 J Clin Aesthet Dermatol. 2021;14(5):E70–E79.
J Clin Aesthet Dermatol. 2021;14(5):E70–E79.
by Je-Young Park, MD; Frank Lin, MBBS; Atchima Suwanchinda, MD; Rungsima Wanitphakdeedecha, MD; Jonathan Yu, MD; Ting Song Lim, MD; Jeng Feng Chen, MD; Wilson Ho, MD; Joyce Lim, MBBS; Lanny Juniarty, MD; Yong Seng Kee, MD; Seong Jae Youn, MD; and Sabrina Fabi, MD
Dr. Park is with the Apkoo-Jung Department of Oracle Dermatology Center in Seoul, South Korea. Dr. Lin is with Eastern Plastic Surgery in Melbourne, Australia and the Department of Plastic Surgery at Eastern Health Box Hill Hospital in Melbourne, Australia. Dr. Suwanchinda is with Medisci Biointegrative and Antiaging Center in Bangkok, Thailand. Dr. Wanitphakdeedecha is with the Department of Dermatology, Faculty of Medicine at Siriraj Hospital, Mahidol University in Bangkok, Thailand. Dr. Yu is with JY Dermatology & Aesthetic Center in Manila, Philippines. Dr. T. Lim is with Clique Clinic in Kuala Lumpur, Malaysia. Dr. Chen is with Beauté J’adore Dermatology and Esthetic Medicine in Taipei, Taiwan. Dr. Ho is with The Specialists: Lasers, Aesthetic & Plastic Surgery in Hong Kong. Dr. J. Lim is with Joyce Lim Skin and Laser Clinic in Singapore. Dr. Juniarty is with Miracle Aesthetic Clinic in Surabaya, Indonesia. Dr. Kee is with Premier Clinic in Kuala Lumpur, Malaysia. Dr. Youn is with Leaders Dermatology Clinic in Seoul, South Korea. Dr. Fabi is with Cosmetic Laser Dermatology and the Department of Dermatology, University of California in San Diego, California.
FUNDING: Funding for the preparation of this manuscript was provided by Merz Asia Pacific Pte. Ltd to Dr. Shawna Tan, Medical Writers Asia.
DISCLOSURES: Dr. Fabi is a speaker, consultant, and investigator for Galderma, Merz, Allergan, and Bausch Health. Dr. Yu is an advisory board member for Merz Philippines Healthcare Inc. and has received compensation for travel expenses. The other authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Background: Noninvasive facial-rejuvenation devices, such as nonablative radiofrequency (RF) and laser-assisted technology, are increasingly replacing higher-risk surgeries for face and body skin laxity.
Objective: We sought to review published information on noninvasive energy device safety and efficacy in aesthetic skin tightening, compare these with our experiences in Asian patients, and disseminate a consensus for optimizing microfocused ultrasound with visualization (MFU-V) in Asian patients.
Methods: A broad, nonexhaustive, nonsystematic literature search of published studies indexed in PubMed was performed to compare selected energy technologies to MFU-V for noninvasive face and body skin tightening, in particular, among Asian patients. This was supplemented with internal documents to provide evidence and support arguments if no peer-reviewed data were available.
Results: We highlighted the differences between devices and platforms and identified factors requiring attention and caution. Due to the increase in new devices lacking strong supporting clinical evidence of both safety and efficacy in Asia, it is necessary to convene physicians with substantial experience in MFU-V and devise a consensus on Asian patient selection, treatment planning, and customization.
Conclusion: Many platforms duplicate or claim similar technologies, efficacy, or safety without significant peer-reviewed scientific or clinical evidence. We showed that MFU-V satisfies this clinical imperative. Further, the patented DeepSEE® technology allows users to noninvasively “see” through the skin to ensure treatment precision, facilitate optimal skin lifting and tightening, and enhance patient comfort and safety. Therefore, we believe that MFU-V is the gold standard for nonsurgical lifting and skin tightening.
Keywords: Nonsurgical skin tightening, energy device, MFU-V, HIFU, Asian
Face and body skin laxity cannot be improved with diet and exercise alone.1 The International Association for Physicians in Aesthetic Medicine recently noted that noninvasive facial-rejuvenation devices, such as nonablative radio-frequency (RF) and laser-assisted technology, are increasingly replacing higher-risk surgeries for these problems.2
Monopolar RF and intense focused ultrasound (IFU) are noninvasive, energy-based technologies for facial lifting, tightening, and contouring. IFU devices use transducers to concentrate variable acoustic or ultrasound energy within a small, targeted, subcutaneous tissue area, such as the superficial musculoaponeurotic system (SMAS).3 The target tissue is heated to more than 65°C, denaturing proteins in the area almost immediately, leading to the contraction of collagen fibers4 and stimulating de-novo neocollagenesis that lifts and tightens skin. IFU devices include those using high-intensity focused ultrasound (HIFU) or microfocused ultrasound with visualization (MFU-V). Ultherapy® (Merz North America, Inc., Raleigh, North Carolina), also known as MFU-V, is cleared by the United States (US) Food and Drug Administration (FDA) for the noninvasive lifting of the brow,5,6 neck, and submentum,6 and for relieving décolleté wrinkles and lines.7 Meanwhile, the European Union has cleared MFU-V for upper and lower face, neck, and décolleté contouring and lifting.8 None of the available IFU devices are as robustly supported by clinical evidence as MFU-V, making MFU-V the current gold standard for noninvasive skin lifting.43 MFU-V delivers low-energy MFU (0.4–1.2 J/mm2) to three different depths—1.5mm, 3.0mm, and 4.5mm—to heat target tissues from superficial skin to SMAS.5 This heat creates 1-mm3, inverted cone-shaped microthermal lesions down to the 5-mm-deep reticular layer of the dermis and subdermis without harming the overlying papillary dermal and subdermal layers.9 MFU-V can therefore be used to tighten and lift the SMAS and treat wrinkles or sagging skin in the face, neck, and décolleté.10 One distinctive feature of MFU-V is its capacity for real-time visualization up to 8.0mm, which HIFU lacks.3,8 While HIFU and RF systems rely on the somewhat blind application of energy, MFU-V incorporates a real-time, high-resolution ultrasound imager, which lets users simultaneously “see and treat” distinct tissue layers, including the SMAS, subcutaneous fat, dermis, and epidermis. Table 1 summarizes the differences between HIFU and MFU-V. 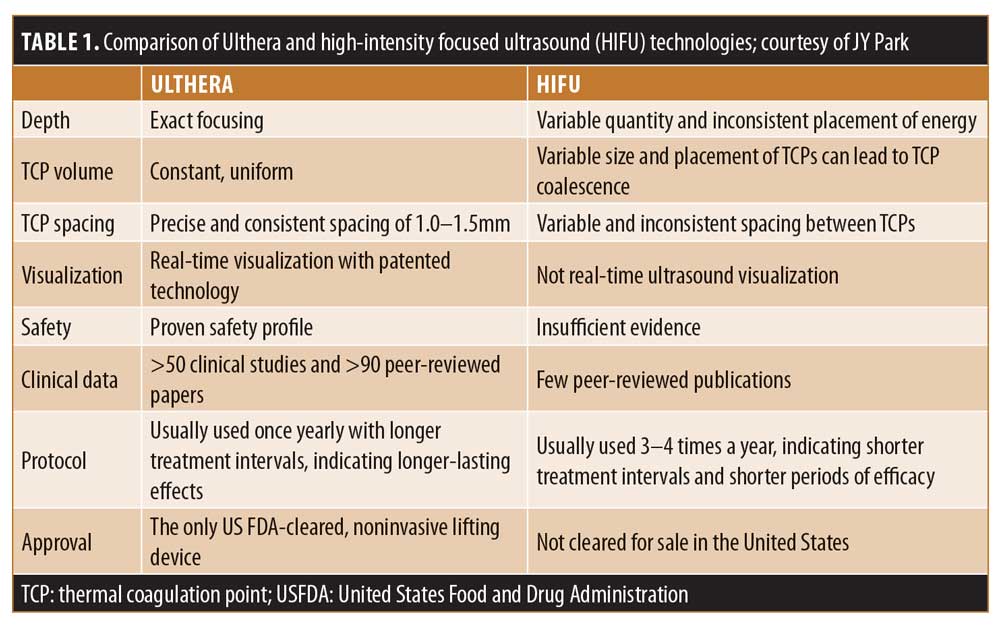
In Asia, popular monopolar RF technologies include the Thermage (Comfort Pulse Technology, Solta Medical Hayward, California), ThermiTight (ThermiAesthetics, Southlake, Texas), and TruSculpt (Cutera, Inc., Brisbane, California) systems. All energy devices11–14 are associated with some adverse events, such as poor RF technique leading to blistering and crusting.15,16 When emitted RF heat energy traveling through tissue is impeded by adipocytes, it localizes within the obstructing cells and thermolyzes them1 but can also induce dermal regeneration through neocollagenesis and elastogenesis, producing skin tightening.17
