 by Carolyn I. Jacob, MD, FAAD, and Brittany Rank, PA-C
by Carolyn I. Jacob, MD, FAAD, and Brittany Rank, PA-C
Dr. Jacob and Ms. Rank are with Chicago Cosmetic Surgery and Dermatology in Chicago, Illinois.
J Clin Aesthet Dermatol. 2020;13(4 Suppl):S16–S20
FUNDING: No funding was provided for the preparation of this article.
DISCLOSURES: Carolyn Jacob, MD, FAAD, speaks for BTL on medical congresses.
Objective: High-intensity focused electromagnetic (HIFEM) technology offers an alternative to surgical procedures in terms of correction of altered body shape. In this pilot study, we investigated whether HIFEM technology can positively affect abdominal appearance in postpartum women. Methods: Ten women (3–36 months postpartum; average age: 37.7 years) received four 30-minute abdominal HIFEM treatments. Magnetic resonance imaging (MRI) examination of abdominal fat thickness, rectus abdominis thickness, and the width of abdominal separation was performed and evaluated at baseline, one month, three months, and six months post-treatment. Additionally, weight was recorded, standardized photographs were taken, and patient comfort levels with the procedures were assessed, using a 7-point scale, at these same time points. The paired t-test was used to statistically analyze the mean differences between the baseline and post-treatment data. Results: Results obtained from MRI images showed an average abdominal fat reduction of 17.0 percent at the one-month follow-up visit, while at the three-month follow-up, it was 20.2 percent. The average muscle thickness increase at the one-month follow-up was 20.5 percent, and at the three-month follow-up, it was 21.3 percent. The distance between the rectus abdominis muscles was reduced by 16.7 percent at the first follow-up visit and by 22.7 percent at three-month follow-up visit. The nine subjects who attended the six-month visit showed, on average, a 17.6-percent fat reduction, 21.7-percent increase in muscle, and a 23.2-percent reduction of abdominal separation.Weight did not change significantly. Conclusion: HIFEM treatments appeared to reduce the fat layer and width of abdominal separation, while increasing the thickness of abdominal muscle thickness in postpartum women. The observed results at one month post-procedure were improved at three months post-procedure and remained stable at the six-month follow-up visit. Future studies that include a control or sham group are needed to identify and reduce the risk of bias.
KEYWORDS: EmsculptTM, HIFEM treatment, postpartum, body shaping
Pregnancy and childbirth are inevitably associated with changes in a woman’s body shape and size, which can lead to dissatisfaction with body appearance and a negative perception of body image for many women.1,2 In addition to stretch marks, increased body weight, and worsened breast shape after childbirth and breastfeeding, women predominantly report their stomach as one of the main distressing body areas after child birth.3
During pregnancy, the abdominal muscles are stretched and separated extensively to accommodate the growing fetus.4 However, the abdominis muscles often do not completely return to their original position and can remain separated after childbirth. In severe cases, the separation exceeds 2.7cm, and this condition—known as diastasis recti—is associated with a lack of abdominal tightness and pronounced abdominal laxity.5
The most popular solution to diastasis recti is abdominoplasty, also known as a tummy tuck, which was among the top four cosmetic surgical procedures in 2018, with more than 130,000 surgeries performed in the United States (US).6 Abdominoplasty is a 2- to 5-hour long procedure and is associated with 2 to 4 weeks of downtime.6 However, noninvasive alternatives offering correction of abdominal separation and restoring the abdominal tightness have been lacking.
Recently, Kinney et al7 and Kent et al8 reported a reduction in abdominal separation (10.0%), an increase in the thickness of rectus abdominis (15.1%), and reduction in abdominal fat (18.1%) after a noninvasive high-intensity focused electromagnetic (HIFEM) procedure. HIFEM technology induces a rapidly changing magnetic field that triggers supramaximal muscle contractions, not achievable voluntarily. In response, the muscles grow and strengthen, which lead to a tighter abdomen. Also, the muscle load triggers metabolic responses, leading to the reduction of subcutaneous fat.9
We hypothesized that parous women might benefit from the positive effects of HIFEM while avoiding the risks and downtime associated with surgical abdominoplasty. The fat reduction and muscle thickening observed using this procedure might help reverse the negative body image perception that women can experience after pregnancy.
This pilot study assessed the abdominal separation, abdominal fat, and muscle thickness effects, as well as patient comfort levels, of the HIFEM procedure in a group of postpartum women.
