J Clin Aesthet Dermatol. 2018;11(10):12
Dear Editor:
Geographic location can be an important diagnostic factor in determining the cause of allergic contact dermatitis. For example, fragrances might cause dermatitis in persons repeatedly dosed with perfumes (e.g., on the chest, prominentia laryngea, and wrists).1 When allergens are associated with a wash-off product, such as shampoo, wash-line dermatitis can develop.
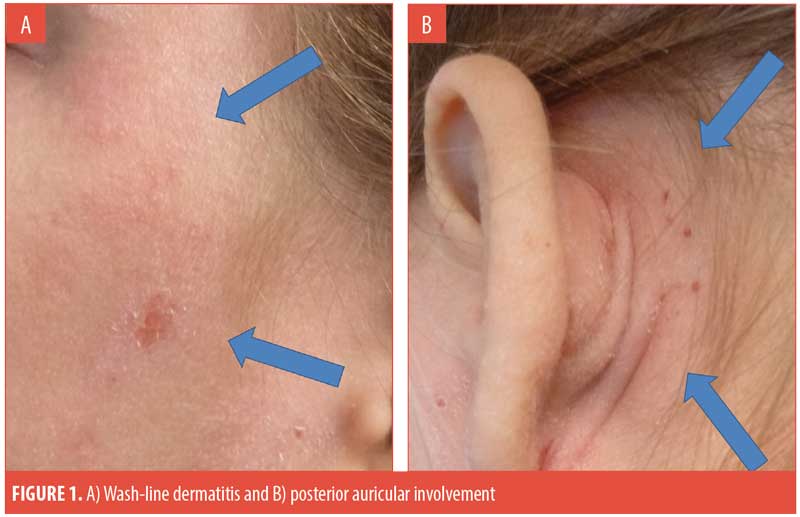
Case report. A 14-year-old girl presented to pediatric dermatology for evaluation of extremely pruritic dermatitis on her face and scalp, which had been present for one year. On examination, she was noted to have well-defined erythematous plaques on her face running parallel with the hairline, in addition to similar plaques with overlying excoriations on her postauricular and posterior neck areas (Figures 1A and 1B). Pertinent negatives on examination included no involvement of the nasolabial folds, knees, or elbows, and no nail pitting. There was no past or family history of seborrhea or psoriasis, she did not play any contact sports, and her family did not have any pets. Notably, the patient was treating her dermatitis with tacrolimus 0.1% ointment and had seen some improvement but continued to experience repeated flares.
She was patch tested using the Thin-Layer Rapid Use (T.R.U.E.) Epicutaneous Patch Test™ (Smart Practice, Phoenix, Arizona), which revealed a 1+ reaction to methylchloroisothiazolinone/ methylisothiazolinone (MCI/MI). In the postpatch evaluation session, the patient noted that she customarily washed her hair by tilting her head backwards in the shower. Importantly, the runoff area of the shampoo corresponded to the area of development of the facial plaques, specifically at the wash-line. Evaluation of the ingredients of the patient’s personal hygiene products revealed the presence of MI in her shampoo. She was instructed to select a shampoo product that was free of her allergens, after which her dermatitis improved.
Discussion. MCI/MI is one of the most common causes of preservative contact allergy and dermatitis.2 It is the active ingredient of a commonly used preservative system consisting of MCI and MI in a 3:1 combination.3 MCI/MI can be found in many cosmetic products, including both rinse-off and leave-on products.4 Cases of contact allergy can be caused by the compound preservative or by MCI and/or MI alone. Although patients are less likely to develop contact dermatitis from rinse-off products, many cases have still been reported.5 Both the American Contact Dermatitis Society Core Series and the T.R.U.E.™ test include the MCI/MI mix. It is important to note that testing with the mix can miss approximately 40 percent of MI allergies, likely due to the low concentration of MI in the MCI/MI combination patch test.3
In patients who have an inadequate response to topical treatment and/or persistent dermatitis, evaluation for contact allergy is warranted. There is a wide spectrum of potential allergens to shampoo ingredients, which presents a significant challenge for patients.6 As allergen avoidance is the treatment of choice for allergic contact dermatitis, identifying shampoo as the exposure source can be a significant asset in designing a treatment regimen and avoidance protocol.
With regards,
Sharon E. Jacob, MD and Shehla Admani, MD
Dr. Jacob is is a Professor of Dermatology in the Dermatology Department at Loma Linda University in Loma Linda, California. Dr. Admani is a Clinical Assistant Professor of Dermatology at Stanford University School of Medicine in Stanford, California.
References
- Jacob SE, Castanedo-Tardan MP. A diagnostic pearl in allergic contact dermatitis to fragrances: the atomizer sign. Cutis. 2008;82(5):317–318.
- Thyssen JP, Engkilde K, Lundov MD, et al. Temporal trends of preservative contact allergy in Denmark (1985–2008). Contact Dermatitis. 2010;62(2): 102–108.
- Castanedo-Tardana MP, Zug KA. Methylisothiazolinone. Dermatitis. 2013;24(1):2–6.
- Biebl KA, Warshaw EM. Allergic contact dermatitis to cosmetics. Dermatol Clin. 2006;24(2):215–232, vii.
- Aerts O, Baeck M, Constandt L, et al. The dramatic increase in the rate of methylisothiazolinone contact allergy in Belgium: a multicentre study. Contact Dermatitis. 2014;71(1):41–48.
- Zirwas M, Moennich J. Shampoos. Dermatitis. 2009;20(2):106–110.