Ulthera’s DeepSEE® technology works in dual stages, with an immediate tissue-lifting effect followed by a wound-healing response. First, MFU energy is concentrated in dermal and subcutaneous tissues, causing collagen fibrils within them to heat to 60°C to 70°C, creating focal points of thermal injury known as thermal coagulation points (TCPs).9,18,19 These temperatures are optimal for the collagen fibril contraction and denaturation that produces the initial lift. Wound healing in the second stage induces neocollagenesis for tissue remodeling. From 48 hours until 10 weeks after treatment,20 inflammation also stimulates neocollagenesis, fibroblast proliferation, and elastogenesis around the TCPs. By Day 28, the adjacent dermis undergoes remodeling and viscoelasticity increases. Over time, the tissue lifts and the skin thickens and tightens, further increasing elastin in the injury zone and collagen in the reticular dermis.21 Ten weeks after treatment, neocollagenesis22 completely replaces the existing collagen in treated areas with thermal injury,20 further tightening and lifting the skin in a sustained remodeling phase that can last for up to one year. The availability of six MFU-V transducers allows customization to three different tissue depths—4.5mm, 3.0mm and 1.5mm—below the skin. Narrow transducers (10 MHz/1.5 mm and 7.0 MHz/3.0 mm) are also available for smaller areas and can be used alongside the wider transducers. Individual variations in tissue thickness can be visualized through MFU-V and, with the availability of transducers targeting different depths, physicians can now customize treatments based on skin thickness. MFU-V can be used at more than one tissue depth per treatment session, and multiple studies show that both single- and dual-depth treatments improve, tighten, or regenerate sagging skin on the face, neck,5,23–30 abdomen,31 knees,31,32 upper arms,31 thighs,31 buttocks,33 and elbows.34
A Gold-standard Device with Real-world Evidence in Clinical Practice
The MFU-V device includes real-time ultrasound imaging that targets specific tissue layers and avoids critical structures, such as bone and blood vessels. By merely adjusting standardized algorithms and optimizing MFU energy levels and line densities, tissues in multiple planes can be lifted and tightened. In one author’s practice, prioritizing comfort and satisfaction led to 60 percent of patients returning for repeat treatments.35 Recent publications and consensus guidelines have also made recommendations supporting the tailoring of MFU-V treatments to each patient. For example, the “See-Plan-Treat” tool visualizes tissue planes and anatomies before a personalized, tissue-targeting strategy for MFU delivery is devised. The tool was found to improve treatment comfort, efficacy, and success.36
A range of MFU-V transducers is available to target MFU to the different tissue depths of the SMAS/fibrous and dermal layers,30 with dual-depth treatments found to produce superior outcomes.27 For dual-depth treatments, the manufacturer recommends targeting the superficial fascial/SMAS and deep dermal layers. A significant brow lift was achieved in 86 percent of patients 90 days after MFU-V was applied to the whole face and neck at 4.5mm and 3.0mm.37 In the submentum, almost 73 percent of patients had visible submental lift of greater than 20.0mm2, which persisted in nearly 69 percent of subjects at three months.28 We observed skin laxity improvements in almost 78 percent of patients receiving face and neck MFU treatments, with results persisting in 67 percent of patients 180 days later.38 After 90 days, MFU-V also significantly improved the décolleté in 46 percent of patients with moderate-to-severe rhytids, and 62 percent of these patients showed sustained improvement at 180 days.39 Of patients receiving multiple MFU-V passes during dual-depth treatments, 58.1 percent also had improved cheek and submental skin laxity and jawline definition at 90 days posttreatment, with improved lower face and neck in 65.6 percent of patients.28 MFU-V results are long-lasting, as shown by the relief of marionette folds40 and improved lower face and neck skin laxity at one38,41 and even two years42 posttreatment.
By applying our gold-standard consensus recommendations43 of using the highest tolerable MFU energy setting, but reducing this according to patient comfort while maintaining the necessary density of treatment lines, patients only experience mild discomfort. A split-face study on marionette lines found that using higher MFU energies (in other words, delivering greater line densities or using higher energy levels) and more treatment planes (or two or three tissue depths) led to more significant tissue lifting and elasticity.38 Treating just a single depth is unlikely to give the ideal TCP density for effective treatments and may cause stacking of TCPs, thus leading to adverse events. Table 2 demonstrates that variations in protocol facilitate treatment success when physicians use MFU-V with a good understanding of facial anatomy and Ulthera technology and understand how to optimize outcomes.43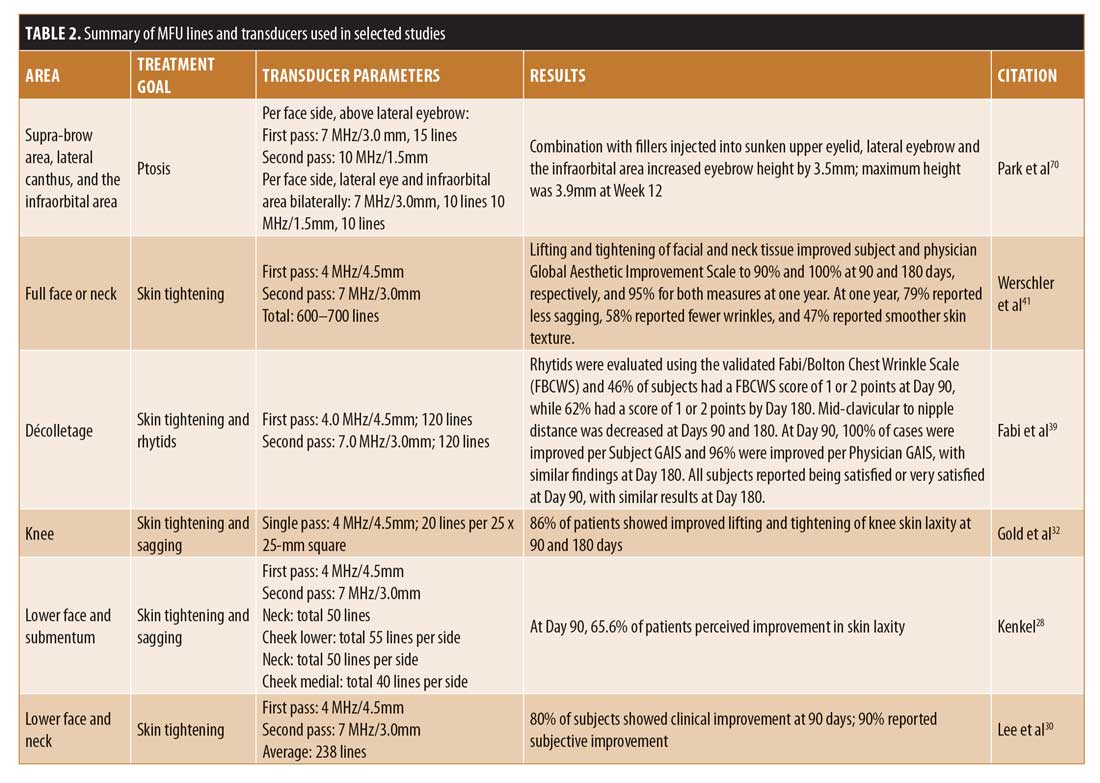
Our Experience with Noninvasive Skin-tightening Devices in Asian Patients
DeepSEE® technology uses real-time ultrasound to analyze parameters in skin images, such as skin thickness and tissue echogenicity. A treatment line over the image demonstrates where MFU will be placed relative to the tissue layers, ensuring that MFU is delivered only to the intended layer and nowhere else (Figure 1A). Ulthera’s high-resolution, real-time visualization of dermal and subdermal layers facilitates optimal transducer selection and proper transducer coupling to the skin before MFU is applied. The thickness of ultrasound gel layers will affect the final treatment depths, which can be used to tailor treatments in thin-skinned patients where even the most superficial transducers fail to reach optimal treatment depths. Care is necessary to avoid treating too superficially, however, as burns can occur.44,45 This highlights the importance of being able to make fine adjustments to gel layer thickness so that MFU can be placed either slightly above or below the set transducer depth.25 It also underscores the necessity of visualizing tissue depths.46 Moreover, Asian patients, who have denser SMAS, deep fascia connections, and thinner skins with lipid-rich stratum corneum,46 will benefit from tissue visualization, as this increases the accuracy of MFU placement.
