 J Clin Aesthet Dermatol. 2022;15(4):44–48.
J Clin Aesthet Dermatol. 2022;15(4):44–48.
by Sahana P. Raju, MD, DNB, FRGUHS; Mukta Sachdev, MD, DPD, DD, FCS; Niti Khunger, MD, DDV, DNB; and Nina Madnani, MD
Dr. Raju is with the Department of Dermatology, Bangalore Medical College and Research Institute, India. Dr. Sachdev is with the Department of Dermatology at Manipal Hospital in Bangalore, India. Dr. Khunger is with the Department of Dermatology at VMMC & Safdarjung Hospital in New Delhi, India. Dr. Madnani is with the Department of Dermatology at PD Hinduja National Hospital and Sir HN Reliance Foundation Hospital in Mumbai, India.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: The COVID-19 pandemic has given rise to the need to use personal protective equipment such as masks, among healthcare professionals and the general public. Numerous facial dermatoses linked to the use of masks have been described, from which the term maskne or mask acne has emerged. Although prolonged mask usage has been necessary, and a vast majority of people develop various skin conditions, there is a lack of research on the effects of masks on skin. In this article, we review alterations in biochemical properties of skin associated with mask use in individuals with skin of color and the factors predisposing them to developing acne. Because masks are crucial in preventing the spread of COVID-19, we also elucidate some fundamental strategies such as gentle skin care measures, decreasing the duration of mask wear, and following appropriate protocols for mask re-use, which may prevent mask acne and its long-term effects.
Keywords: Mask acne, COVID-19, darker skin, N95 respirators
COVID-19 (coronavirus disease-2019), caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was declared a pandemic by the World Health Organization on March 11, 2020. The major route of transmission is via the respiratory system through inhalation of viral particles and droplets. Understandably, respiratory etiquette in the form of mask usage, coughing into a flexed elbow while in public, social distancing, and hand washing hygiene, form the mainstay in preventing the disease. However, prolonged periods of wearing masks is known to cause an array of physical and psychological adverse events, such as headaches, difficulty in breathing, cutaneous side effects, and impaired cognition.1 In a study by Techasatian et al2, acne was found to be the most common adverse event due to use of masks, followed by facial rash, itching, post-auricular rash, facial pigmentation and pressure related skin injury.
Guidance to preventing side effects associated with mask wearing is important, particularly among healthcare workers (HCW) who are required to wear masks continuously for prolonged periods. In this article, we review cutaneous biomechanical alterations, in particular acne, associated with mask usage among individuals with skin of color, and measures that may be taken to mitigate these negative effects.
Types of masks
Masks can be mainly divided into two categories— medical and nonmedical. Medical masks include N95 respirators and surgical masks, and nonmedical masks include fabric masks. In regard to N95 respirators, N denotes the National Institute for Occupational Safety and Health of the United States (NIOSH) and 95 represents filter efficacy, which amounts to mask being 95-percent efficient in filtering out particles measuring 0.3 microns or larger. SARS-CoV-2 molecules are around 0.1 micron in size, but are transmitted via larger respiratory droplets.3
To be effective, masks should be compactly worn against the skin without gaps. Continuous use of these masks over prolonged periods of time may lead to the formation of a microenvironment with increased temperature and humidity, thus triggering changes in the skin exposome favorable for the de-novo development or aggravation of acne; hence, the term maskne emerged.4,5 Mask acne is thought to be a subtype of acne mechanica, although numerous other factors are implicated in its pathogenesis.
Pathomechanism of mask acne
Understanding the effects of two major factors—temperature and humidity—plays a key role in comprehending the occurrence of acne with use of masks.
