 J Clin Aesthet Dermatol. 2021;14(4):28–30.
J Clin Aesthet Dermatol. 2021;14(4):28–30.
by Nima Milani-Nejad, MD, PhD; Amy G. Johnson, MD; and Catherine G. Chung, MD
Dr. Milani-Nejad is with the Department of Dermatology at the University of California in Los Angeles, California. Dr. Chung is with the Division of Dermatology in the Department of Internal Medicine as well as the Department of Pathology at The Ohio State Wexner Medical Center in Columbus, Ohio. Dr. Johnson is with the Division of Hematology at The Ohio State University Wexner Medical Center in Columbus, Ohio.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Pancreatic panniculitis occurs in up to three percent of all patients with pancreatic disease. This cutaneous eruption, as implied by the name, is almost exclusively encountered in the context of pancreatic disorders, such as pancreatitis or pancreatic carcinoma. We report three cases in which histopathologic examination demonstrated hallmarks of pancreatic panniculitis occurring in patients without any history or evidence of pancreatic disorder. These nonpancreatic pancreatic panniculitis eruptions might be underreported in the literature.
Keywords: Panniculitis, pancreatic panniculitis, alpha1-antitrypsin deficiency, enzymatic panniculitis, fat necrosis
Pancreatic panniculitis, also known as enzymatic fat necrosis, is a rare form of predominantly lobular panniculitis characterized by subcutaneous fat necrosis, calcification, ghost cells, and basophilic degeneration that was first described in 1883 by Hans Chiari. It is almost exclusively reported in association with pancreatic disorders, such as pancreatitis and pancreatic carcinoma1,2 and typically manifests as tender, firm, erythematous subcutaneous nodules on the lower extremities, buttocks, or trunk.1,2
It is thought that injury to the pancreas results in a release of pancreatic enzymes, such as trypsin, amylase, and lipase, which then spread through hematogenous or lymphatic channels, thereby promoting lipolysis and necrosis of fat lobules remote to the pancreas itself.1,2