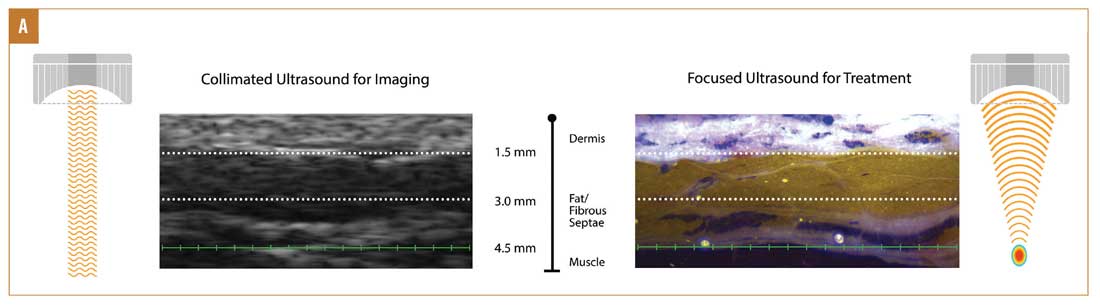
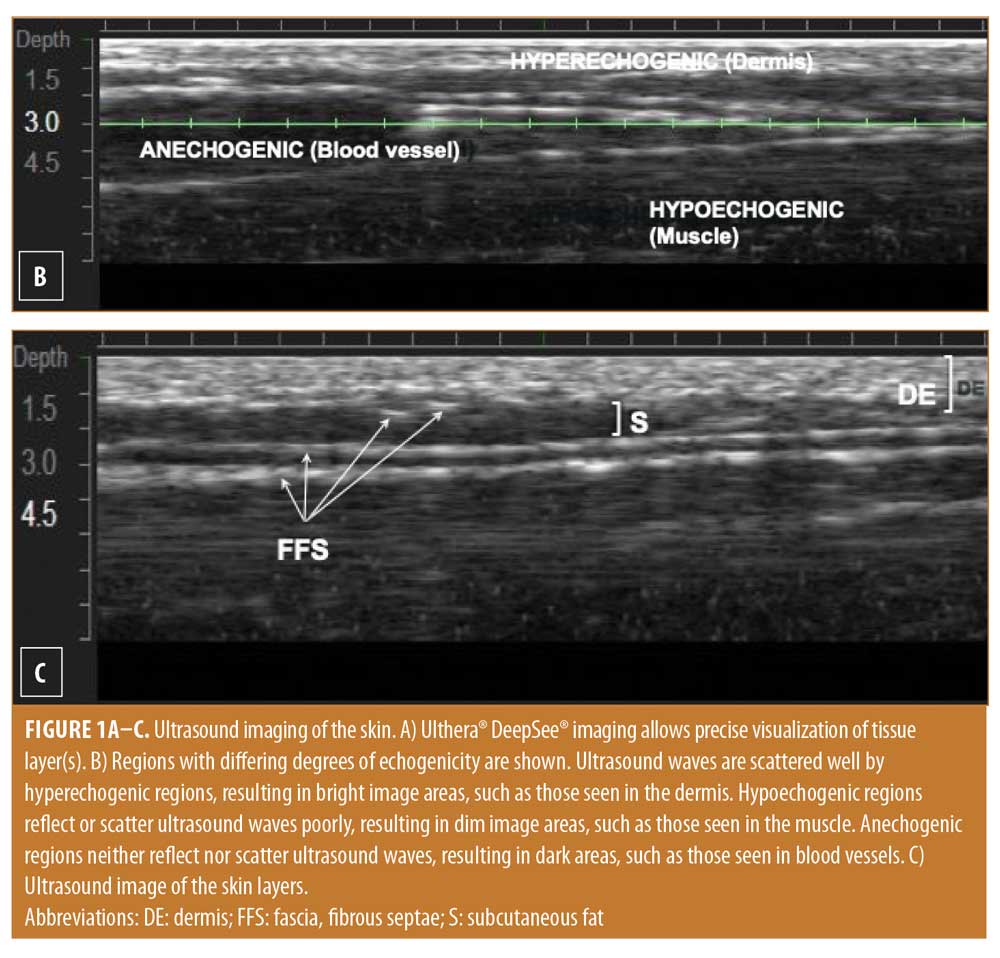
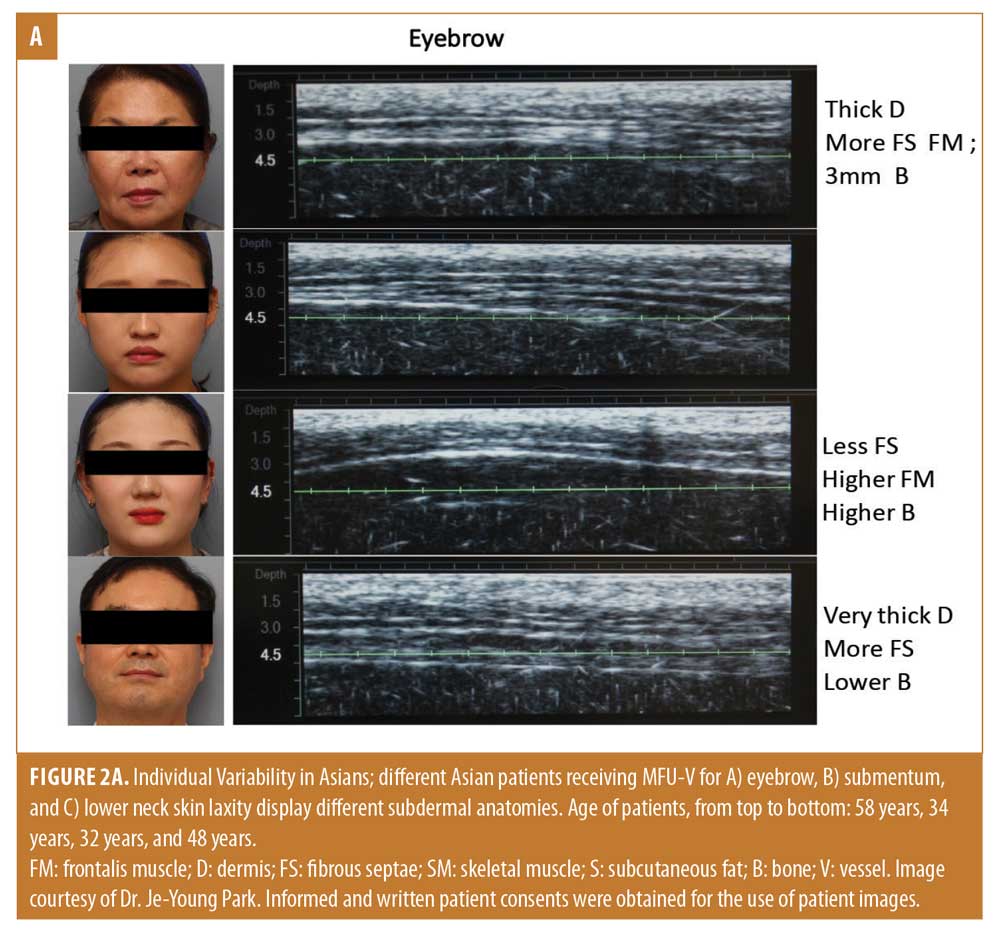
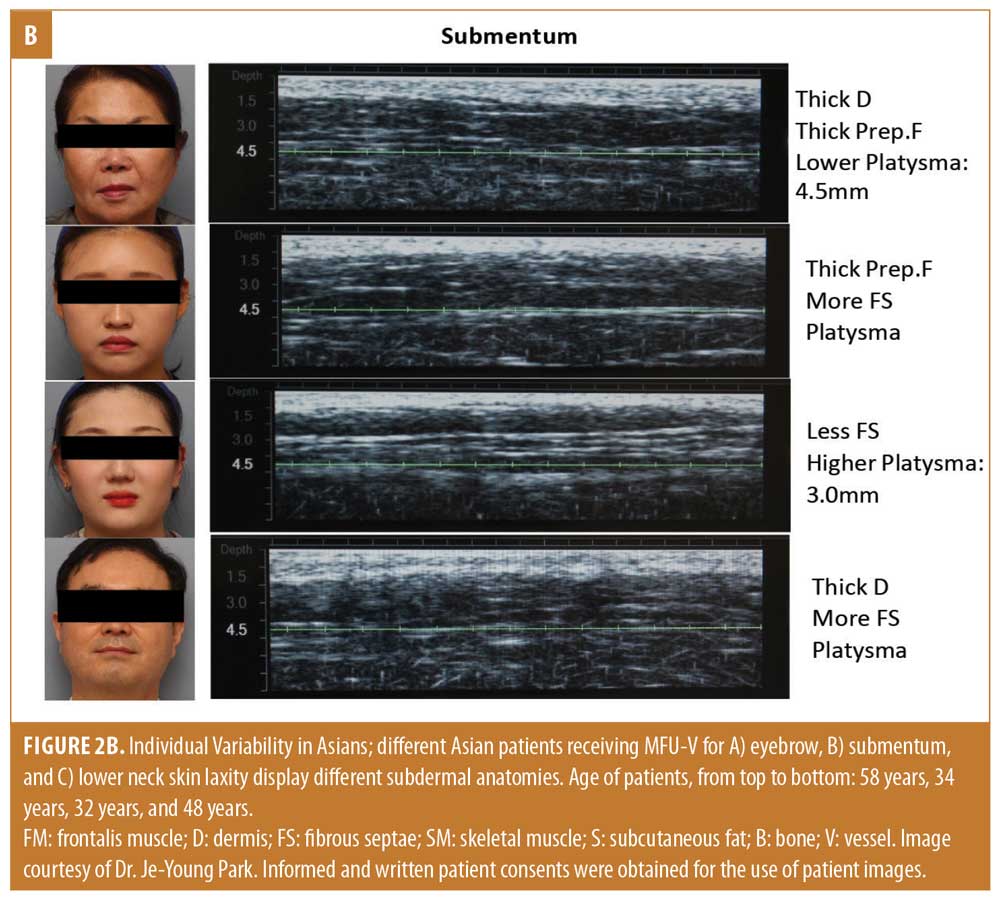
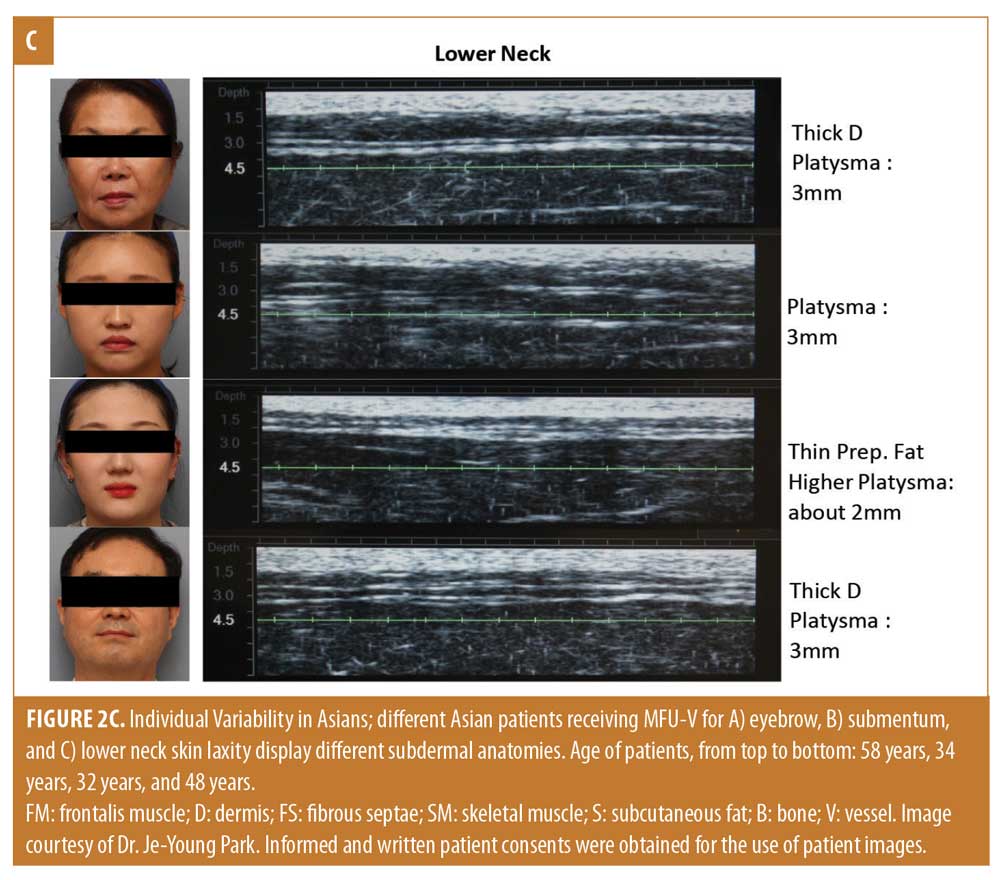
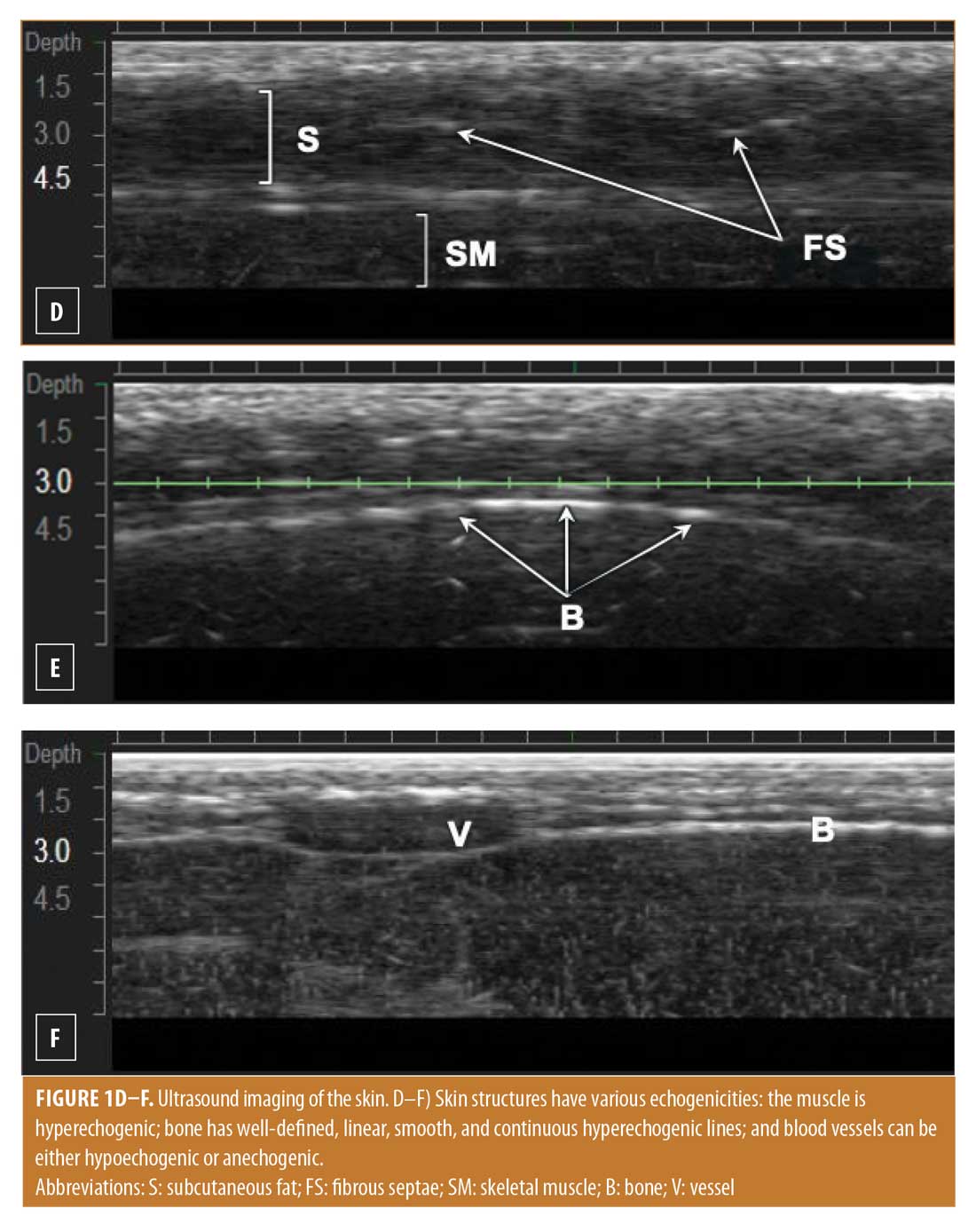 In Asian patients, MFU-V outcomes can be affected by the different protocols available. Lee et al30 used 4-MHz/4.5-mm and 7-MHz/3.0-mm transducers to deliver an average of 238 lines in the dermal and fibrous layers of the lower face and neck, resulting in improvements for 90 percent of patients at 90 days posttreatment. Jung et al47 used a 4-MHz/4.5-mm transducer on Korean patients to deliver 100 to 120 lines for facial tightening. Thus, even with variable line numbers and transducer strengths, MFU-V consistently produces successful outcomes (summarized in Table 2 for selected anatomical sites). MFU-V offers an unrivaled level of precision by leveraging the variable echogenicity (i.e., the ability to reflect or scatter ultrasound waves) of the different tissue layers (Figures 1B–1F). Under ultrasound, the dermis and epidermis display homogenously bright areas.48,49 Normal, collagen-rich fascia appears as continuous, bright, and linear structures bordering fat and muscle. Subcutaneous fat creates bands with varying thickness, whereas fibrous septae appear as short, curvilinear, bright lines or specks. The thinner upper dermis can be distinguished from the lower dermis on ultrasound as it has fewer collagen fibers. The thin papillary dermis layer only weakly reflects ultrasound and thus echoes less than thicker, collagen-rich, lower dermis tissues. As such, the upper papillary layer can be differentiated from the lower reticular dermis layer on ultrasound. Blood vessels do not reflect ultrasound waves and appear as dark areas. Figure 2 illustrates the variations in subdermal anatomies for four Asian patients receiving MFU-V in equivalent anatomical areas. Physicians can leverage this information to accurately diagnose patients and target MFU.
In Asian patients, MFU-V outcomes can be affected by the different protocols available. Lee et al30 used 4-MHz/4.5-mm and 7-MHz/3.0-mm transducers to deliver an average of 238 lines in the dermal and fibrous layers of the lower face and neck, resulting in improvements for 90 percent of patients at 90 days posttreatment. Jung et al47 used a 4-MHz/4.5-mm transducer on Korean patients to deliver 100 to 120 lines for