MATERIALS AND METHODS
Inclusion criteria for participation in this pilot study was 1) female sex, 2) giving birth to a baby 6 to 36 months prior to study, 3) being at least 22 years of age, 4) maintaining stable weight (±5lb fluctuation) for at least a month before the study, and 5) having a body mass index (BMI) range less than 30kg/m2. Exclusion criteria included 1) being pregnant, 2) having metal implants, 3) having a heart disorder or any medical condition contraindicating the application of an electromagnetic field, or 4) undergoing active cancer.
Ten women met study criteria and were enrolled in the study, with an average age of 37.7±2.7 years, body weight of 60.0±8.1kg, and BMI of 22.9±2.5kg/m2. Before treatments, the subjects received oral instructions regarding the study, after which they signed an informed consent form. The treatment protocol was approved by the Institutional Review Board (IRB) and conformed to the ethical guidelines of the 1975 Declaration of Helsinki.
The protocol included four 30-minute treatments delivered twice a week for two weeks with an HIFEM technology device (Emsculpt, BTL Industries Inc., Boston, Massachusetts). The treatment was administered on the abdomen of each participant while lying in a supine position. Where the patient size allowed, two applicators were used for treatments. Otherwise, a single applicator was placed over the umbilicus. The device intensity was initially set to 15 to 20 percent, and the applicator placement was adjusted to induce the strongest and most consistent muscle response across the abdomen. The intensity was gradually increased to induce strong, but not painful, muscle contractions.
The patients were evaluated at baseline, one month, three months, and six months post-treatment. The evaluation methodologies included magnetic resonance imaging (MRI) and weight measurements. The patients were also asked to rate, on a scale of 1 to 7 (1= strongly disagree; 7=strongly agree), their level of comfort during the treatments, based on the question: “I found the treatments comfortable.”
The MRI scans were used to evaluate changes in abdominal tissues. The scanned area was defined by vertebrae T12 to S1. The images were acquired in the axial plane with the following sequences: T2 FIESTA (TR=3.8ms, TE=1.6ms, ST=5mm, spacing=1mm, matrix size 512×512) and T1 FSPRG (TR=200ms, TE=1.6ms, ST=5mm, spacing=1mm, matrix size 512×512). The MRI images were examined by a single certified radiologist who used the images to measure the thickness of the abdominal fat layer, thickness of the abdominal muscles, and the width of abdominal separation.
The measurements were performed at epi-umbilical and sub-umbilical scans. The muscle thickness was measured at the midpoints of left and right rectus abdominis. The fat thickness was measured above the muscle measurements. The average results for each patient were calculated.
The normality of the data was verified using a Shapiro-Wilk normality test. The significance of statistical difference between the baseline data and post-treatment data was tested using the paired t-test.
RESULTS
The treatment procedure. All 10 patients completed the treatment procedure and attended the one-month and three-month follow-up visits. A total of nine out of the 10 patients were successfully recalled for examination at six months after the last treatment. The treatments were well tolerated; eight out of the 10 patients reported the treatments to be comfortable while two patients reported the treatments to be neither uncomfortable nor comfortable. The intensity of the muscle stimulation was gradually increased during the treatments, and all patients were able to tolerate 100-percent intensity by the second treatment. After the treatment sessions, the subjects were able to resume their daily activities. Mild muscle fatigue, comparable with post-exercise soreness, was the only reported AE. The fatigue resolved itself within 48 hours post-treatment. The patients did not report any changes in their diet or physical activity levels.
Abdominal separation. The baseline MRI measurements of the abdominal separation indicated diastasis recti in four of the 10 patients, with the measured distance being higher than 27mm. The condition was resolved in two patients at the one-month follow-up and resolved in all four patients at the three-month follow-up visit. In general, shortening of the abdominal separation was seen in all of the examined patients, and eight of the 10 patients showed more than 15.0-percent improvement at the one-month follow-up. During the three-month follow-up, the measured improvement was higher than 20.0 percent in nine of the 10 patients.
At baseline, the average epi-umbilical abdominal separation was 22.3±8.1mm, and the sub-umbilical separation averaged 11.6±4.6mm. At one-month follow-up, the abdominal separation reduced significantly (p<0.05) by 15.1 percent epi-umbilically and by 18.3 percent sub-umbilically compared to the baseline. Average reduction in abdominal separation at one-month follow-up was 16.7 percent (-2.6±1.1mm). During the three-month follow-up, the abdominal separation showed additional reduction compared to the one-month measurements (p<0.05). Compared to baseline, the average reduction was 22.7 percent (-3.6±1.4mm)—23.8 percent sub-umbilically and 21.5 percent epi-umbilically at three-months post-treatment. Detailed results are reported in Table 1.