We present three cases of subcutaneous fat necrosis with histopathologic features of pancreatic panniculitis in patients without evidence of pancreatic disorder, suggesting that pancreatic panniculitis might occur as an incidental finding in individuals without pancreatic disease.
Case Presentations
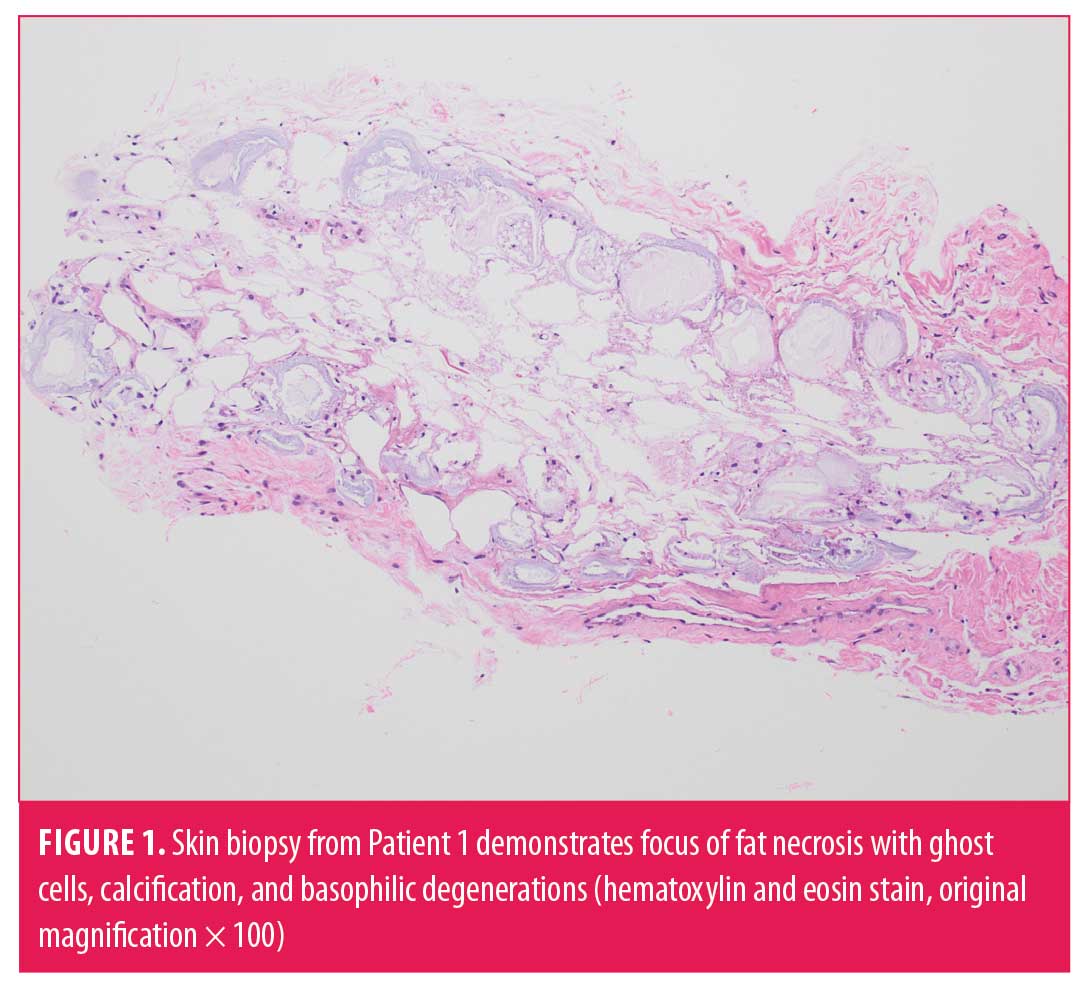
Patient 1. A 57-year-old Caucasian male patient with a medical history significant for alpha1-antitrypsin deficiency and type 2 diabetes mellitus presented with pneumonia and sepsis one month after bilateral lung transplant. He had no history of alcohol use and a remote one-year history of cigarette smoking (0.5 pack/day). Physical examination was notable for erythematous papules with central areas of white discoloration on the left forearm. Biopsy demonstrated fat necrosis characterized by ghost cells, calcification, and basophilic degeneration (Figure 1). No organisms were identified on bacterial and fungal stains. Serum amylase, lipase, and triglyceride levels were normal. Computed tomography (CT) imaging showed normal pancreas without any evidence of pancreatic mass or peripancreatic fluid abnormality.
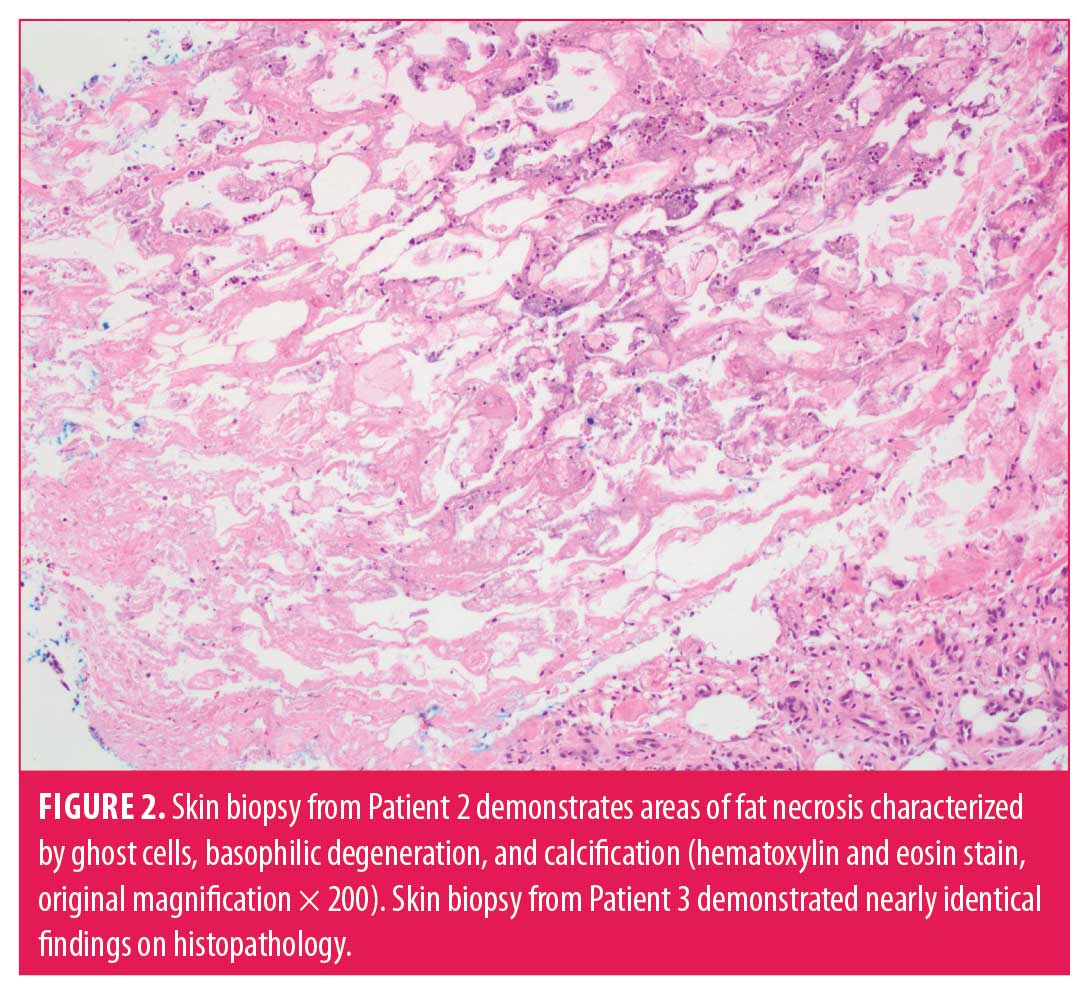
Patient 2. A 66-year-old African-American female patient with a medical history significant for end-stage renal disease on hemodialysis and type 2 diabetes mellitus presented with a four-month history of enlarging tender irregular ulcerative plaques on the left thigh. She had no history of smoking or alcohol use. Incisional biopsy demonstrated the presence of fat necrosis and fibrosis, calcification, ghost cells, and basophilic degeneration (Figure 2). No amylase, lipase, or abdominal imaging findings at the time of diagnosis were available but, upon review of her medical records that included subsequent follow-up data, she was noted to have no history or symptoms suggestive of pancreatic disorder.