facial tightening. Thus, even with variable line numbers and transducer strengths, MFU-V consistently produces successful outcomes (summarized in Table 2 for selected anatomical sites). MFU-V offers an unrivaled level of precision by leveraging the variable echogenicity (i.e., the ability to reflect or scatter ultrasound waves) of the different tissue layers (Figures 1B–1F). Under ultrasound, the dermis and epidermis display homogenously bright areas.48,49 Normal, collagen-rich fascia appears as continuous, bright, and linear structures bordering fat and muscle. Subcutaneous fat creates bands with varying thickness, whereas fibrous septae appear as short, curvilinear, bright lines or specks. The thinner upper dermis can be distinguished from the lower dermis on ultrasound as it has fewer collagen fibers. The thin papillary dermis layer only weakly reflects ultrasound and thus echoes less than thicker, collagen-rich, lower dermis tissues. As such, the upper papillary layer can be differentiated from the lower reticular dermis layer on ultrasound. Blood vessels do not reflect ultrasound waves and appear as dark areas. Figure 2 illustrates the variations in subdermal anatomies for four Asian patients receiving MFU-V in equivalent anatomical areas. Physicians can leverage this information to accurately diagnose patients and target MFU.
There are few peer-reviewed publications on the efficacy and safety of alternative HIFU devices, including Korean devices such as the Ultraformer® III (Classys Inc., Seoul, Korea), Ultraskin™ (WONTECH Co., Daejeon, Korea), and Doublo™ (HIRONIC Co., Sungnam, Korea).21,50–52 While MFU-V has been de-novo cleared by the US FDA for noninvasive lifting since 2009, Ultraformer III has been approved by the Korean FDA since 2012, but lacks US FDA clearance. There is no published evidence to support the manufacturer’s claims that Ultraformer III creates skin coagulation points within target tissue layers at approximately 65.4°C,53 contrasting starkly with MFU-V’s peer-reviewed data showing its consistent heating of tissue to 60° to 70°C. 54,55 Moreover, MFU-V’s thermal coagulation points are precisely spaced and consistently placed at specific depths without surface disruption; there is no information for how or if this occurs with the Ultraformer III. Clinical data on the efficacy and safety of the Ultraformer III device are also limited, with only one published clinical trial for the face, another for both the face and body, and a third on a pilot study for the body. 28,38,56–59
