 by Bruna Souza Felix Bravo, MD; Leonardo Gonçalves Bravo, MD; Camila Mariano da Rocha, MD; Stephanie Bianco de souza, MD; Fernando Luis Lopes, MD; and Julien Totti, MD
by Bruna Souza Felix Bravo, MD; Leonardo Gonçalves Bravo, MD; Camila Mariano da Rocha, MD; Stephanie Bianco de souza, MD; Fernando Luis Lopes, MD; and Julien Totti, MD
Dr. B. Bravo is with the Institute of Dermatology of Professor Rubem David Azulay in Rio de Janeiro, Brazil. Dr. L. Bravo is Full member of the Brazilian society of plastic surgery, Plastic surgeon at Burn Center in Hospital Souza Aguiar Rio de Janeiro, Plastic surgeon at federal Hospital servidores do estado do Rio de Janeiro. Dr. Mariano da Rocha is with the Federal University of Health Sciences of Porto Alegre in Porto Alegre, Brazil, and the Federal University of Rio de Janeiro in Rio de Janeiro, Brazil. Drs. De Souza and Lopes dos Santos are with Gamboa Hospital in Rio de Janeiro, Brazil. Dr. Totti de Bastos is with the Federal Hospital of Lagoa in Rio de Janeiro, Brazil.
Funding: No funding was provided for this article.
Disclosures: Dr. BSF Bravo reports that he is a speaker for Allergan. The other authors have no conflicts of interest relevant to the content of this article.
Abstract: The nose is an essential feature when considering the aesthetic appeal of the face. As aesthetic preferences vary from person to person, the concept of the “ideal” nose must be applied on a case-by-case basis, with respect to the classical patterns of anthropometry, sex, ethnic group, and psychosocial factors. Interest in less invasive procedures for nasal correction has increased considerably, among which is the emerging use of hyaluronic acid for nonsurgical rhinoplasty. In this article, the authors present an objective review of the anatomy of the nasal region, the evaluation and indications of nasal filling with hyaluronic acid, a description of the technique, and brief discussion of associated complications.
Keywords: Nasal filler, anthropometry, proportions, hyaluronic acid, nasal correction
J Clin Aesthet Dermatol. 2018;11(4):36–40
Nonsurgical rhinoplasty using hyaluronic acid is an effective technique for ameliorating nasal defects. It can be classified as primary, when the patient has had no previous procedures, or secondary, when used for corrections after surgical rhinoplasty.1
Surgical nasal remodeling, which is the gold standard for correcting nasal defects, allows for precise improvements.2 However, certain surgical procedures might be unsuitable for patients who are interested in the correction of small defects or desire improvements complementary to a previous surgical procedure. In these cases, the use of hyaluronic acid is a safe, less invasive, and less costly alternative to surgery that requires shorter recovery time and has less associated risks of complication.
In both men and women, the nose is an essential feature when considering the aesthetic appeal of the face.3 As aesthetic preferences vary from person to person, the concept of the “ideal” nose should be applied on a case-by-case basis, with respect to the classical patterns of anthropometry, sex, ethnic group, and psychosocial factors.2 Morphology is not only restricted to the static quality of the nose but is directly related to the personality and preferences of the patient. When patients wish to correct or adjust lack of projection of the nasal tip, rectification of the back, or deviations of the septum, hyaluronic acid is an excellent alternative to surgical correction.
Anatomy
The nose is a three-dimensional structure that, when dividing the face vertically into three sections, is located in the middle third of the face. When the face is divided horizontally into fifths, the nose is located in the middle fifth. It is composed of four structures: skin, cartilage, muscle, and bone. Its appearance is defined not only by rigid structures but also by the soft tissue.
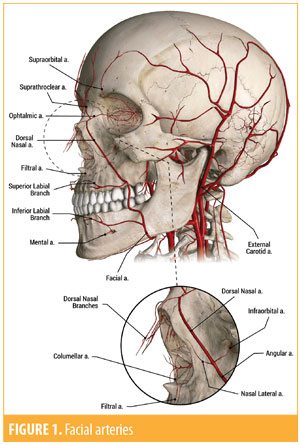
Topographically, the nose extends inferiorly from the forehead and can be divided into three sections. The upper third is formed by the nasal bones and the frontal process of the maxilla; the middle third by the lateral processes of the septal cartilage paired; and the lower third by the inferior nasal spine, part of the maxillary bone process, and by the larger wing cartilages that have three components: a medial branch, a middle branch, and a lateral branch. The piriform, interalar ligaments, and the elastic fibers connect the cartilages to each other.4 The blood supply of the nose originates from both the internal and external carotid arteries.
