 by Douglas DiRuggiero, DMSc, MHS, PA-C
by Douglas DiRuggiero, DMSc, MHS, PA-C
Mr. DiRuggiero is with Skin Cancer and Cosmetic Dermatology Center in Rome, Georgia.
J Clin Aesthet Dermatol. 2020;13(9 Suppl):S21–S25
FUNDING: This study was supported by Ortho Dermatologics.
DISCLOSURES: Douglas DiRuggiero is a consultant to Ortho Dermatologics.
ABSTRACT: This case report describes the management of a 64-year-old Hispanic male patient with a 20-year history of severe psoriasis who presented with a worsening of his condition, and topical corticosteroid-induced tinea incognito. The patient was initially treated with systemic and topical antifungals to clear the corticosteroid-induced tinea incognito. He was subsequently treated with broadalumab, an interleukin-17 receptor A antagonist. A combination of oral terbinafine and twice daily ciclopirlox cream to the pruritic lichenified patches on the patient’s neck, upper chest, buttocks, and hip cleared the fungal tinea infection within one month, but well-demarcated plaques remained unchanged on nearly 35 percent of his body. Three weeks of after commencement of broadalumab, the pruritus resolved and the patient’s psoriasis body surface involvement was less than three percent; at four months, it was less than one percent. Conclusion: PAs and NPs working in dermatology should monitor patients on long-term topical corticosteroid therapy to alert them to possible cutaneous complications. Tinea incognito and psoriasis often mimic each other and can occur concomitantly but require different treatment approaches. If tinea incognito is confirmed, topical corticosteroids should be discontinued and it should be treated with antifungals, while, if appropriate, systemic management of the psoriasis with an appropriate biologic may be initiated.
KEYWORDS: Psoriasis, tinea incognito, brodalumab, antifungal therapy, topical corticosteroids
Patients with psoriasis are at increased risk for comorbid skin diseases.1,2 Of those, fungal organisms that colonize and infect keratinizing epithelial structures are among the most prevalent.1,3 Prolonged use of topical corticosteroids in the treatment of psoriasis can suppress the local immune response and result in the atypical iatrogenic dermatophyte presentations referred to as tinea incognito.4–6
CASE REPORT
A new 64-year-old Hispanic male patient with a 20-plus year history of biopsy-confirmed psoriasis presented to the clinic with complaints of intensely pruritic plaques and scale covering nearly 35 percent of his body. He reported that his psoriasis seemed to be “spreading” in certain regions despite adherence with prescribed topical corticosteroids. He had previously been treated in Mexico with multiple high-potency topical corticosteroids, aloe, intramuscular “steroid” injections, and light therapy. More recently, treatments by other United States-based dermatology clinicians included potent topical corticosteroids and vitamin D analog creams. His past medical history was otherwise unremarkable, with no known drug allergies and no other medications.
Physical examination revealed grouped excoriated plaques with surrounding scale on buttocks, hips, lower back, abdomen, upper chest, and neck. Lichenifications with linear excoriations covered the bilateral lower extremities and forearms (Figures 1A–E). Potassium hydroxide (KOH) analysis of skin scrapings from the lower abdomen, buttocks, and upper chest and neck revealed a heavy load of hyphae, confirming the diagnosis of tinea incognito, which was complicating his long-standing psoriasis.

The patient was instructed to discontinue use of all topical steroids and was treated with oral terbinafine 250mg once a day for four weeks and ciclopirlox cream twice daily to neck, upper chest, buttocks, and hip. Using this treatment approach the tinea infection resolved completely within one month; however, well-demarcated plaques and generalized lichenifications remained unchanged on nearly 35 percent of the patient’s body.
Previous long-term steroid exposure, with only intermittent improvement, coupled with disease severity (body surface area [BSA]>30%) and intense widespread pruritus prompted a discussion with the patient regarding biologic therapy. All available biologic treatments were discussed with the patient, including their risks and benefits, and the patient chose to pursue treatment with brodalumab injections (Siliq®, Ortho Dermatologics, Bridgewater, New Jersey). Brodalumab blocks interleukin (IL)-17A, IL-17C, IL-17E (IL-25), and IL-17F via their receptors, which stops the pro-inflammatory cascade that leads to psoriasis. Clinical trials have demonstrated brodalumab’s effectiveness in helping patients attain and retain total clearance.7,8
The patient denied a history of depression and signed the required Risk Evaluation and Mitigation Strategy (REMS) consent form. The insurance approval process was initiated, and the patient was sent for lab work, including complete blood count (CBC), comprehensive metabolic panel (CMP), human immunodeficiency virus (HIV), hepatitis panel, and QuantiFERON Gold.
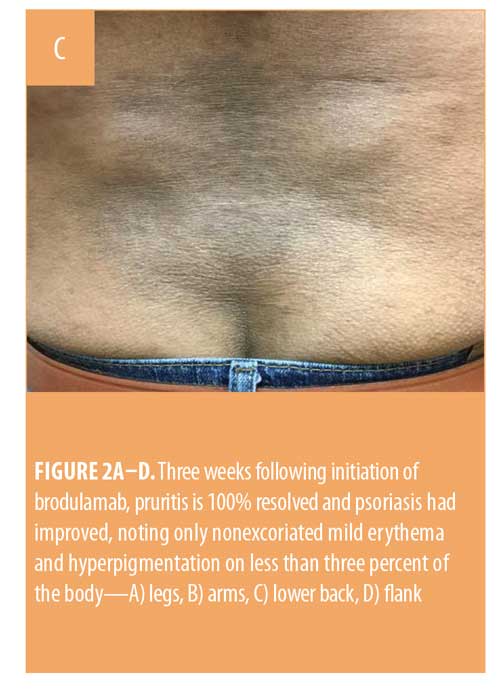
Transportation and communication difficulties delayed initiation of brodalumab treatment for nearly two months. The patient’s initial injection of 210mg was subcutaneously administered in office, and the patient administered the subsequent Week 1 and Week 2 injections at home prior to office follow-up at three weeks. At that time,pruritus was 100-percent resolved, and the patient’s psoriasis was noted as only nonexcoriated mild erythema and hyperpigmentation on less than three percent of the body (Figures 2A–D). He was instructed to self-administer brodalumab every other week and to follow up with the clinic in three months.



