 J Clin Aesthet Dermatol. 2022;15(4):49–58.
J Clin Aesthet Dermatol. 2022;15(4):49–58.
by Jaspriya Sandhu, MD, DNB, MNAMS; Arushi Kumar, MD; Sunil Kumar Gupta, MD; and Shriya Garg, MBBS
All authors are with the Department of Dermatology, Venereology and Leprology, Dayanand Medical College and Hospital in Ludhiana, Punjab, India.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Objective. Mask usage and hand hygiene are the pillars of defense against the novel pathogen causing COVID-19. This study was conducted to compare these practices among healthcare workers (HCWs) and nonhealthcare workers (nonHCWs) and to examine the outlook toward the healthcare sector among the two.
Methods. A cross-sectional online survey (via Google forms) using snowball sampling was conducted. Appropriate ethical clearance was taken from the Institutional Ethical Committee (IEC). HCWs and nonHCWs 18 years of age or older with basic literacy in English and with internet access were included.
Results. There were 404 total respondents (M:F ratio: 0.87:1; mean age: 30.16±9.63 years). Among the respondents, 63.3 percent were HCWs while 35.6 percent were nonHCWs. Persons performing hand hygiene more than10 times/day were found to be almost three times more likely to develop skin dryness (odds ratio [OR]: 2.95, 95% confidence interval [CI]: 1.372, 6.362). Female participants were found to be 2.5 times more likely to develop dryness (odds ratio: 2.594, 95% CI: 1.590, 4.234). Use of gloves was found to be a protective factor against development of dryness (odds ratio: 0.485,95% CI: 0.287, 0.818). A statistically significant correlation was found between mask acne and female respondents (p-value=0.000), HCWs (p-value=0.000), and use of N95 mask in combination with surgical mask (p-value=0.04).
Limitations. Being an online survey, responses could not be captured from people with limited internet access and of lower socio-economic strata.
Conclusion. There is a considerable burden of preventive measures on HCWs and nonHCWs alike. Significant dermatological implications are seen with frequent hand hygiene and mask usage.
Keywords: COVID-19 pandemic, hand hygiene, hand eczema, masks, perception, practice patterns, questionnaires and surveys
The coronavirus disease of 2019 (COVID-19) pandemic is an unparalleled challenge the entire world is facing, perhaps forever altering an increasingly globalized world. Since the first confirmed report of human-to-human transmission of COVID-19 in January 2020, the impact of the virus has been felt by each and every individual. Early concerns of the outbreak began in late 2019, when a cluster of pneumonia cases of an unknown etiology (possibly originating from wet markets) began surfacing in the city of Wuhan in Hubei Province of China.1,2 Quick comparisons were made to the severe acute respiratory syndrome (SARS) outbreak of 2003, but the contagion soon surpassed SARS-1 cases.3 Subsequently, on March 11, 2020, COVID-19 was declared a pandemic by the World Health Organization (WHO).4 The WHO officially named the virus severe acute respiratory syndrome coronavirus 2 (SARS-COV2), and COVID-19 was the disease caused by this virus.5 As of March 2022, India has reported 42,951,566 confirmed cases of COVID-19 with 514,589 deaths.6
Current evidence shows that the virus is a droplet infection that spreads from human to human.7,8 To prevent this transmission, health agencies and state governments have recommended social distancing, wearing masks, and frequent hand hygiene.9,10 The impact on the healthcare sector has been enormous, particularly for a country like India where the doctor:patient ratio is only 0.62 per 1,000 persons (with rural areas largely underserved), as opposed to the 1 per 1,000 persons recommended by the World Health Organization (WHO).11,12 Though no data have been made public by the government, the Indian Medical Association (IMA) reports that more than 1,500 doctors have died of COVID-19 as of July 2021.13 Even in these devastating times, violence against doctors has continued unabated, further adding to their duress.14 Furthermore, COVID-19 has impacted livelihoods and businesses, leading to increased incidences of anxiety, depression, and even suicide.15
There is paucity of data regarding hand hygiene and mask usage practices among the healthcare community and general population, particularly in India; therefore, we conducted a survey to analyze these new practices and behaviors in the COVID-19 pandemic.
Hypothesis
Hand hygiene practices and mask usage recommended during the pandemic have a significant physical and psychological burden. Hand hygiene practice and mask usage differs among healthcare workers (HCWs) and nonhealthcare workers (nonHCWs).
Objective
Primary objectives. The primary obejctives are to study hand hygiene practices and their cutaneous implications; to study mask usage practices, types of masks used, and problems related to mask usage; and to examine the outlook of individuals toward the healthcare sector.
Secondary objectives. The secondary objectives are to compare the hand hygiene practices among HCWs versus nonHCWs; to compare mask usage practices, types of masks used, and problems faced by HCWs versus nonHCWs; and to compare differences of outlook toward the healthcare sector among HCWs versus nonHCWs.