A branch of the internal carotid, the supratrochlear, and a branch of the external carotid, the facial artery, give rise to the branches that cross the midline to form the vascular network that crosses the dorsum. Its irrigation consists of branches of the ophthalmic and facial arteries. The supratrochlear artery, a branch of the ophthalmic artery, gives rise to the angular, lateral, and external nasal arteries.
The facial artery has a superior path toward the angular artery, and following along its path below the nose, it gives origin to the upper labial artery. The upper labial artery branches into filter branches, columellar branches, and nasal arches (Figures 1 and 2).

The muscular part consists of the nasal transverse, nasal wing lifter, lip and nose lifter, and procerus and orbicularis oculi muscles.
The external nasal sensitivity is mediated by the ophthalmic and maxillary branches, which are branches of the trigeminal nerve. The sensitivity of the cephalic part, radix, nasion, and the lateral faces of the nose are innervated by the branches of the supratrochlear nerve and infratroclear, which are branches of the ophthalmic nerve. The external nasal branch of the ethmoidal nerve emerges between the nasal bone and the superior lateral cartilage, innervating the part of the nasal tip to the columella.
Several components and external reference points should be noted by the clinician when considering nasal characteristics and alterations. From the top to the bottom, the nose is divided into the glabella, the radix (deepest part of the back), the rhinion (cartilaginous bone union), the supratip (the lowest point of the back, immediately above the nasal tip), and the nasal tip. The nasal tip is the most prominent part of the nose. The nasal pyramid comprises the nostrils, the columella, and the nasal wings (which form the sides of the nasal tip and attach the lobe of the tip to the skin of the face), while in the lower part of the columella, there is the subnasal region.
Materials and Methods
Subjects. We analyzed the clinical data of 44 patients who underwent nasal filling with hyaluronic acid between December 2016 and July 2017. All patients signed a consent form and were informed about the procedure. Photoconsent was provided by individuals whose photos appear in this article.
Symmetry measurements. After obtaining patient medical history, we analyzed their noses in relation to their faces and then individually.5 During the procedure, it is first necessary to exclude intraoral deformities, retrognathisms or prognathisms, and asymmetries. The anthropometric measurements of the nose are the most important part of the nonsurgical rhinoplasty planning, including the patient indication and the technique used, all tailored to the patient’s desired results.
The evaluation starts by analyzing the position of the nose in relation to each third of the face. When dividing the face into thirds latitudinally, the ideal nose should be localized in the middle third of the face and extend from the glabella to the subnasal region (Figure 3).
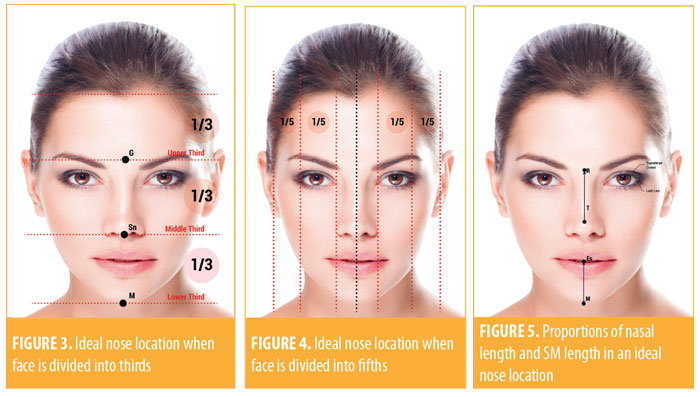
When dividing the face into fifths longitudinally, ideally, the nose should be present in the central fifth and extend into the medial intercantal areas. This extension is the same width of the nasal base in an ideal nose (Figure 4). However, facial differences often produce nasal wings that are wider or narrower. The central fifth should be divided in half to analyze any deviated nasal septum.Viewing the patient from the front, the physician should measure the nasal length, going from the radix to the tip. This distance must be the same from the center point between the lips to the chin in an ideal nose (Figure 5). To calculate and draw the ideal nasal length (RTi), we use two different methods: RTi=0.67 x length of the middle third of the face, or RTi=SM.