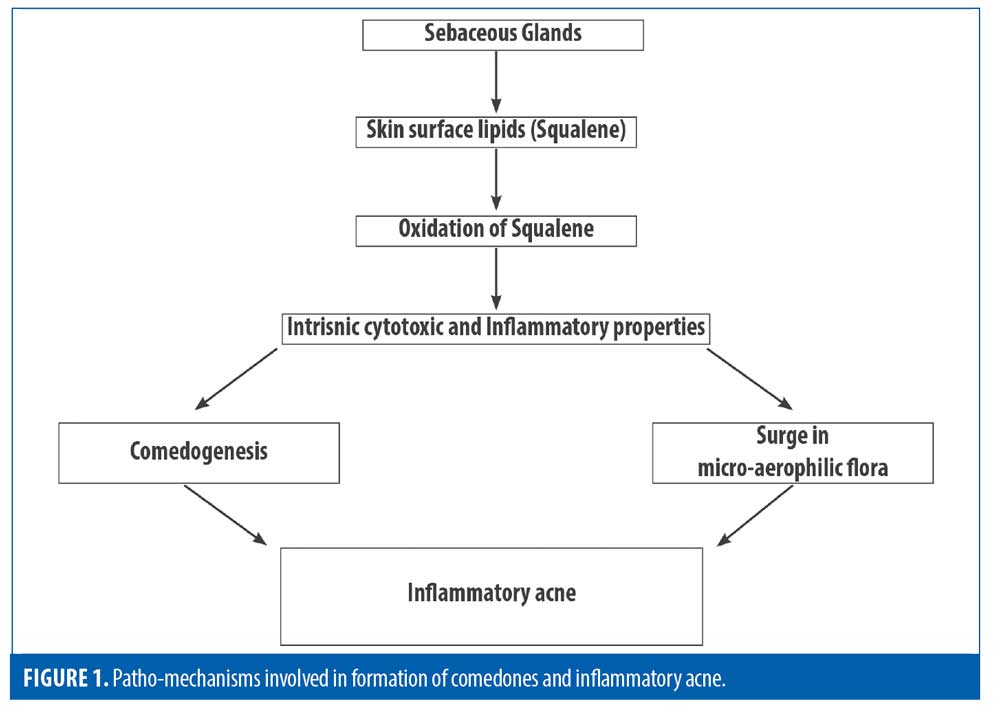
Effect of temperature on lipid composition. An increase in ambient temperature effectuates changes in composition of skin surface lipids (SSL). A qualitative analysis of SSL by thin layer chromatography (TLC) has shown the following components, in decreasing order of polarity: squalene, sterol-esters, wax-esters, triglycerides, free fatty acids, cholesterol, and lastly, mono- and diglycerides. The role of squalene and its oxidation products such as mono-hydroperoxide, in the pathogenesis of acne was highlighted in a study by D. Saint-Leger et al,6 and is illustrated in Figure 1. Also, quantitative differences have been found in the specific wax ester lipid fractions between fair skin and darker skin, which may result in morphological changes in presentation of acne.7
Effect of temperature on sebum excretion rate (SER). Changes in temperature were proportionally shown to increase or decrease SER by 10 percent per 1°C. This can be partly attributed to sebum viscosity decreasing with an increase in temperature. It may increase cutaneous circulation, which may increase gland metabolism rate of sebum excretion.8
Effect of humidity on the pilosebaceous duct. Williams et al9 deduced that increase in humidity produces hydration of keratin and reduces the pilosebaceous duct orifice. It has also been shown that humidity causes swelling of epidermal keratinocytes.10 Applying Poiseuille’s law (which states that flow rate of a fluid is directly proportional to fourth power of radius and inversely proportional to outflow resistance), the researchers concluded that a decrease in pilosebaceous duct size, ultimately resulting in obstruction of the duct.
Psychological stress and sleep disturbances are associated with the current pandemic, which significantly alter skin homeostasis and trigger the mechanisms responsible for acne.11 Insufficient sleep increases cortisol levels and sebum dysregulation, leading to an increase in proinflammatory cytokines and oxidative stress. Also, the use of masks results in a greater concentration of CO2 on the transepidermal surface, which can result in altered biomechanics triggering or aggravating acne.12
The final common pathway,involving an amalgamation of intrinsic and extrinsic factors could either trigger or aggravate acne vulgaris.
Factors predisposing to mask acne
Occupation. Various studies indicated a higher incidence of mask acne in healthcare workers compared to the general public, which can be explained by the increased hours of wearing personal protective equipment.2,13,14
Techasatian et al2 demonstrated that the risk of acne increased by 1.5 times in people who changed their masks every 2 to 3 days, compared to the people who changed masks on a daily basis.