Methods
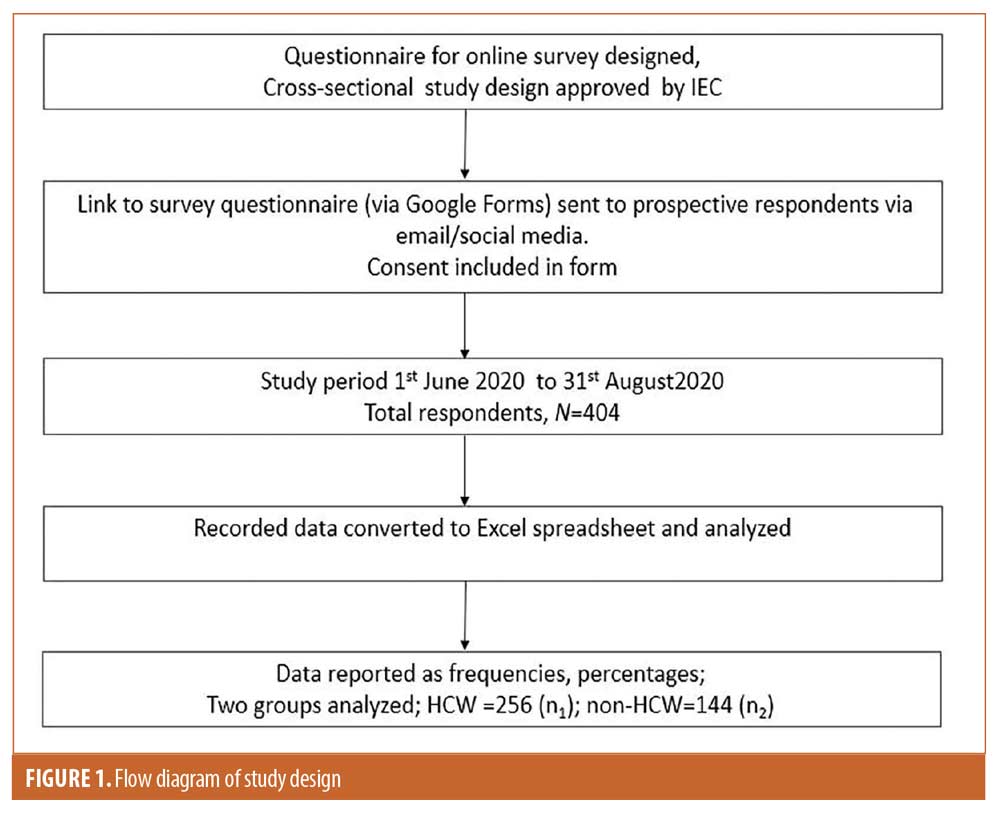
Study design and location. A cross-sectional online questionnaire-based survey was conducted by investigators based in a medical college and tertiary hospital in Punjab, India. The data were collected between June 1, 2020, and August 31, 2020. This study was reviewed and approved by the Institutional Ethical Committee (IEC). A brief layout of the study design is represented in Figure 1.
Study population. Snowball sampling was used to recruit participants via email and social media (e.g., WhatsApp, LinkedIn), and they were encouraged to reach out to their respective contacts. The study participants were included if they were 18 years or older and either an HCW or lay person living in India or abroad with basic literacy in English and internet access. The study participants consented to participate in the study via consent in the google form.
Sample size determination. With the assumption that more than 50 percent of the population is aware of the COVID-19 pandemic and adhering to the prescribed preventive measures, the calculated sample size as the per the Leslie Kish formula {n=Zalpha2 p(1-p)/d2} was 384.
Study tool. The questionnaire was designed by principal investigator (PI). An online survey of 24 questions with multiple options (single option/check boxes/Likert scale) was conducted via a Google form which included a linked consent and usage form
Data analysis. The data were sourced from the Google form onto an Excel spreadsheet. Data were analyzed by Statistical Package for the Social Sciences (SPSS) version 20. Data was described in terms of numbers, frequencies, and percentages. Fischer’s exact test and Chi-square test were used to determine associations. Multiple logistic regression analysis was applied with the demographic characteristics, hand hygiene practices, and mask usage as independent variables, with development of problems occurring therein as the dependent variable. Spearman correlation was applied to determine burden felt by respondents with demographic data, hand hygiene, and mask usage. P-value less than 0.05 was considered to be significant.
Bias. To ascertain the bias in this study, we used the risk of bias instrument for cross-sectional survey of attitudes and practice.15
Results
Demographic data. A total of 404 respondents completed the survey. The male-to-female ratio was 0.87:1 (2 study participants preferred not to specify sex). The mean age of respondents was 30.16±9.63 years. The majority of participants were younger than 35 years of age (81.18%); most had college-level education or higher (86.6%). Among the respondents, 63.3 percent were HCWs and 35.6 percent were nonHCWs (4 [0.9%] respondents chose not to answer this question) (Table 1).
Hand hygiene practice. The most common sources of information regarding hand hygiene and preventive measures in the survey were government guidelines/Arogya setu application/COVA Punjab application (63.3%). These were the most frequent sources for both HCWs (61.32%) and nonHCWs (59.72%). A significantly higher number of HCWs gathered information from medical journals/textbooks (57.81%) and newspapers (53.12%), whereas, for nonHCWs, friends/family/colleagues (54.16%) and television (55.56%) were significant sources of information (Table 2).