Next, the profile analysis must be done. An ideal nose is characterized by a high and projected tip, taking into account ethnic and racial characteristics.1 The patient’s profile should be analyzed for length, height, contour, tip projection, radix depth, and nasolabial angle. It is key to remember that these parameters should be evaluated in both static and dynamic form.4 The real radix projection is calculated by the distance from the corneal plane to the radix plane. The ideal radix projection derives from the ideal nasal length: radix projection=RT1 x 0.28. The average is 9mm to 14mm. The ideal measure of nasal tip projection corresponds to a line drawn from the subnasal area to the tip. This value should ideally correspond to the nasal length value multiplied by 0.67. The nasal length is obtained through a transit line from the radix to the nasal tip, as cited above (Figure 6). While referring to the anatomical reference points, the physician begins to measure the angles and calculate the projections. The physician begins with the nasofrontal angle (aNF), which is defined when two lines are drawn from the radix, one parallel to the back and another parallel to the glabella. The angle of the cross between these two lines should measure 115 to 130 degrees. The larger this angle, then the longer the nose and the lower the tip (Figure 6).
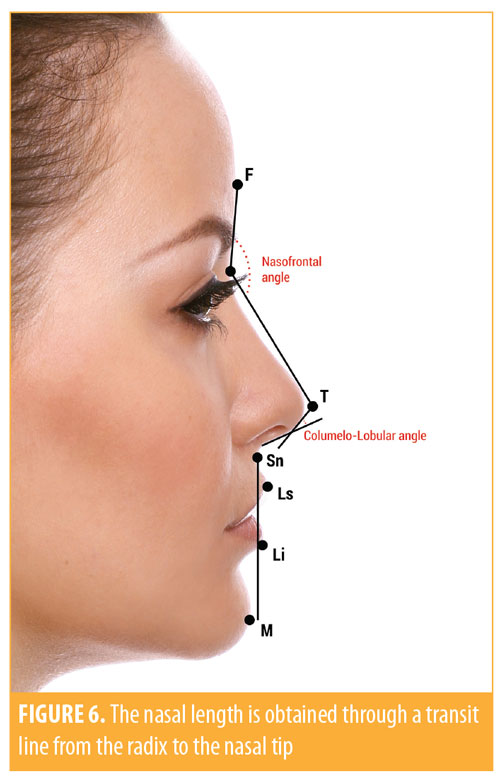
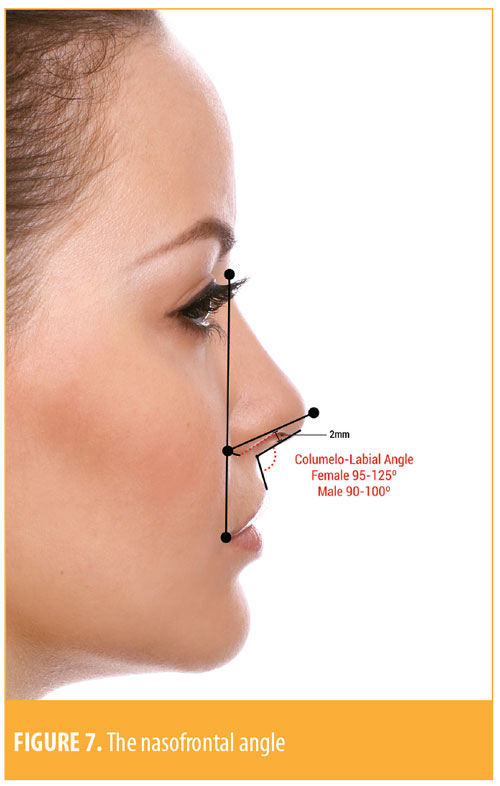
Next, the physician measures the columella labial angle (aCL). This is a tangent line of the columella crossing a line from the subnasal area toward the labial limb. The measurement of the columella labial angle in women is usually 95 to 125 degrees and, in men, 90 to 100 degrees. Therefore, the female ideal nose is more raised than the male nose.
We next measure the columellar-lobular angle, obtained through the intersection of a line parallel to the columella crossing a line drawn parallel to the lobe. This angle measures ideally 30 to 45 degrees. The smaller the angle, the more rectified, larger, and more rounded it will be, with a less natural appearance (Figure 7).
The base of the nose and nasal wings should be compared to the tip of the lobe and the nasal pyramid. The columella must be evaluated with regard to the position of the median line, alignment, width, length, and position in relation to the nasal wings. Finally, the cephalic head view is used to evaluate the nasal pyramid.
