 J Clin Aesthet Dermatol. 2020;13(6):36–39
J Clin Aesthet Dermatol. 2020;13(6):36–39
by Shruti Sharma, MD; Priyadarshini Sahu, MD, DNB; Surabhi Dayal, MD; Anjali Yadav, MBBS; and Komal Brar, MD
Drs. Sharma, Sahu, Dayal, and Yadav are with the Department of Dermatology at the Pandit B.D. Sharma Postgraduate Institute of Medical Sciences in Rohtak, Haryana, India. Dr. Brar is with the Department of Pathology at the Pandit B.D. Sharma Postgraduate Institute of Medical Sciences in Rohtak, Haryana, India.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Nevus comedonicus and hidradenitis suppurativa (HS) are disorders of the pilosebaceous unit sharing a similar pathogenesis of follicular occlusion. To our knowledge, less than 10 cases of HS-like lesions complicating nevus comedonicus have been reported. We describe a six-year-old female child with congenital linear nevus comedonicus in the left axilla and groin, complicated by recurrent HS-like lesions in the two years prior to presenting to our clinic. After a meticulous review of the literature, we propose a novel term, nevus comedonicus suppurativa, for this clinical entity.
Keywords: Nevus comedonicus suppurativa, nevus comedonicus, hidradenitis suppurativa
Nevus comedonicus (NC) is a rare type of epidermal nevus that occurs either congenitally or in early childhood. It is clinically characterized by asymptomatic, closely arranged, dilated follicular openings with keratinous plugs. These resemble classical comedones and most commonly affect the head and neck region. Overstimulation of fibroblast growth factor receptor-2 (FGFR2) signaling with increased expression of interleukin-1alpha might be involved in its pathogenesis. Association of NC with a variety of skeletal, ocular, and central nervous system abnormalities is known as nevus comedonicus syndrome (NCS).1
NC is classified into two types: the classical type an inflammatory NC type characterized by papules and pustules.1 Here, we report a case of a prepubertal female patient presenting with hidradenitis suppurativa (HS)-like lesions complicating unilateral NC. We suggest using the term nevus comedonicus suppurativa to classify this type of NC.
Case Report
A six-year-old female child, born out of nonconsanguineous marriage, presented with recurrent episodes of painful boils in the left groin and inner thigh for two years prior to visiting our clinic. The lesions subsided temporarily upon taking oral antibiotics and painkiller medications. The patient had not applied any topical medication or spray to the lesions. She did not have a history of systemic comorbidities and was not on chronic medications. Her past and family history was unremarkable.
The patient was febrile (100°F) but the rest of the systemic examination revealed no abnormalities. Lymphadenopathy was absent. During cutaneous examination, the left inguinal region showed closely arranged, comedone-like lesions in a linear fashion, extending from the left lower abdomen up to the inner thigh. The lesions were present against a background of a well-demarcated hyperpigmented patch. The comedones were accompanied by deep-seated nodules, abscesses, a few sinus tracts, and scarring (Figure 1). Linearly arranged grouped comedones with a background of hyperpigmentation were also observed in the left axilla (Figure 2). No evidence of inflammation was present in the axilla. Double comedones were not seen. The contralateral axilla and groin appeared normal. Further investigation revealed that comedone-like lesions had been present since birth but remained asymptomatic until two years before visiting our clinic. The patient had no history of premature menarche and a thorough physical examination did not reveal signs of endocrinal abnormalities, such as hirsutism, acne/oily skin, alopecia, acanthosis nigricans, clitoromegaly, or cushingoid appearance. Skeletal, ocular, and neurologic examination findings were within normal limits. The outcomes of routine blood investigations were also normal. Metabolic syndrome was ruled out on the basis of normal blood pressure, an absence of central obesity, and normal fasting blood sugar and lipid profiles. An ultrasound of the abdomen showed no feature of polycystic ovaries nor any other abnormality. Free T3, T4, and thyroid-stimulating hormone results were found to be within normal limits. Unfortunately, other hormonal investigations, such as testosterone levels, dehydroepiandrosteronsulfate, sex hormone-binding globulin, estrogen, follicle-stimulating hormone, luteinising hormone, prolactin, and fasting insulin levels were not completed due to a lack of testing materials in our institute and the inability of the patient’s family to pay for private testing.
