):61.
- Das A, Sarda A, De A. Cooling devices in laser therapy. J Cutan Aesthet Surg. 2016;9(4):215–219.
- Stein HA, Salim AG, Stein RM, et al. Corneal cooling and rehydration during photorefractive keratectomy to reduce postoperative corneal haze. J Refract Surg. 1999;15(2 Suppl):S232–S233.
- Kitazawa Y, Maekawa E, Sasaki S, et al. Cooling effect on excimer laser photorefractive keratectomy. J Cataract Refract Surg. 1999;25(10):1349–1355.
- Kataoka T, Zako M, Takeyama M, et al. Cooling prevents induction of corneal damage by argon laser peripheral iridotomy. Jpn J Ophthalmol. 2007;51(5):317–324.
- Lam TT, Takahashi K, Fu J, et al. Methylprednisolone therapy in laser injury of the retina. Graefes Arch Clin Exp Ophthalmol. 1993;231(12):729–736.
- Takahashi K, Lam TT, Fu J, et al. The effect of high-dose methylprednisolone on laser-induced retinal injury in primates: an electron microscopic study. Graefes Arch Clin Exp Ophthalmol. 1997;235(11): 723–732.
- Scott R. The injured eye. Philos Trans R Soc Lond B Biol Sci. 2011;366(1562):251–260.