The Doublo system has three transducers with energy levels that claim to target either the upper dermis, deep dermis, or SMAS. In contrast, MFU-V’s six transducers target three tissue depths (4.5, 3.0, and 1.5mm) and offer adjustable energy levels. One Doublo study found it to be less effective for noninvasive skin tightening and skin rejuvenation than another study,60 and attributed this inconsistency to the use of different Doublo devices. Such limited data and erratic practices force physicians to make decisions based on unreliable scientific evidence. We observed unintended outcomes following HIFU in a 56-year-old female patient, who underwent two HIFU (device name and model unknown) treatments over a three-month period before presenting to the author’s clinic after six months (Figure 3A–B). She developed tear trough bulging, tear trough aggravation, sunken cheeks, and increased skin laxity, all of which were caused by excessive and uncontrolled delivery of HIFU to the superficial or deep fat layers. A second, 35-year-old female patient also developed adverse effects five months after receiving 400 lines of HIFU (Figure 3C–D) and presented to the author’s clinic with skin laxity and crepiness, tear trough aggravation, sunken cheeks, and periorbital and perioral fine lines. We also caution that these cases represent only the milder consequences of suboptimal HIFU treatment.

In contrast, the safety and efficacy of MFU-V is supported by more than 50 clinical studies and 90 peer-reviewed publications, both independent and company-sponsored, with patients of various ethnic groups, sexes, ages, and follow-up durations. Additionally, more than 1.5 million treatments with MFU-V have been performed globally (as of June 2019).61 Our recent consensus highlighted MFU-V’s high precision at TCP formation and targeting specific tissue depths and its demonstrated safety profile.43 While we found that 800 to 1,200 lines were optimal for full-face and neck treatments, we also stressed that this should be customized to patient needs, face size, skin laxity, fat distribution, skin quality, and ultrasound image results. Ultrasound imaging should be performed to estimate SMAS depths relative to superficial skin depths and for the correct transducers and number of lines for each tissue plane to be determined.