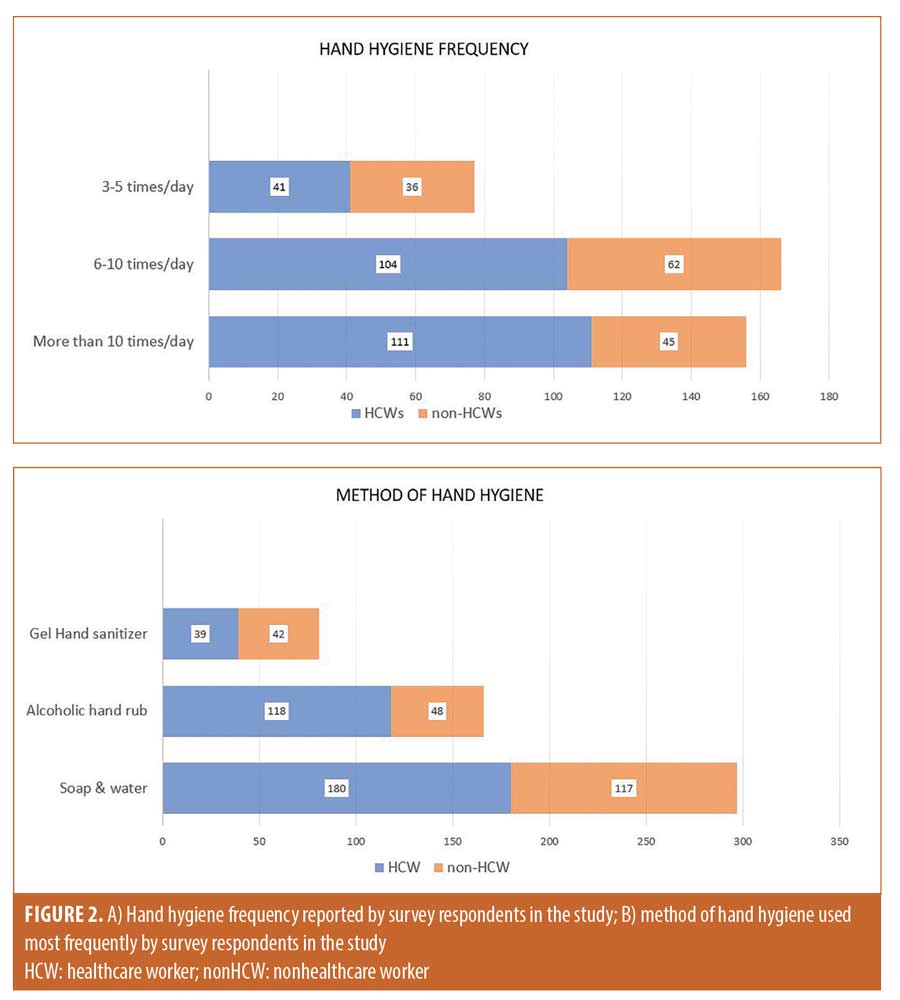
Forty-three percent of HCWs (43.35%) washed their hands more than 10 times per day, compared to 31.32 percent of nonHCWs. Sixteen percent (16.01%) of HCWs and 25 percent of nonHCWs washed their hands 3 to 5 times a day. Only one (0.69%) individual (nonHCW) reported washing their hands 1 to 2 times per day. The most frequently used method for practicing hand hygiene among HCWs was soap and water (70.3%), followed by alcoholic hand rub (46.1%); similar practice was seen among nonHCWs. Use of gel-based hand sanitizers was significantly higher in nonHCWs (29.16%, P<0.001) (Figures 2a and 2b).
A higher percentage of HCWs (40.23%) “strongly agreed” that there has been a marked change in their hand hygiene routine ever since the pandemic, compared to nonHCWs (31.25%); only 5.46 percent of HCWs and 8.33 percent of nonHCWs “strongly disagreed.”
Slightly more HCWs (55.07%) reported regular moisturizer use compared to nonHCWs (52.08%). Significantly more HCWs used latex gloves (64.06%), compared to nonHCWs (18.75%) (P<0.0001). Surfaces at home were disinfected by significantly more HCWs compared to nonHCWs (76.75% vs. 23.61%, respectively, P<0.0001) (Table 2).
Impact of hand hygiene practice. Out of 404 participants, 130 (32.17%) had some form of dermatological problem they attributed to their hand hygiene practices. Overall, excessive dryness was the most common condition reported by respondents (27.72%).
The frequency of dermatological problems was higher among HCWs, with 36.3 percent reporting one or more dermatological complaints, compared to 25.69 percent nonHCWs. Among HCWs, these complaints included excessive dryness (31.25%), itching (5.1%), eczema (4.68%), and intertrigo (3.1%). Among nonHCWs, dryness (22.22%) was most common, followed by itching (4.8%) and intertrigo (4.8%). Eczema was reported less frequently by nonHCWs (0.69%).
Eczema. Of the 13 respondents who developed hand eczema/dermatitis, 12 were HCWs (92.3%) and one was a nonHCW (7.7%); the male-to-female ratio was 0.85. The mean age of respondents who developed eczema was 28±3.85 years. A pre-existing atopy was present in six respondents (46.1%); an associated known latex allergy was seen in two of these respondents (15.3%). Atopic conditions seen among these respondents were asthma (23.1%), allergic rhinitis (15.4%), and pre-existing hand eczema (46.2%).