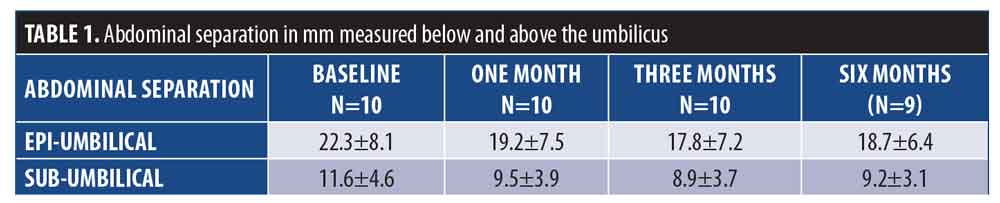
The improvement in abdominal separation was maintained through the six-month follow-up visit. Nine patients who attended the six-month follow-up visit showed a reduction from 23.6±7.5mm (epi-umbilically) and 12.4±4.1mm (sub-umbilically) at baseline to 18.7±6.4mm and 9.2±3.1mm at six-month follow-up, respectively, which corresponds to an average reduction of 23.2 percent (-4.0±1.8mm) in abdominal separation. The differences were statistically significant (p<0.05).
Correlation analysis showed a strong positive relationship (r=0.87; p<0.001) between the level of baseline abdominal separation and the level of observed improvement at three months. This indicates that the patients with a more severe condition were more likely to see improvements. The level of improvement, however, was independent of the baseline weight and BMI.
Muscle thickness. The muscle thickness increased in all 10 patients at the one- and three-month post-treatment visits. Statistical analysis showed that the thickness of the rectus abdominis muscle increased significantly (p<0.05) by 20.5 percent (+2.0±0.6mm), on average, at the one-month follow-up. At the three-month follow-up, muscle thickness increased by 21.3 percent (2.1±0.7mm), on average, compared to the baseline. The difference between the one-month and three-month measurements was not statistically significant (p>0.05).
The improvement between the epi-umbilical and sub-umbilical measurements at the one-month follow-up (19.4% and 21.6%, respectively) and three-month follow-up (21.4% and 21.2%, respectively) did not show significant differences. The detailed results can be seen in Figure 1.
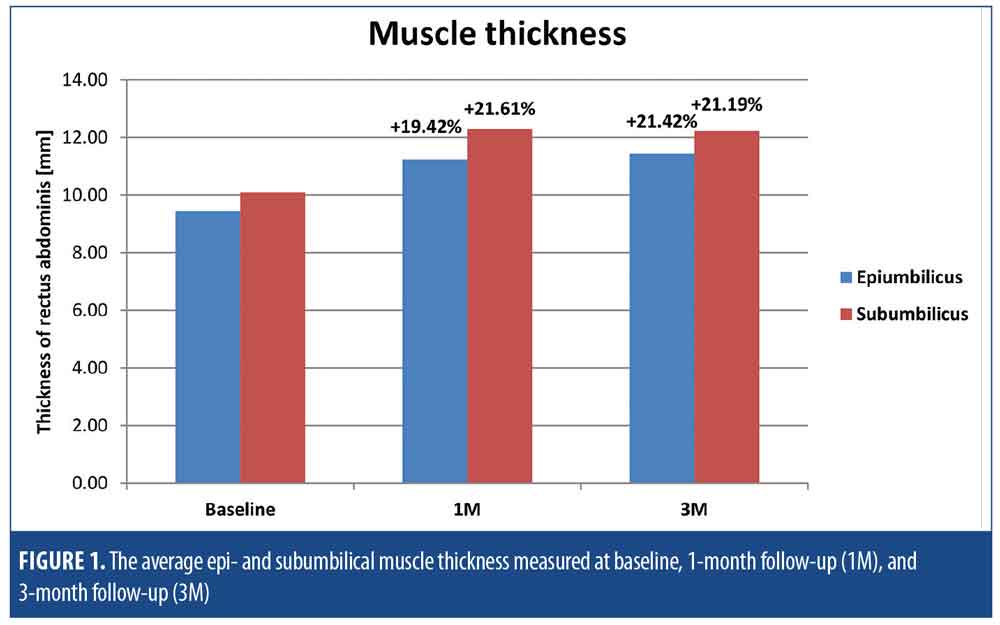
The analysis of the six-month MRI images demonstrated a sustained increase in the muscle thickness, compared to measurements at three three-month follow-up. At baseline, the epi-umbilical and sub-umbilical muscle thickness measurements of the nine patients who returned for the six-month follow-up were 9.1±2.2mm and 9.8±1.9mm, respectively. At the three-month follow-up, muscle thickness increased to 11.0±2.8mm (epi-umbilical) and 11.9±2.4mm (sub-umbilical), an incremental increase of 21.7 percent (2.0±0.6mm), on average. At the six-month follow-up, the nine patients maintained muscle improvement by 21.7 percent, as the epi- and sub-umbilical muscle thickness was 11.1±2.6mm and 11.8±2.3mm, respectively.