Users should be wary of the entry of cheaper, copycat, and counterfeit devices from East Asia into clinics worldwide.62 Many of these devices lack system feedbacks, fail-safes, or manufacturer assurances of safety, reliability, or reproducibility. Most have not undergone comprehensive, long-term testing in multiple clinical trials for safety and efficacy.63 Copycat devices can cause serious adverse events. For example, copycat cryolipolysis systems have caused burns and freeze injuries63 while some HIFU systems have caused corneal stromal damage.64 Without the exacting and rigorous standards of clinical studies, it is difficult to establish clear guidance to prevent improper techniques or untested protocols.
Personalization is Important
Deep tissue visualization is important for precision, consistency, and safety of aesthetic treatments. Ulthera DeepSEE® ultrasound imaging enables physicians to see, in real-time, the target tissue layer. No other FDA-cleared, nonsurgical energy device has this visualization capability. As inaccurate energy delivery can be detrimental, users must correctly identify the SMAS or superficial fascia layers, whose depths can differ depending on patient weight, body mass index, age, sex, and target area.65,66
Though research is needed to confirm our observations, in the authors’ clinical experience, the efficacy of the results are determined by the quality of energy delivered, which is also affected by depth, temperature, volume, and precision. Per their clinical experience, skin burns, scars, and longer recovery times can result from the delivery of too much ultrasound energy and, thus, high temperatures, or from the creation of excessively large or inconsistently spaced TCPs. Burns can also result from ultrasound energy delivered at too-shallow depths. Poor coupling of the transducer to skin or stacking of energy pulses can also cause burns. Treatment efficacy is affected by low energy and temperature levels, targeted tissue depths being too deep and affecting bone, or failure to create TCP due to imprecise delivery. These factors all affect the optimum temperature required for collagen denaturation and subsequent neocollagenesis. Also, TCPs that are too small can only treat low volumes of tissue, thus reducing efficacy. These observations require additional research before firm conclusions can be made.
Synergistic combinations of multiple aesthetic modalities enhance the efficacies of individual ones, and multimodality approaches incorporating MFU-V are recommended in position statements, consensus documents, clinical studies, and trials.67–71 MFU-V augments the effects of neuromodulators, biostimulators, and fillers, and can achieve natural results when used judiciously to avoid overtreatment.67 MFU-V can tighten and strengthen an area of skin before fillers are placed there, while also enhancing their volumization or collagen-stimulating effects, such as during cellulite or atrophic acne scarring treatments.71–75 Delivery of MFU energy over areas injected with hyaluronic acid and calcium hydroxylapatite (CaHA) fillers does not change filler appearances, increase inflammation, or induce product migration but can increase collagen fiber density and thickness.74,76 The upper face can be treated first with MFU-V to tighten skin and lift ptotic brows, followed by botulinum toxin A (BoNT/A) to relax brow depressor muscles, and fillers to correct temporal hollowing and forehead contours.68 Because MFU-V’s dual-phase mechanism of action delays neocollagenesis so that tissue lifting occurs later, this combination approach improves eyebrow heights, eyebrow ptosis, infraorbital hollows, and superior sulcus deformities, even at 12 weeks posttreatment.70 In the midface, fillers can reinflate fat pads and address depleted cheek volume and lost bony support, while MFU-V can lift and tighten the zygomatic-buccal retaining ligaments. Combining different modalities also effectively improves the nasolabial folds, melolabial fold, and jawline. Further, MFU-V improves ultraviolet B-induced pigmentation, which might be an adjunct benefit and new indication for facial rejuvenation.79
In August 2019, expert dermatologists and plastic surgeons from the Asia-Pacific region convened in Kuala Lumpur, Malaysia, to discuss and come to a consensus regarding recommendations for patient selection, treatment planning, and customization when using MFU-V. The recommendations are summarized henceforth.
Treatment plans should be personalized for optimal outcomes. Target areas must be mapped, and patients must be selected correctly. Those unsuitable for MFU-V should be offered alternatives, such as surgery. Patient customizations should include demographic considerations, such as age, body mass index, the number of treatment lines, energy settings, and treatment depths;43 the treatment strategy, as determined by the patient’s goal(s) of restoration, prevention, or maintenance; and safety considerations. The individualized aging pathology should also be assessed before treatment. Ultrasound imaging should be performed to enable the correct selection of transducer depths and line numbers. Higher-density treatments (i.e., more lines per depth) lead to more ideal outcomes; older patients might need multiple treatments to achieve desired outcomes and more frequent treatments to maintain results. Although a treatment interval of 12 to 18 months is effective for maintenance,43 this can be adjusted according to age. Younger patients (30–45 years) and those seeking early intervention or rejuvenation might require retreatment at longer intervals, such as every 24 months, while older patients (>50 years) might need treatments every 12 months. Physicians should tailor their strategies to each patient’s age and clinical conditions.
Patient comfort must be well managed. MFU-V discomfort varies between patients and depends upon the area being treated.5 As with all other energy-based procedures, no standard regimen for pain management exists. Nevertheless, transdermally-delivered lidocaine 4%/benzocaine 20% or compounded lidocaine 23%/teracaine 7% are effective at mitigating discomfort during MFU-V treatment.78 With fewer treatment pauses (due to less patient discomfort), treatment efficacy is improved. All experts agreed that even when trying to achieve the required treatment density (or the number of lines of MFU), using a lower MFU energy level improves patient comfort and produces better outcomes than treatments performed at maximum energy levels, which risk patients dropping out midway. While pain and comfort management are essential to ensure treatment adherence, patient education is also necessary to ensure patient satisfaction. Moreover, a positive treatment experience increases the likelihood of patients returning for future treatments.
Visualization is important for safety. Clinicians must recognize when patients unknowingly encounter counterfeit aesthetic devices and injectables—for example, when they receive less expensive treatments—and be equipped to deal with such situations. Using counterfeit or copycat systems that image tissues incorrectly, or that do not image tissues at all, can damage nerves, blood vessels, and muscles, or cause burns that lead to permanent scarring, thus compromising patient safety.
The Future of Skin Tightening
Aside from facial skin tightening and lifting, MFU also benefits lax skin on limbs, such as the knees, thighs, elbows, and upper arms, as well as the buttocks.31–34 Using MFU-V alongside CaHA fillers on the buttocks and thighs, neocollagenesis was induced and found to improve skin laxity and the appearance of cellulite.74 To assess its effects on the abdomen, one of our authors evaluated MFU-V for skin and soft tissue laxity in patients at six to 24 months postpartum.79 Patients were treated in an area of the anterior abdominal wall between the umbilicus superiorly, the anterior superior iliac spines laterally, and the symphysis pubis inferiorly. Twenty patients received a total of 1,140 lines each, delivered using the 4-MHz/4.5-mm transducer to target Scarpa’s fascia, the 7-MHz/3.0-mm transducer for Camper’s fascia, and the 10-MHz/1.5-mm transducer on dermal and subdermal layers. In addition, one patient received 540 lines on the right hemi-abdomen six weeks before a previously planned abdominoplasty. The patient’s left hemi-abdomen was maintained as a control for comparative histological analysis and intraoperative evaluation of tissue layers. Statistically significant improvements in lower abdominal wall laxity and excellent patient satisfaction were reported. Pretreated hemi-abdomen tissues exhibited neocollagenesis, fibrous septae thickening, and adipocyte sparing as compared with the untreated control hemi-abdomen. Seventeen patients experienced mild postprocedural pain, which resolved after four days with no significant adverse events. Thus, MFU-V was found to be safe and effective in improving abdominal skin laxity in postpartum patients and would suit other areas with well-defined superficial fascial systems.
Since its initial success at skin lifting and tightening in the brow in 2009, continued clinical development and study of MFU-V means that it is now poised for use in even more anatomical areas and indications. We envisage that its users will continue to drive innovations, including its combination with diluted CaHA, which can produce synergistic aesthetic effects and enhance neocollagenesis.
Conclusion
Unlike other platforms that claim similar technologies, efficacy, or safety, only MFU-V is backed by an extensive body of peer-reviewed, published scientific and clinical evidence, and only MFU-V has the patented DeepSEE® technology which allows users to noninvasively see through the skin. With this unparalleled ability to visualize specific tissue planes, clinicians can precisely deliver MFU energy for optimal lifting and tightening. Patient comfort and safety are enhanced as MFU-V causes less downtime and discomfort than traditional, face-lift surgeries and is therefore ideal for the many patients who now demand time-efficient, noninvasive, and durable solutions.