In a study by Foo et al3, all patients who developed acne reported using N95 respirators for an average duration of eight hours per day for a mean period of 8.4 months. Lan et al13 described higher incidence of acne in HCP’s who wore masks for longer than six hours.13 Techasatian et al2 showed that wearing masks up to four hours per day increased the risk for acne.
Type of mask used. Foo et al3 reported cases of acne to be associated with N95 respirators but not surgical or fabric masks during the SARS epidemic in 2003. This may be attributed to the greater air impermeability and increased local pressure of N95 masks.14 Also, masks with a nasal metal wire or fixation bar have been associated with increased predisposition to acne and nickel contact sensitivity in wearers.15 Surgical masks covered by a cloth mask have also been associated with increased predisposition to acne.2 In general, medical masks have been linked to higher predisposition for acne, compared to cloth masks, although the type of fabric must be taken into consideration.
Underlying/aggravating conditions. In a study by Zuo et al,14 underlying inflammatory facial dermatoses were found to be a significant risk factor for acne, which could be due to skin barrier pathology and alteration of skin microbiome. In another study, psychological stress and pre
menstrual flare were found to be significantly associated with mask acne.16
Previous history of acne. In a study by Daye et al,15 more than 50 percent of health care workers using personal protective equipment in the form of masks, especially those with a metal nose bridge, reported an increase in pre-existing acne.
In a study by Ramesh A et al16, the incidence of mask induced acne among health care workers (doctors) was found to be 62.3 percent, among which 50 percent had new onset acne , whereas the other 50 percent had an aggravation of pre-existing acne.
Other than masks, goggles and face shields were also implicated in causing acne.15
Sites affected
The most commonly involved areas of mask acne include the nasal bridge, both cheeks, and chin, described as the zero zone of face. Other personal protective equipment such as face shields can predispose an individual to acne on forehead. In a study by Damiani et al,17 scores on the Global Acne Grading System (GAGS) and Dermatology Life Quality Index (DLQI) significantly worsened in patients (general population) with pre-existing acne and rosacea particularly in areas over the nose, cheeks, and chin, with no changes over forehead, chest, or upper back, after six weeks of use of mask.
Clinical picture and criteria for mask acne
Sinha et al18 considered maskne as a blanket term to encompass acne and other facial lesions caused by masks, such as itching, dryness, contact dermatitis, and maceration.18 Both noninflammatory and inflammatory lesions have been known to occur with use of masks
(Figure 2).

Another consequence of COVID-19 is mask rosacea. A flare in rosacea has been reported in healthcare workers wearing masks for more than eight hours.19 Papulopustular and erythematotelangiectatic were the most common subtypes.17 Mask acne and mask rosacea were described as true Koebner phenomena related to mask use due to various factors acting on the previously inflamed pilosebaceous system.20