Similarly, the correlation analysis for abdominal separation showed a statistically significant (r=0.57; p<0.01) relationship between baseline muscle thickness and measured improvement at three months, indicating that subjects who had lower baseline muscle thickness were more likely to see greater improvement compared to those with higher baseline muscle thickness. The improvement was independent of patient weight, BMI, or baseline fat thickness.
Fat thickness. The MRI images of all patients demonstrated a significant reduction (p<0.05) in the thickness of subcutaneous fat tissue. The total average reduction across the abdomen at one-month follow-up was 17.0 percent (-2.1±1.1mm), with the thickness of fat layer decreasing from 13.9±8.4mm to 11.8±7.4mm. The fat layer was further reduced to 20.1 percent (-2.5±1.3mm), which was significant (p<0.05), at the three-month follow-up while fat reduction greater than 17.0 percent was observed in eight of the 10 patients who attended the three-month follow-up visit. The changes were independent of baseline weight and BMI. Individual results of each patient at the three months are displayed in Figure 2.
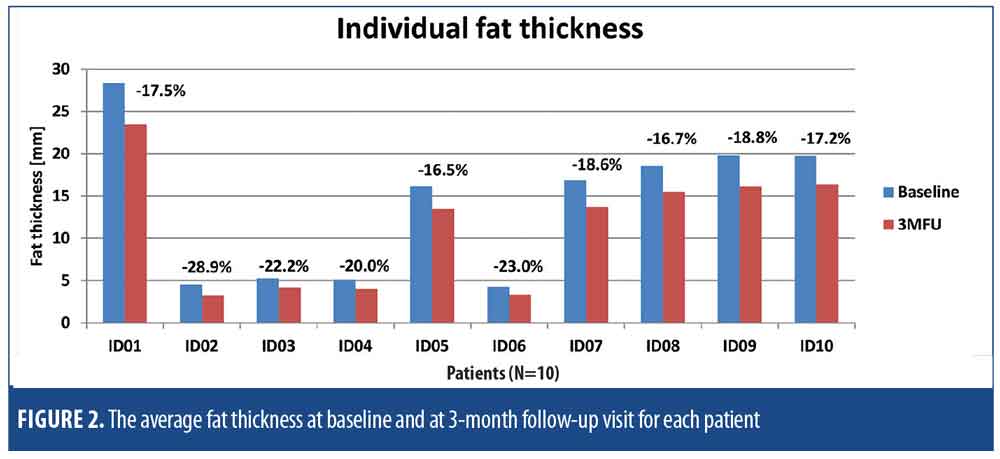
Patients maintained a 17.6-percent fat reduction at the six-month follow-up visit (-2.0±1.3mm), compared to baseline measurements. In absolute values, the average fat thickness of these patients was 13.2±8.9mm at baseline, 11.2±7.9mm at one month, 10.8±7.6mm at three months, and 11.2±7.7mm at six months post-treatment.
The fat reduction was equally distributed across the abdomen. The difference between the fat reduction above the umbilicus and below umbilicus was statistically insignificant (p>0.05) at one-month and three-month follow-ups. A strong positive correlation (r=0.97; p<0.001) was found between the baseline fat thickness and the measured level of fat thickness reduction. This implies that patients with a thicker fat layer at baseline saw greater improvement in absolute values.