References
- Park JH, Kim JI, Park HJ, Kim WS. Evaluation of safety and efficacy of non-invasive radiofrequency technology for submental rejuvenation. Lasers Med Sci. 2016;31(8): 1599–1605.
- IAPAM. Aesthetic trends in 2019 & 2018 according to the IAPAM. Available at: https://iapam.com/aesthetic-trends-2019-iapam.html Accessed February 27, 2020.
- Fabi SG. Noninvasive skin tightening: focus on new ultrasound techniques. Clin Cosmet Investig Dermatol. 2015;8:47–52.
- Ferraro GA, De Francesco F, Nicoletti G, et al. Histologic effects of external ultrasound-assisted lipectomy on adipose tissue. Aesthetic Plast Surg. 2008;32(1):111–115.
- Alam M, White LE, Martin N, et al. Ultrasound tightening of facial and neck skin: a rater-blinded prospective cohort study. J Am Acad Dermatol. 2010;62(2):262–269.
- Brobst RW, Ferguson M, Perkins SW. Ulthera: initial and six month results. Facial Plast Surg Clin North Am. 2012;20(2):163-76.
- Fabi SG, Goldman MP, Dayan SH, et al. A prospective multicenter pilot study of the safety and efficacy of microfocused ultrasound with visualization for improving lines and wrinkles of the décolleté. Dermatol Surg. 2015;41(3):327–335.
- Merz Aesthetics. Ultherapy® – Merz Aesthetics. Available at: https://www.merzaesthetics.com/products/ultherapy/ Accessed February 29, 2020.
- Laubach HJ, Makin IR, Barthe PG, et al. Intense focused ultrasound: evaluation of a new treatment modality for precise microcoagulation within the skin. Dermatol Surg. 2008;34(5):727–734.
- Minkis K, Alam M. Ultrasound skin tightening. Dermatol Clin. 2014;32(1):71–77.
- Chan NP, Shek SY, Yu CS, et al. Safety study of transcutaneous focused ultrasound for non-invasive skin tightening in Asians. Lasers Surg Med. 2011;43(5):366–375.
- Bogle MA, Dover JS. Tissue tightening technologies. Dermatol Clin. 2009;27(4): 491–499.
- Sadick N. Tissue tightening technologies: Fact or fiction. Aesthet Surg J. 2008;28(2):180–188.
- Gold M. Update on tissue tightening. J Clin Aesthet Dermatol. 2010;3(5):36–41.
- Yu CS, Yeung CK, Shek SY, et al. Combined infrared light and bipolar radiofrequency for skin tightening in Asians. Lasers Surg Med. 2007;39(6):471–475.
- Chua SH, Ang P, Khoo LS, Goh CL. Nonablative infrared skin tightening in Type IV to V Asian skin: A prospective clinical study. Dermatol Surg. 2007;33(2):146–151.
- Lloyd AA, Graves MS, Ross EV. Laser–tissue interactions. Nouri K. (ed.) Lasers in Dermatology and Medicine. 2nd ed. New York, NY: Springer; 2018: 29–30.
- White WM, Makin IR, Barthe PG, et al. Selective creation of thermal injury zones in the superficial musculoaponeurotic system using intense ultrasound therapy: a new target for non-invasive facial rejuvenation. Arch Facial Plast Surg. 2007;9(1):22–29.
- White WM, Makin IR, Slayton MH, et al. Selective transcutaneous delivery of energy to porcine soft tissues using intense ultrasound (IUS). Lasers Surg Med. 2008;40(2):67–75.
- Hantash BM, Ubeid AA, Chang H, et al. Bipolar fractional radiofrequency treatment induces neoelastogenesis and neocollagenesis. Lasers Surg Med. 2009;41(1):1–9.
- Suh DH, Shin MK, Lee SJ, et al. Intense focused ultrasound tightening in asian skin: clinical and pathologic results. Dermatol Surg. 2011;37(11):1595–1602.
- Zelickson BD, Kist D, Bernstein E, et al. Histological and ultrastructural evaluation of the effects of a radiofrequency-based nonablative dermal remodelling device: a pilot study. Arch Dermatol. 2004;140(2):204–209.
- Taghizadeh F , Ramirez P. Neck maintenance post-facelift using Ulthera ® DeepSEE ® technology. Presented at: Annual Fall Meeting of the American Academy of Facial Plastic and Reconstructive Surgery; Washington, DC, September 4–8, 2012.
- Alhaddad M, Wu DC, Bolton J, et al. A randomized, split-face, evaluator-blind clinical trial comparing monopolar radiofrequency versus microfocused ultrasound with visualization for lifting and tightening of the face and upper neck. Dermatol Surg. 2019;45(1):131–139.
- Cheng CKL. High-efficiency combination treatment of submental neck fullness. Plast Reconstr Surg Glob Open. 2019;7(7):e2306.
- Lu PH, Yang CH, Chang YC. Quantitative analysis of face and neck skin tightening by microfocused ultrasound with visualization in Asians. Dermatol Surg. 2017;43(11): 1332–1338.
- Baumann L, Zelickson B. Evaluation of micro-focused ultrasound for lifting and tightening neck laxity. J Drugs Dermatol. 2016;15(5): 607–614.
- Kenkel JM. Evaluation of the Ulthera System for achieving lift and tightening cheek tissue, improving jawline definition and submental skin laxity; Presented at: American Society for Laser Medicine and Surgery; Boston, MA: 2013. Results can be viewed at: https://clinicaltrials.gov/ct2/show/results/NCT01368835?view=results. Last accessed 25 May 2021.
- Pak CS, Lee YK, Jeong JH, et al. Safety and efficacy of ulthera in the rejuvenation of aging lower eyelids: a pivotal clinical trial. Aesthetic Plast Surg. 2014;38(5):861–868.
- Lee HS, Jang WS, Cha YJ, et al. Multiple pass ultrasound tightening of skin laxity of the lower face and neck. Dermatol Surg. 2012;38(1):20–27.
- Alster TS, Tanzi EL. Noninvasive lifting of arm, thigh, and knee skin with transcutaneous intense focused ultrasound. Dermatol Surg. 2012;38(5):754–759.
- Gold MH, Sensing W, Biron J. Use of micro-focused ultrasound with visualization to lift and tighten lax knee skin. J Cosmet Laser Ther. 2014;16(5):225–229.
- Goldberg DJ, Hornfeldt CS. Safety and efficacy of microfocused ultrasound to lift, tighten, and smooth the buttocks. Dermatol Surg. 2014;40(10):1113–1117.
- Rokhsar C, Schnebelen W, West A, et al. Safety and efficacy of microfocused ultrasound in tightening of lax elbow skin. Dermatol Surg. 2015;41(7):821–826.
- Fabi SG, Few JW, Moinuddin S. Practical guidance for optimizing patient comfort during microfocused ultrasound with visualization and improving patient satisfaction. Aesthet Surg J. 2020;40(2):208–216.
- Sevi J. ASDS Annual meeting: final program-at-a-glance and poster abstracts. Available at: https://www.asds.net/Portals/0/PDF/annual-meeting-brochure.pdf. Accessed March 3, 2020.White LE, Martin N, et al. Ultrasound tightening of facial and neck skin: a rater-blinded prospective cohort study. J Am Acad Dermatol. 2010;62(2):262–269.
- White LE, Martin N, et al. Ultrasound tightening of facial and neck skin: a rater-blinded prospective cohort study. J Am Acad Dermatol. 2010;62(2):262–269.
- Fabi SG, Goldman MP. Retrospective evaluation of micro-focused ultrasound for lifting and tightening the face and neck. Dermatol Surg. 2014;40(5):569–575.
- Fabi SG, Massaki A, Eimpunth S, et al. Evaluation of microfocused ultrasound with visualization for lifting, tightening, and wrinkle reduction of the décolletage. J Am Acad Dermatol. 2013;69(6):965–971.