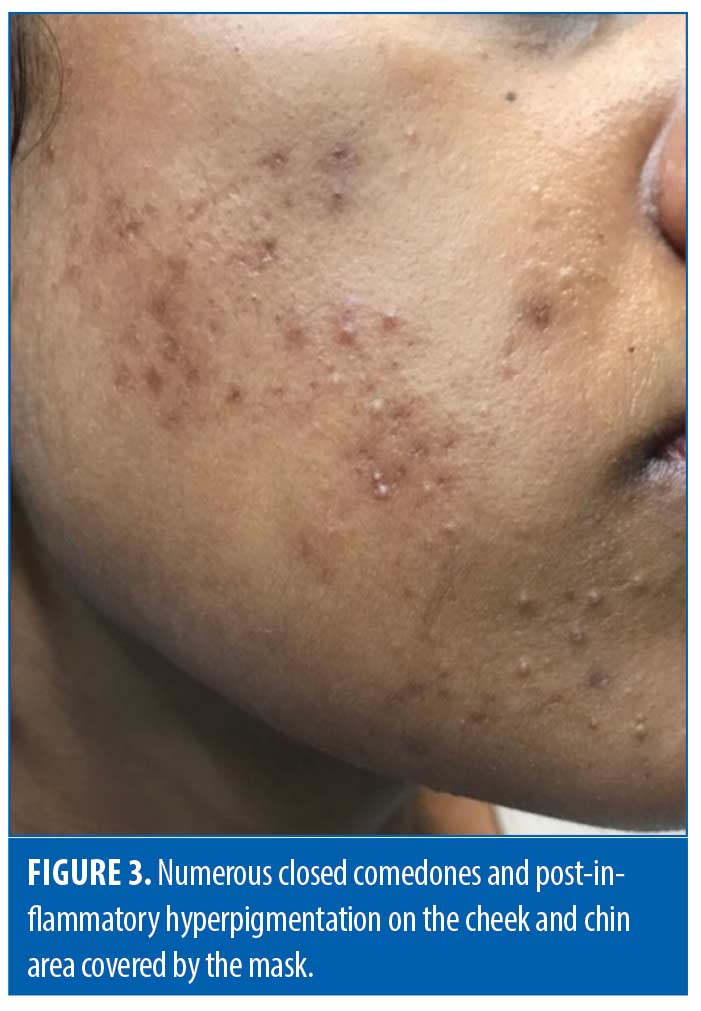
Acne in skin of color has morphological differences compared to light skin.21 Although dark-skinned individuals have a lower propensity to develop nodulocystic acne, they are more likely to develop inflammatory lesions, which may lead to complications such as postinflammatory hyperpigmentation (PIH), keloid formation, and scarring (Figure 3).22 Perkins et al23 reported that postinflammatory hyperpigmentation was the most common complication of acne in skin of color patients.
Teo24 proposed the following criteria for mask acne:
- Occurrence of new lesion of acne or flare of pre-existing acne within six weeks of using masks
- Occurrence of lesions over a clearly demarcated areas—the zero zone
- Exclusion of other common causes of facial eruption, such as rosacea, seborrheic dermatitis, perioral dermatitis, and pityrosporum folliculitis.
Measures which can be implemented to prevent mask acne
People in an open air public setting, where there is least risk of infection, should be educated to wear only nonmedical masks or surgical masks, which not only decrease the incidence of cutaneous facial side effects, but also help solve the problem of scarcity of medical masks, especially N95 respirators, for healthcare workers. N95 respirators, though more expensive and uncomfortable, are of use only in highly contaminated environments.25 Also, synthetic fiber masks are preferred over natural fiber masks, as natural fibers absorb moisture, increasing humidity and thus magnifying the discomfort.24
Education regarding proper use of personal protective equipment and restricting the hours of wearing masks could prevent most of the cutaneous adverse effects. Reduce the duration of pressure by taking mask-free breaks 15 minutes every two hours outside of contaminated areas. If this is not feasible, the mask can be lifted from the sides every two hours.26
The use of hydrocolloid/thin foam dressings or silicone gels underneath pressure points on the face, such as the bridge of the nose, zygomatic arch, and post-auricular regions has been advocated to minimize mechanical friction and pressure injuries caused by masks.27
Frequent touching of the face should be discouraged because it not only causes irritation to the skin, but also increases the risk of contracting COVID-19. Handwashing before and after touching one’s face mask, as well as avoiding the use of make-up on the face, may also reduce risk of developing or exacerbating acne. Avoidance of make-up and washing hands before and after touching a mask can prevent mask acne.
The current United States Centers for Disease Control and Prevention (CDC) guidelines for reusing masks in the settings of noncontaminated or minimally contaminated places are that N95 respirators can be used for a maximum of five times after 72 hours of proper drying.28 They must be discarded appropriately after that. Surgical masks are recommended for single use only. Fabric masks can be reused after washing and drying.