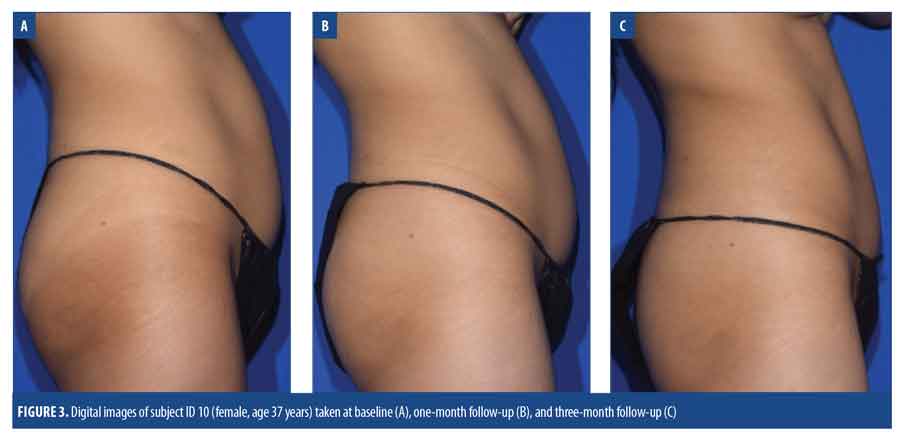
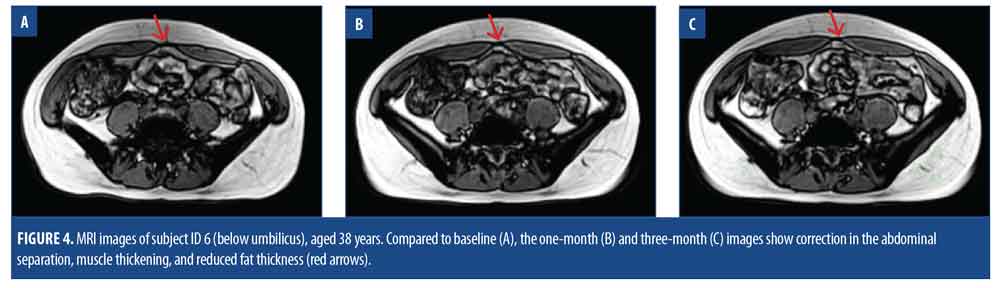
Other results. The weight of the subjects remained constant—the average baseline weight was 60.0±8.1kg, 59.7±8.1kg at one-month follow-up, 59.9±8.4kg at three-month follow-up, and 60.0±7.9kg at the six-month follow-up. The improvement observed in digital photographs corresponded with the improvement measured in the MRI images. Examples of digital images and corresponding MRI images can be seen in Figures 3 and 4.
DISCUSSION
The measurements performed on the MRI images showed an improvement in all three monitored parameters: the width of abdominal separation, subcutaneous fat thickness, and thickness of the rectus abdominis muscle. A notable improvement in digital photographs accompanied these observations.
Compared to previous studies, the muscle improvements we observed in this study are more visible. The most noticeable difference between the results of the current study and previous studies was observed in the abdominal separation. Kent et al8 and Kinney et al7 reported improvement by 9.5 and 10.4 percent, respectively, while our results at three months showed a 22.7-percent reduction in the abdominal separation. We contribute this difference to the patient selection in this study. Our study focused on postpartum women whose conditions at baseline were more severe compared to the subjects in the other studies.
Greater muscle thickening was observed in our study compared to the Kent et al study.8 The average muscle thickening reported in Kent et al8 was 15.47 and 14.8 percent, while our study group showed an average thickening of 21.3 percent. This could be attributed to two factors: 1) our patient group’s initial muscle thickness was 9.1mm, whereas the average thickness in previous studies was 11.0 to 11.1mm, suggesting that the patients of this study had a greater potential for improvement the groups in the other study. Second, the reported values in the previous studies are corresponding to one- and two-month measurements. The results of patients seen in these studies could be further improved in additional follow-up and thus decreasing the discrepancy.
The fat measurements we observed in our patients were, however, similar to previous findings7,8,10 in which the reported fat reduction ranged between 17.5 and 23.3 percent. Our values of 17.0 and 20.3 percent seen at one month and three months fall close to this range.
Due to the additional evaluation at six-month follow-up, we obtained data regarding the long-term effects of HIFEM treatments. While long follow-ups can introduce bias due to the lack of control over patient lifestyle and food habits, these six-month data provide some degree of insight into what can be expected long-term following HIFEM treatment.