- Sasaki GH, Abelev N, Papadopoulos L. A split face study to determine the significance of adding increased energy and treatment levels at the marionette folds. Aesthet Surg J. 2017;37(8):947–960.
- Werschler WP, Werschler PS. Long-term efficacy of micro-focused ultrasound with visualization for lifting and tightening lax facial and neck skin using a customized vectoring treatment method. J Clin Aesthet Dermatol. 2016;9(2):27–33.
- Brobst RW, Ferguson M, Perkins SW. Noninvasive treatment of the neck. Facial Plast Surg Clin North Am. 2014;22(2):191–202.
- Fabi SG, Joseph J, Sevi J, et al. Optimizing patient outcomes by customizing treatment with microfocused ultrasound with visualization: gold standard consensus guidelines from an expert panel. J Drugs Dermatol. 2019;18(5):426–432.
- Marr K, Carruthers JDA, Humphrey S. Transient nerve damage after microfocused ultrasound with visualization. Dermatol Surg. 2017;43(6):894–896.
- Friedmann DP, Bourgeois GP, Chan HHL, et al. Complications from microfocused transcutaneous ultrasound: Case series and review of the literature. Lasers Surg Med. 2018;50(1):13–19.
- Sykes JM. Management of the aging face in the Asian patient. Facial Plast Surg Clin North Am. 2007;15(3):353–360, vi–vii.
- Jung HJ, Min J, Seo HM, Kim WS. Comparison of effect between high intense focused ultrasound devices for facial tightening: Evaluator-blinded, split-face study. J Cosmet Laser Ther. 2016;18(5):252–256.
- Mlosek RK, Malinowska S. Ultrasound image of the skin, apparatus and imaging basics. J Ultrason. 2013;13(53):212–221.
- Merz Pharmaceuticals. Data on File, Quoted from: Competitive Landscape in Asia: Clinical Pearls Ulthera Expert Meeting. Merz Pharmaceuticals GmbH; 2012.
- Suh DH, Choi JH, Lee SJ, et al. Comparative histometric analysis of the effects of high-intensity focused ultrasound and radiofrequency on skin. J Cosmet Laser Ther. 2015;17(5):230–236.
- Suh DH, So BJ, Lee SJ, et al. Intense focused ultrasound for facial tightening: histologic changes in 11 Patients. J Cosmet Laser Ther. 2015;17(4):200–203.
- Suh DH, Kim DH, Lim HK, et al. Intense focused ultrasound (IFUS) with a modified parameter on facial tightening: A study on its safety and efficacy. J Cosmet Laser Ther. 2016;18(8):448–451.
- CLASSYS Inc. Ultraformer. Available at: http://www.ultraformer.com/. Accessed 20 January 20, 2018.
- Hayashi K, et al. The effect of thermal heating on the length and histological properties of the glenohumeral joint capsule. Am J Sports Med. 1997;25(1):107–112.
- White WM, Makin IRS, Slayton MH et al. Selective transcutaneous delivery of energy to porcine soft tissues using intense ultrasound (IUS). Lasers Surg Med. 2008;40(2):67–75.
- Lee H, Nam SM, Park ES, Kim YB. Evaluation of micro-focused ultrasound for lifting and tightening the face. Arch Aesthet Plast Surg. 2015;21(2):65–69.
- Choi SY, No YA, Kim SY, et al. Tightening effects of high-intensity focused ultrasound on body skin and subdermal tissue: a pilot study. J Eur Acad Dermatol Venereol. 2016;30(9): 1599–1602.
- Ko EJ, Hong JY, Kwon TR, et al. Efficacy and safety of non-invasive body tightening with high-intensity focused ultrasound (HIFU). Skin Res Technol. 2017;23(4):558–562.
- Alam M, White LE, Martin N, et al. Ultrasound tightening of facial and neck skin: a rater-blinded prospective cohort study. J Am Acad Dermatol. 2010;62(2):262–269.
- Kim J, So BJ, Ryu HJ. Clinical effectiveness of a high-intensity focused ultrasound in skin lifting. Medical Lasers. 2014;3(2):55–58.
- Merz Aesthetics. https://ultherapy.com/. Accessed May 24, 2021.
- Close M. Special feature: treating the stomach. Available at: https://aestheticsjournal.com/feature/special-feature-treating-the-stomach. Accessed March 3, 2020.
- Biesman BS, Patel N. Physician alert: beware of counterfeit medical devices. Lasers Surg Med. 2014;46(7):528–530.
- Kyung JS, Yang SW, Soo KM, Chul KE. Corneal stromal damage through the eyelid after tightening using intense focused ultrasound. Can J Ophthalmol. 2015;50(4):e54–e57.
- Frank K, Hamade H, Casabona G, et al. Influences of age, gender, and body mass index on the thickness of the abdominal fatty layers and its relevance for abdominal liposuction and abdominoplasty. Aesthet Surg J. 2019;39(10):1085–1093.
- Montes JR, Santos E. Patient satisfaction following treatment with microfocused ultrasound with visualization: results of a retrospective cross-sectional survey. J Drugs Dermatol. 2019;18(1):75–79.
- Casabona G, Kaye K. Facial skin tightening with microfocused ultrasound and dermal fillers: considerations for patient selection and outcomes. J Drugs Dermatol. 2019;18(11):1075–1082.
- Carruthers J, Burgess C, Day D, et al. Consensus recommendations for combined aesthetic interventions in the face using botulinum toxin, fillers, and energy-based devices. Dermatol Surg. 2016;42(5):586–597.
- Fabi SG, Burgess C, Carruthers A, et al. Consensus recommendations for combined aesthetic interventions using botulinum toxin, fillers, and microfocused ultrasound in the neck, décolletage, hands, and other areas of the body. Dermatol Surg. 2016;42(10):1199–1208.
- Park JY, Byun EJ, Kim HS. Rejuvenation of periocular region in Koreans: A multimodal approach combining botulinum toxin, fillers, and micro-focused ultrasound with visualization for optimal results. Dermatol Ther. 2020;33(1):e13159.
- Fabi SG, Goldman MP, Mills DC, et al. Combining microfocused ultrasound with botulinum toxin and temporary and semi-permanent dermal fillers: safety and current use. Dermatol Surg. 2016;42 Suppl 2: S168–S176.
- Casabona G, Nogueira Teixeira D. Microfocused ultrasound in combination with diluted calcium hydroxylapatite for improving skin laxity and the appearance of lines in the neck and decolletage. J Cosmet Dermatol. 2018;17(1):66–72.
- Hart DR, Fabi SG, White WM, et al. Current concepts in the use of PLLA: clinical synergy noted with combined use of microfocused ultrasound and poly-L-lactic acid on the face, neck, and decolletage. Plast Reconstr Surg. 2015;136(5 Suppl):180S–187S.
- Casabona G, Pereira G. Combination treatment using microfocused ultrasound with visualization and calcium hydroxylapatite to improve skin laxity and the appearance of cellulite on buttocks and thighs. Plast Reconstr Surg Glob Open. 2017;5(7):e1388.
- Casabona G. Combined use of microfocused ultrasound and a calcium hydroxylapatite dermal filler for treating atrophic acne scars: a pilot study. J Cosmet Laser Ther. 2018;20(5):301–306.
- Casabona G, Michalany N. Microfocused ultrasound with visualization and fillers for increased neocollagenesis: clinical and histological evaluation. Dermatol Surg. 2014;40(Suppl 12):S194–S1948.
- Vachiramon V, Jurairattanaporn N, Harnchoowong S, Chayavichitsilp P. Non-invasive high-intensity focused ultrasound for UV-induced hyperpigmentation in Fitzpatrick skin types III and IV: a prospective, randomized, controlled, evaluator-blinded trial. Lasers Med Sci. 2018;33(2):361–367.
- Palm MD, Misell LM. Topical transdermally delivered lidocaine and benzocaine compared to compounded lidocaine/tetracaine during microfocused ultrasound with visualization treatment. J Drugs Dermatol. 2018;17(7): 729–734.
- Lin F. Non-surgical treatment of post-partum lower abdominal skin and soft tissue laxity using microfocused ultrasound with visualization. Dermatol Surg. 2020;46(12):1683–1690.