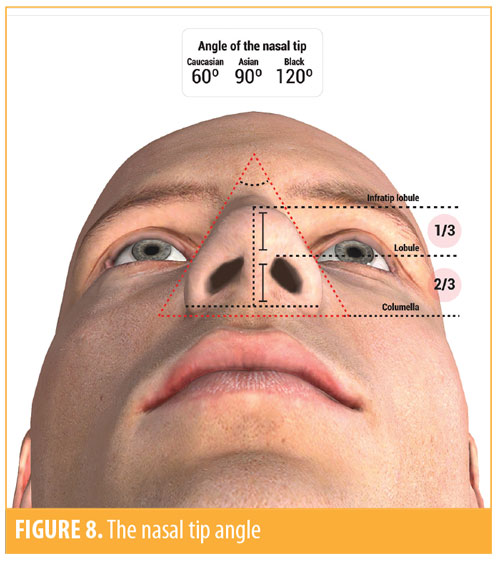
The angle of the nasal tip is calculated through the angle of the lobe toward the nasal wings. The smaller the angle, the narrower the nose; the larger the angle, the wider the nose. There is variation among angles between races: The nasal tip angle is generally 60 degrees in Caucasians, 90 degrees in Asians, and 120 degrees in people of African descent (Figure 8).
These measures and angles should be established and applied individually to each patient to correlate with the main indications of nonsurgical nasal filling, namely elevation or rectification of the tip or the nasal dorsum as a complement to surgical rhinoplasty, correction of asymmetries, or correction to posttraumatic deformities and/or congenital hypodevelopment.
Technique. After photographing with a three-dimensional digital device, the physicians should sterilize the area with 2% alcoholic chlorhexidine. A topical anesthetic with lidocaine spray 10% should then be applied. We prefer not to use a local anesthetic block, because this type of anesthesia can mask pain in the cases of vascular ischemia.
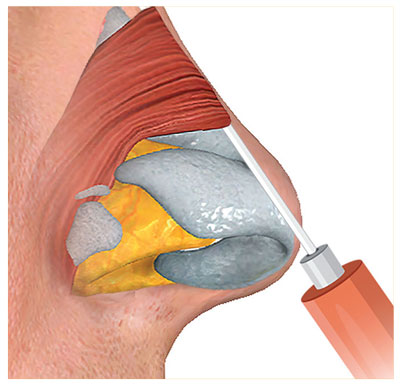
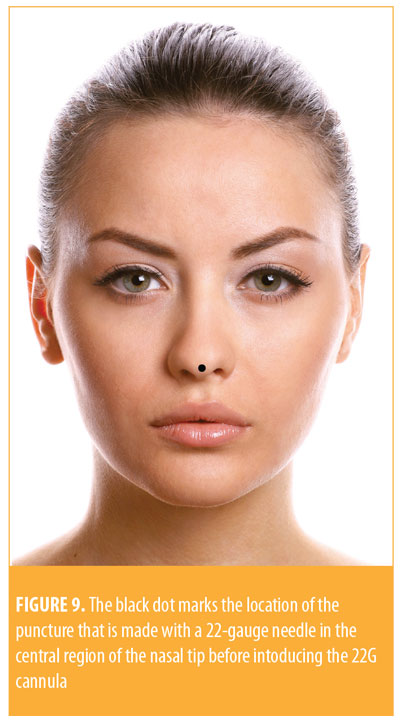
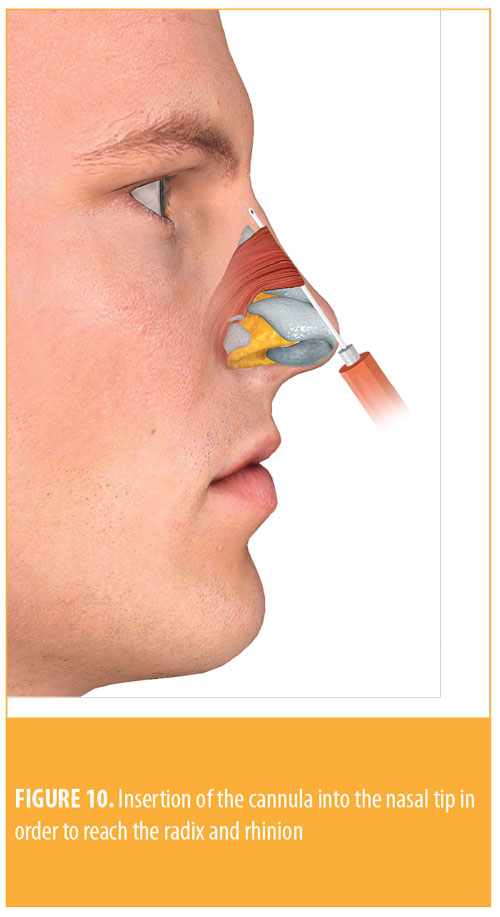
The product we use is a high density hyaluronic acid (20mg/mL). With this technique, a puncture is made with a 22-gauge (G) needle in the central region of the nasal tip in order to introduce the 22G cannula (Figure 9). First, the introduction is made toward the nasal bone crest, passing the septum to reach the lower part of the columella. This aims the projection of the nasal tip. In our patients, the filler is applied with a bolus technique on the bony crest after a retroinjection into the tip.