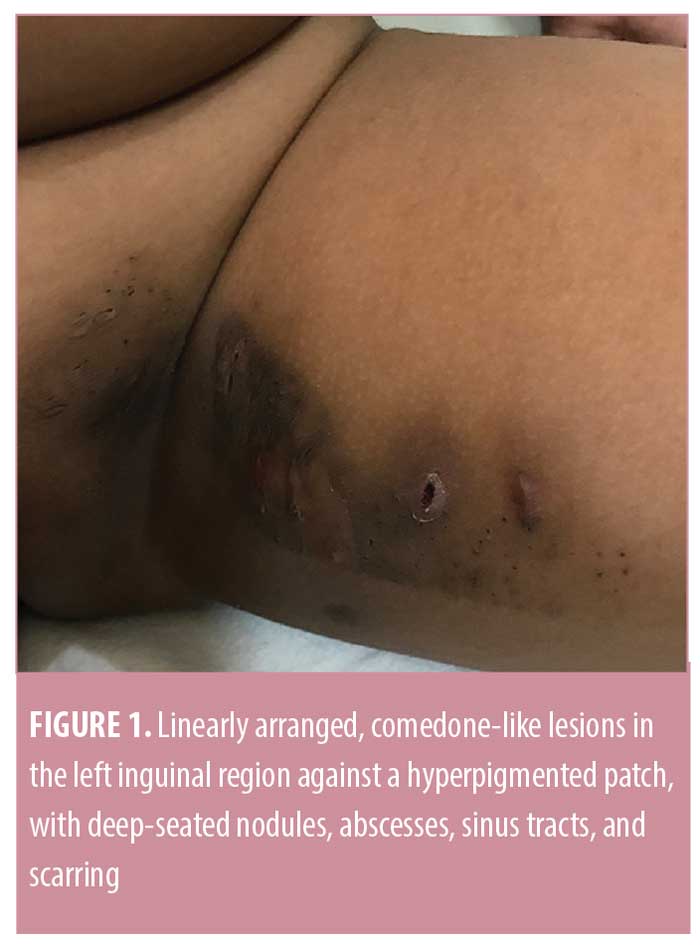

Culture from aspirated material was sterile. Two skin biopsies were sent, one from the axilla and one from the inguinal region, with differential diagnoses of NC and HS. A biopsy report from the axilla showed findings of hyperkeratotic epidermis with mild spongiosis, lymphocytic exocytosis, and a dilated hair follicle, consistent with the diagnosis of NC (Figure 3). The second biopsy showed hyperkeratotic and acanthotic epidermis along with areas of necrosis, dense granulation tissue, and suppurative inflammation, supporting the diagnosis of HS (Figure 4). Therefore, we made the diagnosis of unilateral linear NC without associated NCS yet complicated by HS-like lesions. The patient was prescribed an oral non-steroidal anti-inflammatory drug and topical clindamycin. No improvements were observed after one week of this regimen, so she was advised to take oral amoxicillin and clavulanic acid for five days and was planned to receive oral isotretinoin, but was lost to follow up.


Discussion
HS is a chronic disabling disorder characterized by deep, tender subcutaneous nodules, sinuses, and fibrosis. It usually begins after puberty and the most commonly affected sites are the axillae, perianal region, and perineum. It was first thought to be a disease of the apocrine gland but, histopathologically, it has been shown to involve the pilosebaceous unit, whereas the apocrine gland can be secondarily infected. The alteration of the terminal follicular epithelium with dilatation and distortion of infundibulum leads to the occlusion of the affected hair follicle, eventually resulting in bacterial infection and inflammation.2
The noteworthy features of our case were the sites of involvement, distinctive morphology, and complication by HS-like lesions. In our patient, the unilateral axilla and groin were affected, but these sites are usually not affected by NC. Further, the lesions followed a linear pattern and were present against a background of a well-defined hyperpigmented patch. Hyperpigmentation was absent in the contralateral axilla and groin. To our knowledge, NC on the background of a hyperpigmented patch has not been described in the literature. A review of the patient’s history did not reveal the cause of hyperpigmentation, as the parents did not report the use of any spray or topical medication, indigenous or otherwise. Despite this, we still suspect some topical spray or medication as the cause of hyperpigmentation, due to its well-defined but bizarre margins, as if a liquid or a spray had trickled down the skin.