Patient 3. A 52-year-old Caucasian male patient presented for the evaluation of a subcutaneous nodule on the left shin present for years. His past medical history was significant for type 2 diabetes mellitus and cholecystectomy. He had no history of smoking and minimal alcohol consumption. The patient underwent excision of the lesion and pathology demonstrated fat necrosis, calcification and focal areas of ossification, ghost cells and basophilic degeneration. He had negative abdominal CT findings and normal lipase/amylase levels around the time of onset, which had been assessed for the evaluation of an unrelated small bowel obstruction; in the subsequent years since the lesion appeared, a review of his medical records demonstrated no history of or subsequent development of pancreatic disease.
Discussion
Pancreatic panniculitis, also known as enzymatic fat necrosis, is a rare cutaneous complication affecting up to three percent of patients with pancreatic disorders.2 It is thought that injury to the pancreas allows trypsin, amylase, and lipase to spread through lymphatic channels or hematogenously, thereby promoting lipolysis, necrosis, and panniculitis within fat lobules remote to the pancreas itself.1–4 However, in-vitro experiments wherein human adipose tissue was incubated with pancreatic enzymes and serum from a patient with pancreatic panniculitis did not result in fat necrosis, which suggests that other factors, such as prior vascular damage or the release of adipokines, might also contribute to the development of pancreatic panniculitis.5,6
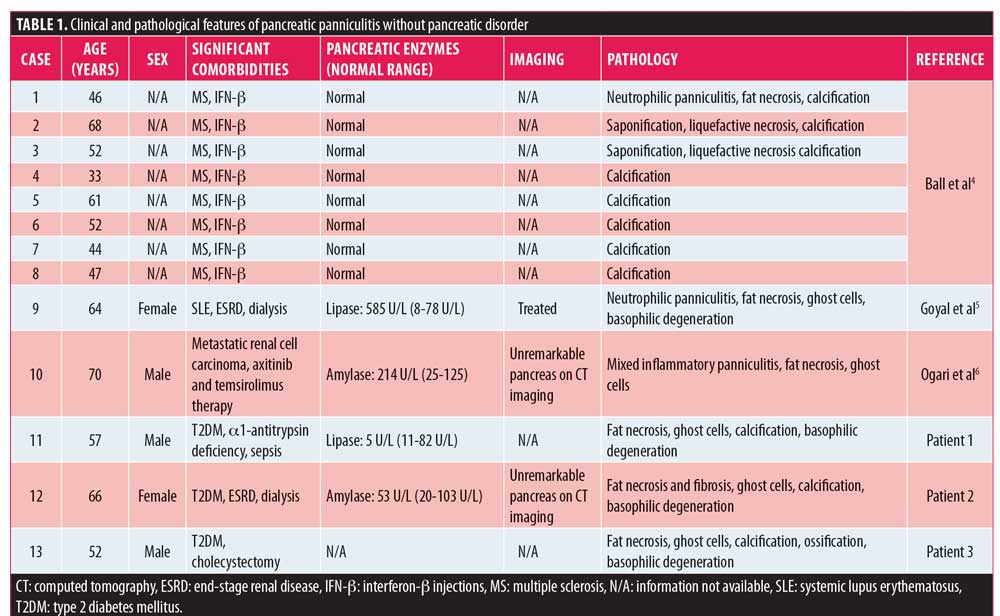
Pancreatic panniculitis has rarely been reported in the absence of pancreatic disease in the literature (Table 1). Ball et al4 reported a series of eight patients who developed panniculitis with features of pancreatic panniculitis at injection sites of interferon-beta in patients with multiple sclerosis.4 One patient with systemic lupus erythematous and lupus nephritis on dialysis developed panniculitis with features of pancreatic-like panniculitis.5 Although this patient had elevated amylase and lipase levels, since no identifiable pancreatic abnormality was identified on imaging, this elevation was attributed to expected effects of decreased renal function and dialysis rather than a pancreatic disorder.5 Similarly, a patient with metastatic renal cell carcinoma developed pancreatic panniculitis while receiving axitinib and temsirolimus without any pancreatic disease.6
Patient 1 in our case series had no evidence of any pancreatic disorder, as evidenced by normal abdominal imaging and laboratory evaluations of pancreatic enzymes. It is notable that this patient did have an alpha1-antitrypsin deficiency, a disorder which may also be associated with lobular panniculitis, neutrophilic infiltrate, and fat necrosis.1 However, patients with alpha1-antitrypsin deficiency panniculitis do not typically demonstrate findings of ghost cells and saponification with basophilic degeneration of adipocytes, which are characteristic of pancreatic panniculitis.1