To reach the radix and rhinion, we insert the cannula through the same entry point in the nasal tip toward the radix and deposit a small bolus in this location (Figure 10). Then, a retroinjection is made along the dorsum, correcting dorsal humps or other asymmetries. If a correction in the higher part of the nose is required, an entry point can be made at the supratip for easier access.
After the end of the procedure, a sterile dressing is placed over the entry point site. A micropore is placed along the dorsum and around the tip to protect and maintain the remodeling. It is removed after 24 hours by the patient. The use of a transparent dressing helps with the identification of early complications (e.g, livedo or ischemia).
In the immediate post-procedure period, light local pain and ecchymosis in the entry point is expected. Edema and erythema have been observed up to 30 days post-procedure.
Results
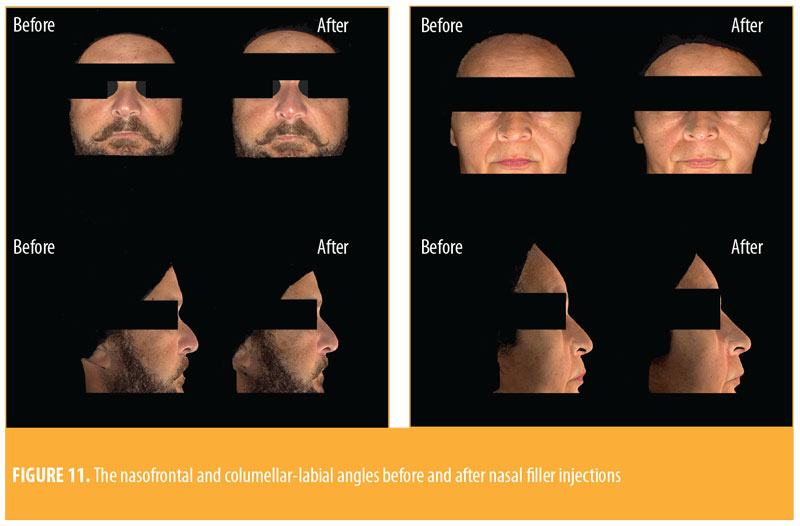
Among our patient sample, 41 of the 45 patients (91.1%) were women. The mean age of the patients was 38 years (22–69 years). The parameters used in this study were nasal length, nasal projection, columellar-labial angle, and frontal nasal angle. Based on the findings, the nasal length increased by an average of 0.1cm -0.5cm to +0.7cm) and the nasal projection increased by an average of 0.08cm (-0.3cm to +0.3cm). Additionally, the nasofrontal angle decreased by an average of 0.37 degrees, and the columellar-labial angle increased by an average of 5.97 degrees (Figure 11).
Complications. Nasal filling can have the same adverse effects and complications as those associated with fillers injected into other sites (Table 1). Major complications associated with this procedure include infection, vascular impairment due to direct injection or local compression, and blindness. The nose is particularly sensitive, as its vascularization has anastomoses with branches of the internal carotid, such as the ophthalmic artery. In addition, many patients who seek nasal fillings want to correct small defects that have remained after previous surgical procedures (e.g., rhinoplasty or septoplasty). In a large majority of cases, this results in a change in the vascularization of the region and certain areas of fibrosis, which might make the hyaluronic acid procedure more difficult, and in some cases, lead to intravascular injection, especially in the area of the nasal tip.
In our patient cohort, only one complication occurred. One patient reported a pustule with discrete pain that did not involve the entry point area. A fistula was diagnosed and treated with the extrusion of a small amount of the product that had remained in that area, which had made it difficult to close the entry point.