All of the respondents reported hand hygiene frequency of six or more times a day, with five (38.5%) of them reporting a frequency greater than 10 times aday. All the respondents reported hand hygiene with soap and water, alcoholic hand rub, or both; none of them used gel-based hand sanitizers. Dermatology consult was sought by less than half the respondents; a higher percentage of HCWs (8.59%) sought dermatological consult for skin problems they attributed to hand hygiene practices, compared to 1.3 percent of nonHCWs. Latex gloves were used by 79.2 percent of respondents who developed hand eczema; 53.8 percent reported regular use of a moisturizer. Development of eczema did not show significant association with the frequency of hand hygiene in both HCWs (P=0.224) and nonHCWs (P=0.514) (Table 3).
Intertrigo. More HCWs compared to nonHCWs reported intertrigo (Total: 15; HCWs: 8; nonHCWs: 7); the male-to-female ratio was 1.14. The mean age of respondents who developed intertrigo was 28.8±4.19 years. Atopy was reported by five respondents (33.3%). All of the respondents reported hand hygiene frequnecy of six or more 6 times a day, with five (33.3%) of them reporting a frequency greater than 10 times a day. Alcoholic hand rub alone was used by five respondents (33.3%), and one respondent reported use of gel-based hand sanitizer. Latex gloves were used by 53.3 percent of respondents who developed hand eczema; 60 percent reported regular use of a moisturizer. None of them sought specialist care for their complaints. Development of intertrigo did not show significant association with the frequency of hand hygiene in both HCWs (P=0.366) and nonHCWs (P=0.194) (Table 4).
Dryness. Incidence of dryness increased significantly with the frequency of hand hygiene, especially in those whose hand hygiene frequency was greater than10 times a day (P<0.001). Female respondents were 2.5 times more likely to develop dryness compared to male respondents (odds ratio [OR]: 2.594, 95% confidence interval [CI]: 1.590, 4.234). Persons performing hand hygiene were almost three times more likely to develop dryness (OR: 2.95, 95% CI: 1.372, 6.362).
Use of hand gloves was found to be a protective factor against the development of dryness caused by hand hygiene (OR: 0.485,95% CI: 0.287, 0.818).
There was a statistically significant correlation of dryness in participants with pre-existing hand eczema (P=0.024), allergic rhinitis (P<0.001), and asthma (P=0.013).
Development of dryness correlated with the development of eczema (P=0.03) and intertrigo (P<0.001) associated with hand hygiene.
No significant correlation was found between age (P=0.707), method of hand hygiene (P=0.346), occupation (HCW vs. nonHCW) (P=0.064), or a known latex allergy (P=0.961) with the development of dryness.
Mask use. Overall, 87.4 percent of respondents “always” wore a mask, while 10.14 percent “mostly” wore one. The majority of HCWs used an N95 mask (46.48%) or surgical mask (34.37%), and some wore a surgical mask in combination with an N95 mask (28.51%). There was a statistically significant association of N95 and surgical mask usage in HCWs (P<0.0001)
Among nonHCWs, cloth masks (44.4%) and surgical masks (38.89%) were used more commonly than N95 masks (34.02%). A significantly smaller percentage of nonHCWs used an N95 mask in combination with a surgical mask (10.41%) (P<0.0001).
Impact of mask use. More HCWs (71.48%) reported problems with mask usage compared to nonHCWs (57.6%). “Inability to breathe satisfactorily” was reported by 46.28 percent of total respondents, slightly more among HCWs (HCWs: 47.26%, nonHCWs: 45.83%). A significantly higher percentage of HCWs reported itching/redness (21.87%, P=0.000538), pressure injury (16.01%, P=0.00016), and headache (18.35%) associated with mask use. Among nonHCWs, light headedness (9.02%), fatigue (8.33%), and itching/redness (8.33%) were common, while a few reported pressure injury (3.47%), headache (7.63%), and light headedness (9.02%, P=0.003474). There was a statistically significant association between acne and HCWs compared to nonHCWs (P<0.0001) (Figure 3) (Table 5).
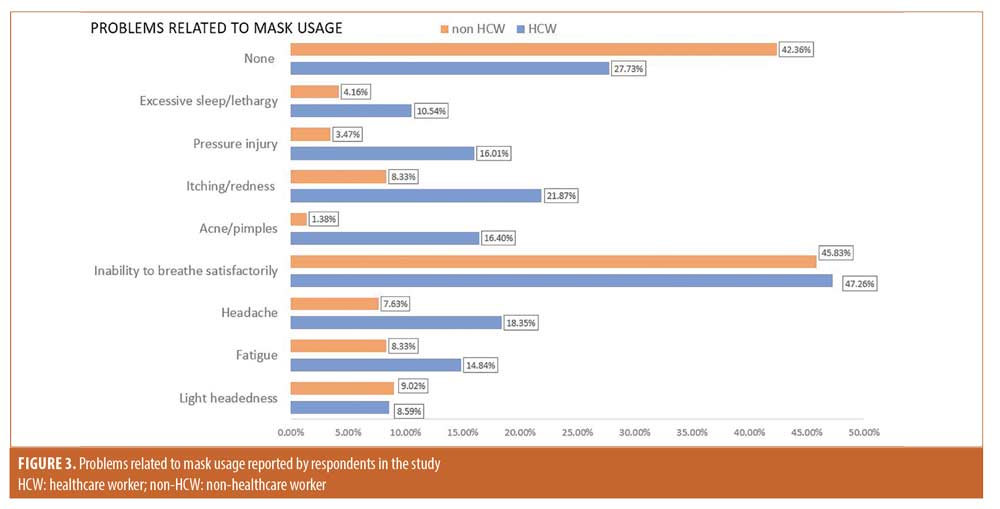
Mask acne. Acne/pimples were reported by 11 percent of respondents; 95.4 percent of them were HCWs (Total: 44/400 [11%]; HCWs: 42/44 (95.4%); nonHCWs: 2/44 [4.5%]); the male-to-female ratio was 0.22. The mean age of respondents who developed acne was 29.79±6.85 years. Thirty-four of the 44 respondents who developed acne wore an N95 mask, either alone or in combination with a surgical mask. None of these respondents used a dupatta/scarf or handkerchief. There was a statistically significant association between development of acne and female sex (P=0.000), HCWs (p-value=0.000), and use of N95 in combination with a surgical mask (P=0.04) (Table 6).