Descriptions of the inflammatory aspects of NC date back to 1933. Vasiloudes et al3 discussed five pediatric cases with inflammatory acneiform or cystic lesions on NC. Less than 10 cases of HS-like lesions in association with NC have been described in the worldwide literature (Table 1), to the best of our knowledge.4–10 In our patient, NC in the left axilla was noninflammatory (i.e., classical), whereas, NC in the left inguinal region had evolved into hidradenitis-like lesions in the two years prior to the patient presenting to our clinic. The role of mechanical stress by tight clothing on the diseased follicles of NC has been hypothesized to cause HS-like lesions.3 Histopathologically, HS-like lesions are indistinguishable from the classical HS. The only differentiating point between the two is that HS is a primary disease of the pilosebaceous unit usually occurring after puberty, whereas HS-like lesions arise secondarily on the already diseased follicles of NC due to mechanical stress, generally affecting prepubertal children .2,4,5,7–10 NC has a benign clinical course not requiring any treatment, unless it evolves into HS-like lesions. The treatment of such complicated lesions is, in general, unsatisfactory, due to the difficulty in approaching such lesions. Some potential therapeutic options are oral and topical antibiotics, oral isotretinoin, CO2 and erbium-doped yttrium aluminium garnet lasers, surgical excision, needle aspiration or drainage, and cryotherapy.2,11 Recently, Sahu et al10 discussed the role of the biologic adalimumab for treating HS-like lesions in a prepubertal female patient with NCS. Although isotretinoin has not been recommended in the treatment guidelines for HS, various studies have investigated it as a possible therapeutic option.11 While the response in severe disease is unsatisfactory, some reports suggest a favorable response with isotretinoin treatment in younger female patients without obesity with mild to moderate HS and a history of or coexisting acne.11 Moreover, pretreatment with isotretinoin at 0.5 to 1mg/kg daily for a few months before surgery has been shown to reduce the inflammatory components.11 Adverse effects of isotretinoin, particularly teratogenicity and concerns regarding depression and suicide ideation, limit the degree of comfort with which isotretinoin is prescribed in the pediatric population, adolescents, and patients who can become pregnant.12 Frequent side effects of isotretinoin include cheilitis and xerosis, which usually respond well to the liberal use of emollients. An isotretinoin symptom survey was designed to assess the presence or absence of 13 possible adverse effects: dry lips, dry/bloodshot eyes, dry skin, muscle aches/pain, nosebleed, frequent headache, mood swings, depression, suicidal thoughts, paronychia, rash, trouble with night vision, and severe sun sensitivity/sunburn. While the monitoring of liver function tests and lipid profile remain essential, simple tools like the described isotretinoin symptom survey might be useful for monitoring any adverse effects.11,12
 Besides nevus comedonicus, few case studies have shown an association of HS-like lesions in the setting of other dermatological disorders sharing pathogenesis of follicular occlusion, such as steatocystoma multiplex, pityriasis rubra pilaris, and acanthosis nigricans.1,13–17 The evolution of steatocystoma multiplex into a suppurative form as a result of the development of HS-like lesions is referred to as steatocystoma multiplex suppurativum.13–17 This term was probably introduced due to a distinct clinical behavior and challenging management of the latter compared to the classical steatocystoma multiplex.
Besides nevus comedonicus, few case studies have shown an association of HS-like lesions in the setting of other dermatological disorders sharing pathogenesis of follicular occlusion, such as steatocystoma multiplex, pityriasis rubra pilaris, and acanthosis nigricans.1,13–17 The evolution of steatocystoma multiplex into a suppurative form as a result of the development of HS-like lesions is referred to as steatocystoma multiplex suppurativum.13–17 This term was probably introduced due to a distinct clinical behavior and challenging management of the latter compared to the classical steatocystoma multiplex.