Discussion
Procedural considerations. Adequate knowledge of the proper techniques and patient anatomy is essential for the practice of nonsurgical rhinoplasty. Being proficient in the handling of the nasal filling from the beginning to the end—from indication to the recognition of any complications—is essential for a successful procedure. Although there is no definitive evidence for an ideal filler for use in the nasal region, hyaluronic acid has been increasingly used due to its longevity and rheological properties compared to other fillers.1 In our experience, hyaluronic acid is safe when the minimum quantity of the product needed for the patient is injected with a blunt-tip cannula. As opposed to a surgical procedure, we have the ability to perform nonsurgical rhinoplasty as many times as necessary due to the absorbability of hyaluronic acid.
In secondary rhinomodulations, hyaluronic acid injection should be done with caution and following a clinical evaluation that considers tissue distensibility and structural architecture. If tissue distensibility and structural architecture are greatly altered, it is not advisable to continue with the remodeling. Although these components are generally not significantly altered, the injection should still be done carefully and with the minimum quantity of the product due to the distortion of the local anatomy after the surgical rhinoplasty.
Corrections that aim to reduce bone, cartilaginous, or soft tissue structures are not possible with this method. In addition, it should be noted that nasal remodeling using hyaluronic acid will increase the structures and proportions due to the volumizing effect of the fillers.
Ideal nose shapes. The measurements of an ideal nose have been recorded since antiquity. Despite the variations over time, the mathematics and the way of calculating the ideal nose shape have not changed—only the standards of beauty. For the Greeks, a high radix is seen as beautiful, while among Brazilians, a low radix is the ideal profile.6
Procedural categories. Use of hyaluronic acid for nonsurgical rhinoplasty filling can be broadly divided based on three indications: dorsum enlargement, dorsum correction, or tip projection.7
The increase of the dorsum is indicated in patients who have a concave dorsum with a hump, producing an unrectified dorsum. Increasing the nasal tip is indicated in cases requiring the correction of bifid tips or for local projection.
The filling of the collumellar-labial angle is indicated in cases of low or fallen nasal tip, short columella, or bulging nasal dorsum. This procedure is equivalent to the insertion of a columellar structure in surgical rhinoplasty.1
Recognizing complications. The recognition of ischemia, the most dangerous complication, is critical. Signs of pallor, livedo, and/or local pain during or immediately after the procedure should be treated immediately with the application of hyaluronidase.
When performing the procedure, all structures of the nose—including the thicknesses and properties of the skin and soft tissue and the size, shape, and strength of the cartilage and bone—should be taken into account in order to avoid complications.
Conclusion
Nonsurgical rhinoplasty requires further study in order to determine its safety and efficacy.8 The nose is a region of complex anatomy, comprising several different tissues, and the use of hyaluronic acid in this area requires expert practice and technique. For this reason, careful evaluation of the nasal surgery site, with measurements of the ideal nasal proportions, is fundamental to ensure optimal and safe use of the filler. The use of hyaluronic acid can either be used as a concomitant or alternative procedure to rhinoplasty, and is emerging as an effective solution for minor corrections. This technique for minor corrections might improve patient satisfaction because immediate results can be seen following the procedure. The clinician must always consider not only the risk of complications, but also the severity of potential complications, and carefully weigh the aesthetic benefits of nasal injectables against any potentially devastating risks.
References
- Daher JC. Columellar rhinoplasty: a new vision with the use of solid silicone. Rev Bras Cir Plást (Impr). 2010;25(3):450–457. Article in Portuguese.
- Furtado IR. Nasal morphology – harmony and proportion applied to rhinoplasty. Rev Bras Cir Plást. 2016;31(4):599–608. Article in Portuguese.
- Augusto GG, Shiro T, Serra GG, et al. Aesthetic comparison of the ideal nasal radix height in a Brazilian population. Braz J Otorhinolaryngol. (Impr). 2011;77(3):334–340. Article in Portuguese.
- Neligan PC. Analysis and nasal anatomy. Plastic Surgery. Philadelphia, PA: Elsevier; 2012: 373–386.
- Aston SJ, Steinbrech DS, Walden JL. Aesthetic Plastic Surgery. Philadelphia, PA:Elsevier;2012:437.
- Augusto GG, Shiro T, Serra GG, et al. Aesthetic comparison of the ideal nasal radix height in a Brazilian population. Braz J Otorhinolaryngol (Impr). 2011;77(3):334–340.
- Youn SH, Seo KK. Rhinoplasty evaluated by anthropometric analysis. Dermatol Surg. 2016;42(9):1071–1081.
- Wang LL, Friedman O. Update on injectables in the nose. Curr Opin Otolaryngol Head Neck Surg. 2017;25(4): 307–313.