Use of a mild, fragrance-free, noncomedogenic cleanser before and after mask use should be encouraged. Cleansers with alpha and beta- hydroxy acids should be avoided due to risk of irritant contact dermatitis under occlusion. Adequate moisturization using noncomedogenic moisturizers at least one hour before use of mask is beneficial. However, petrolatum-based emollients are not recommended as they impede the function of masks, especially N95 respirators.29
Since sunscreen application every 3 to 4 hours is not practical during the pandemic due to long hours of wearing masks, Teo24 advocated the use of ultraviolet protective (UPF) 50+ fabric masks as a photoprotective measure.24
Treatment
Conventional acne treatment, including retinoids, benzoyl peroxide, and salicylic acid, should be prescribed with caution, as they can lead to irritant contact dermatitis when followed by long hours of occlusion from masks. They should be applied during mask- free intervals. Cosmeceuticals containing plant extracts, essential oils, and phytomolecules with antiproliferative, anti-inflammatory and antimicrobial activity may be used for mask acne.30
Mild-to-moderate lesions of acne can be treated with colloidal nanosystems for targeted delivery of topical retinoids and antibiotics, which are more efficacious and cause less irritation.31 Isotretinoin should be used with caution as its side-effect profile is exaggerated due to the moist microenvironment provided by the mask. The risk of secondary infections, such as gram negative folliculitis, Malassezia folliculitis, and impetigo, is increased in individuals with mask acne being treated with isotretinoin.32
PIH should be given top priority in darker skined individuals, as it can cause more psychological distress than the actual acne itself. Early and aggressive treatment of acne is the key to prevent PIH. However, the reality of wearing masks for long hours and the inclination of darker skin to develop irritation must be borne in mind. Topical skin lightening agents to treat PIH should be chosen judiciously as hydroquinone and tretinoin can cause irritant dermatitis. Kojic acid, arbutin, and licorice extract are safer.
Conclusion
Acne is a complex, multifaceted entity with a wide variety of factors responsible for it. Adding to the causative factors are use of personal protective equipment, such as masks, which has primarily been documented in healthcare workers and in certain Association of Southeast Asian Nations (ASEAN) countries where mask wearing has been a common practice as part of antipollution measures. Cutaneous adverse effects caused by masks not only precipitate a skin barrier breach, but can also serve as a means of increased transmission of COVID-19. Healthcare workers are principally affected, which could add to their psychological burden and affect self-esteem. Maskne is becoming increasingly more common in regular clinical and aesthetic dermatology practice and should be considered as an etiological factor in the presentation of acne vulgaris. The efficient management of mask-induced acne is of utmost importance to alleviate long-term physical and psychosocial impacts.
References
- Rosner E, Adverse effects of prolonged mask use among healthcare professionals during COVID-19. J Infect Dis Epidemiol 2020 6:130.
- Techasatian L, Lebsing S, Uppala R et al, The effects of the face mask on the skin underneath: A prospective survey during the COVID-19 pandemic. J Prim Care Community Health. 2020 ;11:2150132720966167
- Foo CC, Goon AT, Leow YH, Goh CL. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome-a descriptive study in Singapore. Contact Dermatitis. 2006 ;55:291–294
- Krutmann J, Bouloc A, Sore G, et al. The skin aging exposome. J Dermatol Sci. 2017;85:152-161
- Tan KT, Greaves MW. N95 acne. Int J Dermatol. 2004 ;43:522–523
- Saint-Leger D, Bague A, Lefebvre E et al. A possible role for squalene in the pathogenesis of acne. II. In-vivo study of squalene oxides in skin surface and intra-comedonal lipids of acne patients. Br J Dermatol. 1986 ;114:543–552
- Pappas A, Fantasia J, Chen T. Age and ethnic variations in sebaceous lipids. Dermatoendocrinology. 2013;5:319–324
- Cunliffe WJ, Burton JL, Shuster S. The effect of local temperature variations on the sebum excretion rate. Br J Dermatol. 1970;83:650–654
- Williams M, Cunliffe WJ, Gould D. Pilo-sebaceous duct physiology. I. Effect of hydration on pilo-sebaceous duct orifice. Br J Dermatol. 1974;90:631–635
- Sardana K, Sharma RC, Sarkar R. Seasonal variation in acne vulgaris-myth or reality. J Dermatol. 2002;29:484-488
- Xerfan EMS, Facina AS, Andersen ML et al. Acne flare-up due to mask wearing: A current pandemic scenario and its relationship with sleep. Skin Res Technol. 2021:17
- Scarano A, Inchingolo F, Lorusso F. Facial skin temperature and discomfort when wearing protective face masks: thermal infrared imaging evaluation and hands moving the mask. Int J Environ Res Public Health. 2020;17:462–464
- Lan J, Song Z, Miao X et al. Skin damage among healthcare workers managing coronavirus disease-2019, J Am Acad Dermatol. 2020;82:1215–1216.