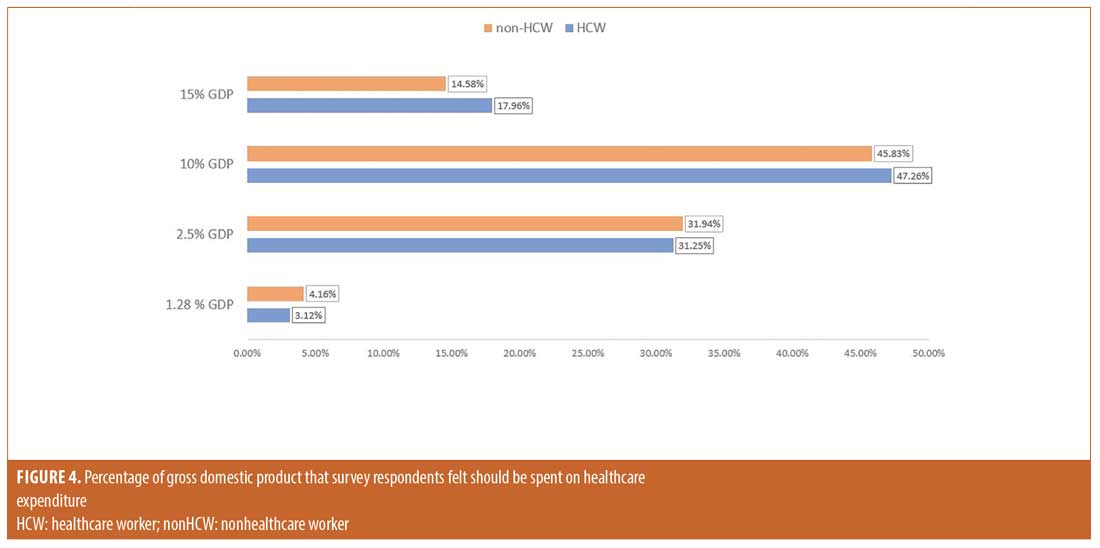
Perceptions and impact of the pandemic. Healthcare expenditure. Most HCWs (47.26%) and nonHCWs (45.83%) felt that 10 percent of the gross domestic product (GDP) should be allocated to healthcare expenditure (Figure 4).
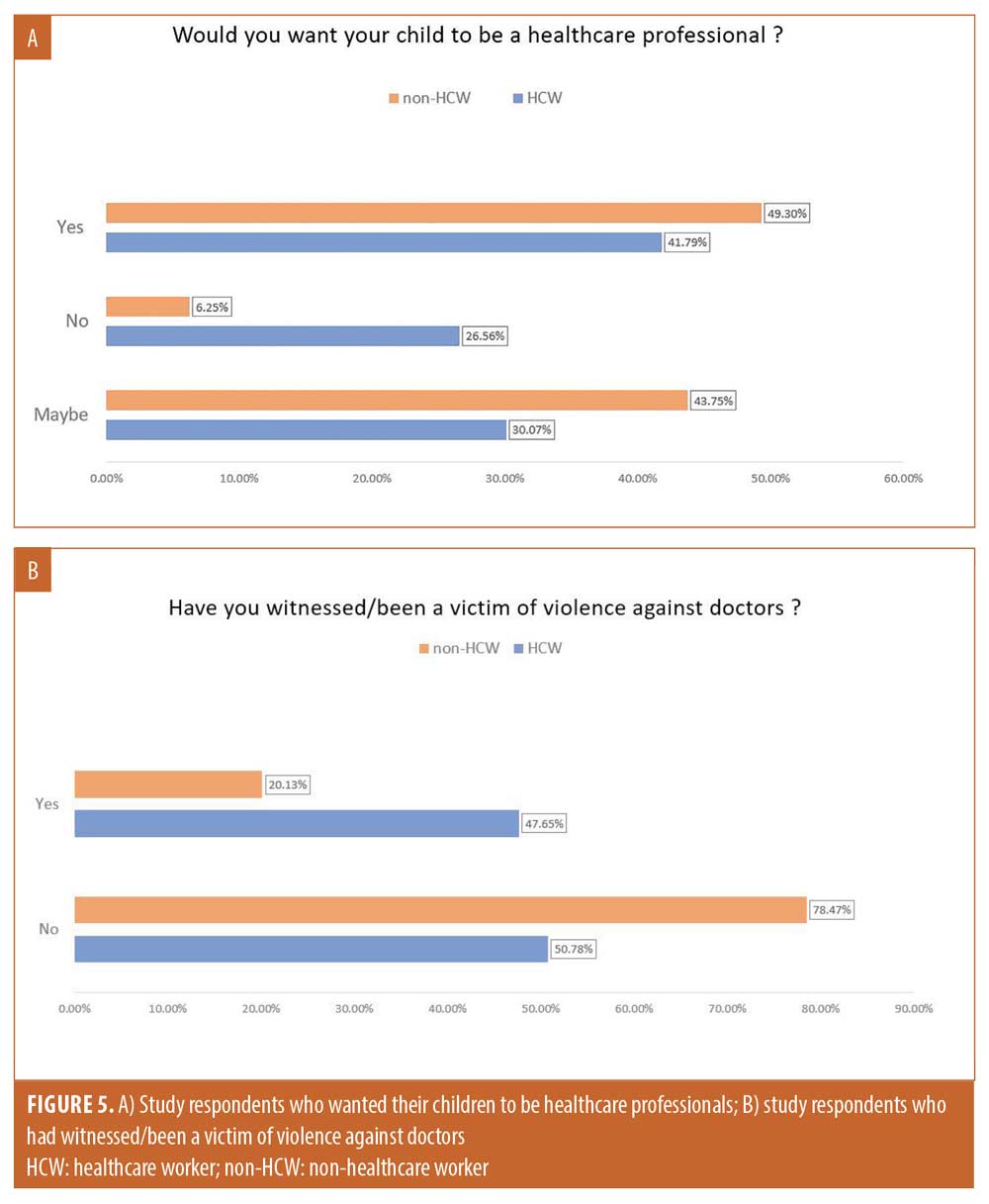
Preference for medical profession. A higher number of HCWs did not want their children to be healthcare professionals, compared to nonHCWs. This difference was statistically significant (P<0.001) (Figure 5a).
Perception of frontline workers. More than 90 percent of respondents “strongly agreed” or “agreed” that doctors, nurses, and other frontline workers deserve respect and admiration equal to the armed forces (HCWs: 91%, nonHCWs: 90.96%).
Perceived stress of the pandemic. Fifty-eight percent (58.91%) of respondents, with a statistically significant number of HCWs compared to nonHCWs (HCWs: 65.23%, nonHCWs: 47.22%, P<0.001), felt there should be mandatory psychological counseling for everyone due to the extraordinary stress of the pandemic. Slightly more HCWs than nonHCWs felt stressed and burdened by the recommended hand hygiene routine and mask wearing due to the COVID-19 pandemic (HCWs: 32.41%, nonHCWs: 30.56%).
On applying Spearman’s correlation, we found that as the age of respondents increased, their tendency to agree with being burdened and stressed by the recommended hand hygiene practice and mask usage increased (P<0.000).
There was a statistically significant correlation found between regular mask usage and stress perceived (P=0.012).
No significant correlation was found between the burden and stress perceived with occupation (HCW vs. nonHCW) (P=0.805), frequency and method of hand hygiene (P=0.940 and 0.562, respectively), and use of latex gloves or moisturizers (P=0.213 and 0.293, respectively).
Violence against doctors. Overall, 37.9 percent of respondents have witnessed/been a victim of violence against doctors, with a higher percentage among HCWs than nonHCWs, the difference being statistically significant (P<0.0001) (Figure 5b).
Bias. To ascertain the bias in this study, we used the risk of bias instrument for cross-sectional survey of attitudes and practice.15 (Risk of bias: representative sample: high; adequacy of response rate: low; missing data: low; conduct of pilot testing: high; validation of survey instrument: high).