Similar to steatocystoma multiplex suppurativum, this new variant, in which HS-like lesions complicate NC, also deserves special recognition in the literature owing to its distinction from classical NC in its clinical presentation, recurrent course, recalcitrant nature to treatment, and decreased patient quality of life. Hence, the label nevus comedonicus suppurativa is suggested for this novel entity.
References
- Tchernev G, Ananiev J, Semkova K, et al. Nevus comedonicus: an updated review. Dermatol Ther (Heidelb). 2013;3(1):33–40.
- Patil S, Apurwa A, Nadkarni N, et al. Hidradenitis suppurativa: inside and out. Indian J Dermatol. 2018;63(2):91–98
- Vasiloudes PE, Morelli JG, Weston WL. Inflammatory nevus comedonicus in children. J Am Acad Dermatol. 1998;38(5 Pt 2):834–836.
- Dufour DN, Bryld LE, Jemec GB. Hidradenitis suppurativa complicating naevus comedonicus: the possible influence of mechanical stress on the development of hidradenitis suppurativa. Dermatology. 2010;220(4):323–325.
- Qian G, Tao L, Chongehen Z, et al. Naevus comedonicus syndrome complicated by hidradenitis suppurativa-like lesions responding to acitretin treatment. Acta Derm Venereol. 2015;95(8): 992–993.
- Bettoli V, Toni G, Ricci M, et al. Hidradenitis suppurativa-acne inversa-like lesions complicating naevus comedonicus: second case supporting the mechanical stress as a triggering factor. G Ital Dermatol Venereol. 2016;151(3):306–307.
- Higgins R, Pink A, Hunger R, et al. Generalized comedones, acne, and hidradenitis suppurativa in a patient with an FGFR2 missense mutation. Front Med (Lausanne). 2017;4:16.
- Ravaioli GM, Neri I, Zannetti G, Patrizi A. Congenital nevus comedonicus complicated by a hidradenitis suppurativa-like lesion: report of a childhood case. Pediatr Dermatol. 2018;35(5):e298–e299.
- Manikavachakan N, Siddaraju MN, Rajendran SC, Venkataraman A. Extensive nevus comedonicus, complicated with recurrent abscesses, successfully treated with surgical resurfacing. J Cutan Aesthet Surg. 2018;11(1):33–37.
- Sahu P, Aggarwal P, Dayal S, Kumar Jain V. Biologic therapy: a boon for hidradenitis suppurativa-like lesions complicating naevus comedonicus in a prepubertal child. Clin Exp Dermatol. 2019;44(3):322–324.
- Huang CM, Kirchhof MG. A new perspective on isotretinoin treatment of hidradenitis suppurativa: a retrospective chart review of patient outcomes. Dermatology. 2017;233(2–3):120–125.
- Hodgkiss- Harlow CJ, Eichenfield LF, Dohil MA. Effective monitoring of isotretinoin safety in a pediatric dermatology population: A novel “patient symptom survey” approach. J Am Acad Dermatol. 2011;65(3):517–524.
- Lima-Santana CNL, Pereira DN, Lisboa AP, et al. Steatocystoma multiplex suppurativa: case report of a rare condition. An Bras Dermatol. 2016;91(5 Suppl 1):51–53.
- Fekete GL, Fekete JE. Steatocystoma multiplex generalisata partially suppurativa-case report. Acta Dermatovenerol Croat. 2010;18(2):114–119.
- Apaydin R, Bilen N, Bayramgürler D, et al. Steatocystoma multiplex suppurativum: oral isotretinoin treatment combined with cryotherapy. Australas J Dermatol. 2000;41(2):98–100.
- Rosen BL, Brodkin RH. Isotretinoin in the treatment of steatocystoma multiplex: a possible adverse reaction. Cutis. 1986;37(2):115–120.
- Statham BN, Cunliffe WJ. The treatment of steatocystoma multiplex suppurativum with isotretinoin. Br J Dermatol. 1984;111(2):246.