At the three-month follow-up visit, the patient, who always appeared proud and stoic at previous visits, greeted the clinician with hugs and tears. The patient reported that after more than 20 years of living with the profound physical and psychological effects of severe psoriasis, he believed that improvement was not possible. However, at this follow-up visit, his skin was free of lesions (Figure 3). Physical exam revealed only limited areas of mild hyper and hypopigmentation, and the patient reported no treatment-related side effects.
Improvement was maintained at the following three-month visit, and the patient was instructed to continue the follow-up visits with the clinic every three months moving forward.


DISCUSSION
When patients with psoriasis present with worsening of generalized psoriatic lesions, intense pruritus, and a history of long-term topical corticosteroid use, concomitant tinea incognito should be considered and a potassium hydroxide (KOH) analysis (or biopsy with periodic acid Schiff [PAS] stain) should be performed. Psoriasis and tinea incognito closely mimic each other in symptomatology, making it easy for other clinicians to miss. Topical corticosteroids can alter the clinical presentation of tinea via anti-in?ammatory actions, which decrease erythema and scaling while allowing the fungus to grow freely without exhibiting the typical clinical signs of tinea. Clinical manifestations of tinea incognito are variable and might resemble rosacea, eczema, lichen, psoriasis, lupus, viral infections, impetigo, and seborrheic dermatitis.1,6, 9–13
The identification of both widespread psoriasis vulgaris and tinea incognito in a patient should alert the clinician for the need of two different types of therapy. In the presented case, antifungals were needed to resolve the tinea incognito, and a switch from topical corticosteroids to a systemic biologic was needed for greater control of his severe psoriasis. Interestingly, after starting systemic therapy, the patient noted improvement in neck, back, hand, and wrist stiffness and overall mobility. Although he had not reported joint symptoms during his initial visit, and brodalumab is not approved for psoriatic arthritis, there appears to have been concomitant benefit from the use of this IL-17R inhibitor, as the patient reported that his back, hand, and wrist joints felt “better and younger” during the follow-up. This is consistent with the results reported in other studies.14,15
Dermatology healthcare providers should monitor patients on long-term topical corticosteroid therapy to prevent possible cutaneous complications. Misdiagnoses or delayed diagnoses of tinea can represent a practical, epidemiologic problem that might lead to associated morbidity for the patient.16
References
- Alteras I, Ingberg A, Segal R, et al. The incidence of skin manifestations by dermatophytes in patients with psoriasis. Mycopathologia. 1986;95(1):37–39.
- Zander N, Schäfer I, Radtke M, et al. Dermatological comorbidity in psoriasis: results from a large-scale cohort of employees. Arch Dermatol Res. 2017;309, 349–356.
- Klaassen KMG, Dulak MG, van de Kerkhof PCM, Pasch MC. The prevalence of onychomycosis in psoriatic patients: a systematic review. J Eur Acad Dermatol Venereol. 2014;28:533–541.
- Crawford KM, Bostrom P, Russ B, Boyd J. Pimecrolimus-induced tinea incognito. Skinmed. 2004;3:352–353.
- Siddaiah N, Erickson Q, Miller G, Elston DM. Tacrolimus-induced tinea incognito. Cutis. 2004;73:237–238
- Kim WJ, Kim TW, Mun JH, et al. Tinea incognito in Korea and its risk factors: nine-year multicenter survey. J Korean Med Sci. 2013;28:145–151.
- Papp KA, Reich K, Paul C, et al. A prospective phase III, randomized, double-blind, placebo-controlled study of brodalumab in patients with moderate-to-severe plaque psoriasis. Br J Dermatol. 2016;175(2):273–286.
- Lebwohl M, Strober B, Menter A, et al. Phase 3 studies comparing brodalumab with ustekinumab in psoriasis. N Engl J Med. 2015;373(14):1318–1328.
- Aste N, Pau M, Aste N, Atzori L. Tinea corporis mimicking herpes zoster. Mycoses.
2011;54:463–465. - Nicola A, Laura A, Natalia A, Monica P. A 20-year survey of tinea faciei. Mycoses. 2010;53:504–508.
- Gorani A, Schiera A, Oriani A. Case report. Rosacea-like tinea incognito. Mycoses. 2002;45:135–137.
- Serarslan G. Pustular psoriasis-like tinea incognito due to Trichophyton rubrum. Mycoses. 2007;50:523–524.
- Meymandi S, Wiseman MC, Crawford RI. Tinea faciei mimicking cutaneous lupus erythematosus: a histopathologic case report. J Am Acad Dermatol. 2003;48:S7–S8.
- Thomas LW, Lee EB, Wu JJ. Systematic review of anti-drug antibodies of IL-17 inhibitors for psoriasis. J Dermatolog Treat. 2018:1–7.
- Mease PJ, Genovese MC, Greenwald MW, et al. Brodalumab, an anti-IL17ra monoclonal antibody, in psoriatic arthritis. N Engl J Med. 2014;370(24):2295–2306.
- Jankovic A, Binic I, Gligorijevi? J, et al. Mimicking each other: Psoriasis with tinea incognito. Dermatologica Sinic. 2011;29:
149–150.