Discussion
As with any new infectious agent appearing on the global scene, a lack of factual scientific knowledge was a great deterrent to the effective management of COVID-19 initially. It was originally believed to be a disease originating from animals, possibly bats, and the wet markets of Wuhan were the alleged epicenter, with no clear evidence of human-to-human transmission at that time.16
With COVID-19 being a droplet infection, masks were initially advised only for healthcare professionals, but as more evidence emerged, the WHO recommended masks for the general population as well.18 Owing to the size of the SARS-COV2 virus, N95 masks were initially deemed unnecessary; however, N95 masks were then recommended for HCWs in COVID-19-affected areas.19 The mode of spread still remains circumspect, with the United Statesn Centers for Disease Control and Prevention (CDC) going back and forth on the issue of aerosol transmission.20 Consequently, masks, social distancing, and hand hygiene have become a universally accepted means to prevent COVID-19 spread in communities. India has been diligent in promoting this with the slogan “Do gaz ki doori, mask hai zaroori” (Six feet apart, wear a mask) made popular by our prime minister. This recommendation has been largely followed by Indians, HCWs and nonHCWs alike. In our study, we found that 87.4 percent of respondents “always” wore a mask; this is a considerably high percentage, especially compared to countries without a government mandate on masks, such as the United States (US), where mask wearing is not federally enforced.20 This would explain lesser the severity and significantly lower mortality seen in India, as even a cloth or simple survival mask can decrease the inoculum of the infection (mortality rate as of October 13, 2020: India=1.5%; US=2.7%).22,23 Severity of the disease, particularly cytokine storm, has been reported to correlate with the initial exposure inoculum.24
India’s response to the pandemic has been noteworthy and deserves mention here, with an early lockdown for capacity building before cases rose, free state-sponsored testing, and quick mobilization of an already robust grassroots cadre of public health infrastructure.