The best results in muscle thickness and abdominal separation were seen at three months post-treatment. At six-month post-treatment, results were maintained, which suggests that the effect on muscles is persistent in the long-term. Similarly, the best improvement in fat tissue was seen at three months (20.1%). However, at six months, we could see a slight decline in improvement (17.6%). Although the individual results might vary, the results suggest that the patients would benefit from maintenance treatments six months after the last treatment to avoid significant declines in the treatment outcomes.
A commonly used approach for the treatment of abdominal separation is an abdominal exercise program. Two eight-week studies11,12 investigated the effects of abdominal exercise programs in postpartum women, showing a14.0-11 and 16.0-percent12 reduction in abdominal separation after eight weeks of exercise. We saw a considerably greater improvement after the application of the HIFEM procedure in the present study (22.7%), indicating HIFEM-induced supramaximal contractions play an important role in the reparative process.
Limitations. The present study is limited by the low number of test subjects (10) due to the specificity of the inclusion criteria. Future studies in larger sample sizes with greater statistical power are necessary to validate the outcomes of this study. Since this study was a first investigation of the applicability of the HIFEM procedure for the treatment of abdominal separation and body remodeling after childbirth, the study lacks a control group, which is also a limitation. Future studies should include a control or sham group to identify and reduce the risk of bias.
CONCLUSION
The HIFEM procedure appears to be effective in producing positive abdominal remodeling in women after childbirth by reducing abdominal separation and fat thickness and increasing abdominal muscle mass. Our results suggest that postpartum women may achieve greater improvements with the HIFEM procedure, compared to the general population, and that the HIFEM procedure may yield better results than abdominal exercise programs in this patient population. While additional larger, controlled studies are needed to confirm these findings, we believe HIFEM has demonstrated its potential use as a convenient, noninvasive treatment for improving abdominal appearance in women following childbirth.
References
- Rallis S, Skouteris H, Wertheim EH, Paxton SJ. Predictors of body image during the first year postpartum: a prospective study. Women Health. 2007;45(1):87–104.
- Jenkin W, Tiggemann M. Psychological effects of weight retained after pregnancy. Women Health. 1997;25(1):89–98.
- Kantrowitz-Gordon I, Abbott S, Hoehn R. Experiences of postpartum women after mindfulness childbirth classes: a qualitative study. J Midwifery Womens Health. 2018;63(4):462–469.
- Mota P, Pascoal AG, Vaz C, et al. Diastasis recti during pregnancy and postpartum. In: Brandão S, Da Roza T, Ramos I, Mascarenhas T (eds). Women’s Health and Biomechanics, Vol 29. Cham: Springer International Publishing; 2018:121–132.
- Mota PGF da, Pascoal AGBA, Carita AIAD, Bø K. Prevalence and risk factors of diastasis recti abdominis from late pregnancy to 6 months postpartum, and relationship with lumbo-pelvic pain. Man Ther. 2015;20(1):200–205.
- The American Society for Aesthetic Plastic Surgery site. Procedural statistics. 2018. The Aesthetic Society. https://www.surgery.org/sites/default/files/ASAPS-Stats2017.pdf. Accessed September 3, 2020.
- Kinney BM, Lozanova P. High intensity focused electromagnetic therapy evaluated by magnetic resonance imaging: safety and efficacy study of a dual tissue effect based non-invasive abdominal body shaping. Lasers Surg Med. 2019;51(1)40–46.
- Kent DE, Jacob CI. Simultaneous changes in abdominal adipose and muscle tissues following treatments by high-intensity focused electromagnetic (HIFEM) technology-based device: computed tomography evaluation. J Drugs Dermatol. 2019;18(11):1098–1102.
- Weiss RA, Bernardy J. Induction of fat apoptosis by a non-thermal device: mechanism of action of non-invasive high-intensity electromagnetic technology in a porcine model. Lasers Surg Med. 2019;51(1):47–53.
- Katz BE, Bard RL, Goldfarb R, et al. Changes in subcutaneous abdominal fat thickness following high-intensity focused electro-magnetic HIFEM field treatments: a multicenter ultrasound study. In: Lasers in Surgery and Medicine, Vol 50. Dallas (Texas): Wiley Periodicals, Inc.;2018:360–361.
- Khandale SR, Hande D. Effects of abdominal exercises on reduction of diastasis recti in postnatal women. Int J Health Sci. 2016;(6):10.
- Sancho MF, Pascoal AG, Mota P, Bø K. Abdominal exercises affect inter-rectus distance in postpartum women: a two-dimensional ultrasound study. Physiotherapy. 2015;101(3):286–291.