- Zuo Y, Hua W, Luo Y, Li L. Skin reactions of N95 masks and medial masks among health-care personnel: A self-report questionnaire survey in China. Contact Dermatitis. 2020;83:145–147
- Daye M, Cihan FG, Durduran Y. Evaluation of skin problems and dermatology life quality index in health care workers who use personal protection measures during COVID-19 pandemic. Dermatol Ther. 2020 ;33:e14346
- Ramesh A, Shabari A. Clinico-epidemiological study of mask induced acne due to increased mask use among healthcare workers during COVID pandemic in a tertiary care institute. Int J Res Dermatol 2021;7:48–52
- Damiani G, Gironi LC, Grada A et al. COVID-19 related masks increase severity of both acne (maskne) and rosacea (mask rosacea): Multi-center, real-life, telemedical, and observational prospective study. Dermatol Ther. 2021;34:e14848
- Sinha A, Singh AR. An unforeseen hazard of masks being in vogue. Int J Occup Environ Med 2020;11:213-214
- Chiriac AE, Wollina U, Azoicai D. Flare-up of Rosacea due to face mask in healthcare workers during COVID-19. Maedica (Bucur). 2020;15:416-417
- Damiani G, Gironi LC, Kridin K et al. Mask-induced Koebner phenomenon and its clinical phenotypes: A multicenter, real-life study focusing on 873 dermatological consultations during COVID-19 pandemics. Dermatol Ther. 2021;34:e14823.
- Davis EC, Callender VD. A review of acne in ethnic skin: pathogenesis, clinical manifestations, and management strategies. J Clin Aesthet Dermatol. 2010;3:24–38
- Wilkins JW, Jr, Voorhees JJ. Prevalence of nodulocystic acne in white and negro males. Arch Dermatol. 1970;102:631–634.
- Perkins A, Cheng C, Hillebrand G, et al. Comparison of the epidemiology of acne vulgaris among Caucasian, Asian, Continental Indians, and African American women. J Eur Acad Dermatol Venereol. 2011;25:1054–60.
- Teo WL. Diagnostic and management considerations for ‘Maskne’ in the era of COVID-19. J Am Acad Dermatol. 2020;84:
520–521 - Jefferson T, Del Mar C, Dooley L et al. Physical interventions to interrupt or reduce the spread of respiratory viruses: systematic review. BMJ. 2009 21;339:b3675
- National Pressure Injury Advisory Panel (NPIAP). NPIAP position statements on preventing injury with N95 masks. 2020. https://cdn.ymaws.com/npiap.com/resource/resmgr/position_statements/Mask_Position_Paper_FINAL_fo.pdf
- Balato A, Ayala F, Bruze M et al. European Task Force on Contact Dermatitis statement on coronavirus disease-19 (COVID-19) outbreak and the risk of adverse cutaneous reactions. J Eur Acad Dermatol Venereol. 2020;34:353–354
- Implementing Filtering Facepiece Respirator (FFR) reuse, including reuse after decontamination, when there are known shortages of N95 respirators. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/decontamination-reuse-respirators.html
- Desai SR, Kovarik C, Brod B et al. COVID-19 and personal protective equipment: treatment and prevention of skin conditions related to the occupational use of personal protective equipment. J Am Acad Dermatol. 2020;83
:675–677 - Sinha P, Srivastava S, Mishra N, Yadav NP, new perspectives on antiacne plant Drugs: contribution to modern therapeutics’ , Biomed Research International, 2014;301–304
- Latter G, Grice JE, Mohammed Y, et al. Targeted Topical Delivery of Retinoids in the Management of Acne Vulgaris: Current Formulations and Novel Delivery Systems. Pharmaceutics 2019;11:490.
- Teo WL. The “Maskne” microbiome – pathophysiology and therapeutics. Int J Dermatol. 2021, 12:10–11.