The Aarogya setu, a government mobile application for tracking cases, became the world’s fastest growing application; since its launch, it has been downloaded more than 150 million times.27 Its merits and role in pandemic mitigation in India have received commendation by the Director General of the WHO.27 An equivalent application for the state of Punjab, called COVA, has been equally effective. This effectiveness is reflected in our findings, as among both HCWs and nonHCWs, government guidelines/Arogya setu application/COVA Punjab application were the most common sources of information regarding preventive measures and information during the pandemic. Other authors have reported television and social media as the main sources of information during the pandemic.25,26
When comparing the groups, as expected, the frequency of hand hygiene is higher among HCWs. HCWs, who are unable to protect themselves from the pandemic by a work-from-home option, have a considerably higher risk of exposure, even when working in non-COVID-19 zones. This concurs with a Nigerian study that reported more frequent hand washing among individuals who perceived themselves as vulnerable to COVID-19.28
More HCWs have reported a marked change in their hand hygiene routine ever since the pandemic compared to nonHCWs. This would be expected, as in most places, healthcare resources have been diverted to COVID-19 and more stringent infection control practices. No previously published data is available comparing HCWs and non-HCWs during the COVID-19 pandemic to the best of our knowledge.
Consequential to this practice, we found a higher incidence of hand eczema in HCWs. Lan et al29 reported skin damage in 74.5 percent of frontline HCWs (study participants: 526) due to the stringent infection prevention methods, particularly among those who washed their hands more than 10 times a day. However, these were HCWs who donned personal protective equipment working with COVID-19 patients. Occupational hand eczema is a well-described entity among HCWs in particular.30,31 This concurs with our findings. Use of moisturizers on intact skin after washing has been recommended by other authors as well.29,32 Most respondents reported regular moisturizer use. Development of dryness correlated with hand hygiene frequency; this finding is comparable to studies conducted prior to the pandemic. In one such survey of 242 HCWs working in a surgical unit, 47 percent (114) of participants developed skin discomfort or hand eczema due to frequent scrubbing.33
The deleterious effects of prolonged mask wearing are only beginning to emerge. Han et al34 have reported increased flares of acne due to mask usage in two dozen patients who were all involved in healthcare-associated occupations. Five of them had their initial episode of acne after mask use in the COVID-19 pandemic. This is similar to our finding where only two of the 44 respondents with acne were nonHCWs.
The lesson to be learned from this pandemic is that government spending to strengthen the existing public healthcare infrastructure should be increased. The Indian government spent only 1.28 percent (3.2% including private) of its GDP on healthcare in 2019, compared to 10.4 percent of Denmark’s GDP.35,36 Violence against doctors is perhaps a problem unique to the Indian sub-continent and should be addressed. The IMA reported that 75 percent of doctors in India have faced violence at some point in their lives.37 This is reflected by our findings, where a lesser number of HCWs wish to see their children become doctors. Long-term, this could lead to a gradual undermining of the healthcare sector, and the brightest minds would be diverted toward other professions.
Limitations. As this was an online survey, we could not capture responses from the areas with the restricted internet facilities, including economically weaker sections of society, or those not well versed in English. Secondly, respondents may have given false information, as it was a self-administered online questionnaire. Lastly, it was not possible to have age- and sex-matched groups for comparing HCWs and nonHCWs.
Conclusion
The frontline workers in India deserve our support, respect, and empathy, not through symbolic gestures during the pandemic, but on all those countless occasions where they put duty before self. To conclude, there is a considerable burden of preventive measures on HCWs and nonHCWs alike. Significant dermatological implications are seen with frequent hand hygiene and mask usage. As the pandemic winds down, further effects of these practices will emerge.
References
- Rothan HA, Byrareddy SN. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J Autoimmun. 2020;109:102433.
- Wuhan Municipal Health Commission. Report of clustering pneumonia of unknown etiology in Wuhan City. Wuhan, China. 31 Dec 2019. http://wjw.wuhan.gov.cn/front/web/showDetail/2019123108989. Accessed October 21, 2020.
- Nishiura H, Jung SM, Linton NM, et al. The extent of transmission of novel coronavirus in Wuhan, China, 2020. J Clin Med. 2020;9(2):330
- Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Biomed. 2020;91(1):157–160
- World Health Organization. Naming the coronavirus disease (COVID-19) and the virus that causes it. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it. Accessed October 13, 2020.
- World Health Organization. Coronavirus disease 2019 (COVID-19) situation report-51. Geneva: World Health Organization. https://covid19.who.int/region/searo/country/in. Accessed March 5, 2020.
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395(10223):497–506.
- Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet. 2020;395(10223):514–523.
- WHO Director-General’s opening remarks at the media briefing on COVID-19. 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19-11-march-2020. Accessed October 13, 2020.
- United States Centers for Disease Control and Prevention. Clean hands count for healthcare providers. 2020. https://www.cdc.gov/handhygiene/providers/index.html. Accessed September 30, 2020.
- Doctor patient ratio in India. [Internet]. 164.100.47.190. 2018. Available at: http://164.100.47.190/loksabhaquestions/annex/12/AS86.pdf. Accessed October 13, 2020.