The underlying cause for pancreatic panniculitis in Patient 1 remains elusive given the normal pancreas and enzymes. The pathophysiology of pancreatic panniculitis is traditionally attributed to liquefaction and necrosis of adipocytes by pancreatic enzymes resulting in the pathological findings of panniculitis, necrosis, ghost cells, and basophilic degeneration.1,2 It has been demonstrated that amylase and lipase by themselves are not capable of resulting in pancreatic panniculitis in in-vitro studies,3 raising the possibility that additional factors such as cytokines are responsible.1–3 It is possible that alterations in the cytokine profile secondary to sepsis in this patient7 ultimately resulted in the histopathological features of pancreatic panniculitis.
Abdominal imaging and pancreatic enzyme levels were not available for Patient 2, but an exhaustive review of her medical records did not reveal any history or subsequent development of pancreatic disorder. It should be noted that this patient did have end-stage renal disease on dialysis, and studies have shown elevated amylase and lipase levels in this patient population.8–10 Thus, it is suspected that transient elevations of amylase and lipase in Patient 2 might have precipitated the enzymatic liquefaction of adipocytes resulting in the histopathological changes of pancreatic panniculitis in the absence of true pancreatic disease.
Conclusion
Histopathology might suggest pancreatic panniculitis despite an absence of findings that support the presence of pancreatic disease. All three of our patients had a history of type 2 diabetes, but the significance of this in the development of panniculitis is unclear. These cases suggest that nonpancreatic pancreatic panniculitis without an identified pancreatic pathology might be more common than currently reported in the literature and warrants further recognition and investigation.
References
- Lyon MJ. Metabolic panniculitis: alpha-1 antitrypsin deficiency panniculitis and pancreatic panniculitis. Dermatol Ther. 2010;23(4):368–374.
- Requena L, Sanchez Yus E. Panniculitis. Part II. Mostly lobular panniculitis. J Am Acad Dermatol. 2001;45(3):325–361; quiz 362–324.
- Berman B, Conteas C, Smith B, et al. Fatal pancreatitis presenting with subcutaneous fat necrosis. Evidence that lipase and amylase alone do not induce lipocyte necrosis. J Am Acad Dermatol. 1987;17(2 Pt 2):359–364.
- Ball NJ, Cowan BJ, Hashimoto SA. Lobular panniculitis at the site of subcutaneous interferon beta injections for the treatment of multiple sclerosis can histologically mimic pancreatic panniculitis. A study of 12 cases. J Cutan Pathol. 2009;36(3):331–337.
- Goyal A, Jain M, Rehberg K, et al. Pancreatic panniculitis in active systemic lupus erythematosus. J Cutan Pathol. 2019;46(9):688–690.
- Ogari K, Arakawa Y, Cho Z, et al. Subcutaneous fat necrosis due to molecular-targeted therapy. J Dermatol. 2017;44(3):e7–e8.
- Matsumoto H, Ogura H, Shimizu K, et al. The clinical importance of a cytokine network in the acute phase of sepsis. Sci Rep. 2018;8(1):13995.
- Collen MJ, Ansher AF, Chapman AB, et al. Serum amylase in patients with renal insufficiency and renal failure. Am J Gastroenterol. 1990;85(10):1377–1380.
- Shibasaki T, Matsuda H, Ohno I, et al. Significance of serum lipase in patients undergoing hemodialysis. Am J Nephrol. 1996;16(4):309–314.
- Vaziri ND, Chang D, Malekpour A, Radaht S. Pancreatic enzymes in patients with end-stage renal disease maintained on hemodialysis. Am J Gastroenterol. 1988;83(4):410–412.