- High level expert group report on universal health coverage for India Planning Commission of India. New Delhi, November 2011. http://planningcommission.nic.in/reports/genrep/rep_uhc0812.pdf. Accessed October 13, 2020.
- Mascarenhas A. IMA flags 800 doctor deaths in second wave. The Indian Express. July 1, 2021
- Didyala A. Ruckus at Gandhi hospital as COVID victim’s kin attack doctors. The Times of India. June 10, 2020;A:2 (col 4).
- Iqbal S, Gupta S, Venkatarao E. Stress, anxiety and depression among medical undergraduate students and their socio-demographic correlates. Indian J Med Res. 2015;141(3):354.
- Agarwald A, Guyatt G, Busse J. Methods commentary: risk of bias in cross-sectional surveys of attitudes and practices. https://www.evidencepartners.com/wp-content/uploads/2017/04/Methods-Commentary-Risk-of-Bias-in-cross-sectional-surveys-of-attitude….pdf. Accessed October 21, 2020.
- World Health Organization. Novel coronavirus–China. January 12, 2020. https://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/. Accessed October 13, 2020.
- World Health Organization. World Health Organization (WHO) Coronavirus disease (COVID-19) advice for the public: when and how to use masks. 2020. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public/when-and-how-to-use-masks. Accessed October 13, 2020
- United States Centers for Disease Control and Prevention. Pandemic planning: recommended guidance for extended use and limited reuse of N95 filtering facepiece respirators in healthcare settings. 2020. Available at: https://www.cdc.gov/niosh/topics/hcwcontrols/recommendedguidanceextuse.html. Accessed October 13, 2020.
- Morawska L, Milton DK. It is time to address airborne transmission of COVID-19. Clin Infect Dis. 2020;6:ciaa939.
- United States Centers for Disease Control and Prevention. CDC calls on Americans to wear masks to prevent COVID-19 spread. https://www.cdc.gov/media/releases/2020/p0714-americans-to-wear-masks.html. Accessed October 21, 2020.
- United States Centers for Disease Control and Prevention. CDC COVID data tracker. https://covid.cdc.gov/covid-data-tracker/#cases_totaldeaths. Accessed October 16, 2020.
- Ministry of Health and Family Welfare.https://www.mohfw.gov.in/index1.php?lang=1level=1subli nkid=6471lid =4270, Accessed October 16, 2020.
- Castelli V, Cimini A, Ferri C. Cytokine storm in COVID-19: “When you come out of the storm, you won’t be the same person who walked in.” Front Immunol. 2020;11:2132.
- Narayana G, Pradeepkumar B, Ramaiah JD, et al. Knowledge, perception, and practices towards COVID-19 pandemic among general public of India: a cross-sectional online survey. Curr Med Res Pract. 2020;10(4):153–159.
- Reuben RC, Danladi MMA, Saleh DA, Ejembi PE. Knowledge, attitudes and practices towards COVID-19: an epidemiological survey in north-central Nigeria. J Community Health. 2020:1–14.
- WHO lauds Aarogya Setu app, says it helped to identify COVID. The Times of India. Updated October 13, 2020. https://timesofindia.indiatimes.com/business/india-business/who-lauds-aarogya-setu-app-says-it-helped-to-identify-covid-19-clusters/articleshow/78637254.cms. Accessed October 15, 2020.
- Ilesanmi O, Afolabi A. Perception and practices during the COVID-19 pandemic in an urban community in Nigeria: a cross-sectional study. Peer J. 2020;8:e10038.
- Lan J, Song Z, Miao X, et al. Skin damage among healthcare workers managing coronavirus disease-2019. J Am Acad Dermatol. 2020;82(5):1215–1216.
- Skoet R, Olsen J, Mathiesen B, et al. A survey of occupational hand eczema in Denmark. Contact Dermatitis. 2004;51(4):159–166.
- Flyvholm MA, Bach B, Rose M, Jepsen KF. Self-reported hand eczema in a hospital population. Contact Dermatitis. 2007;57(2):110–115.
- Yan Y, Chen H, Chen L, et al. Consensus of Chinese experts on protection of skin and mucous membrane barrier for healthcare workers fighting against coronavirus disease 2019. Dermatol Ther. 2020:e13310.
- Barfred L, Rasmussen HH, Andersen KE. [Incidence of hand eczema after surgical washing and use of surgical gloves]. Ugeskr Laeger. 1993;155(17):1258–1261.
- Han C, Shi J, Chen Y, Zhang Z. Increased flare of acne caused by longtime mask wearing during COVID-19 pandemic among general population. Dermatol Ther. 2020:e13704.
- Ministry of Finance. Social infrastructure, employment and human development. In: Ministry of Finance. Economic Survey 2020-21. 2020;2:325–368. Available at: https://www.indiabudget.gov.in/economicsurvey/doc/vol2chapter/echap10_vol2.pdf. Accessed October 20, 2020.
- State of health in the EU Denmark country health profile 2019. https://ec.europa.eu/health/sites/health/files/state/docs/2019_chp_da_english.pdf. Accessed October 20, 2020.
- Reddy IR, Ukrani J, Indla V, Ukrani V. Violence against doctors: a viral epidemic? Indian J Psychiatry. 2019;61(Suppl 4): S782–S785.

