 J Clin Aesthet Dermatol. 2019;12(4):38–39
J Clin Aesthet Dermatol. 2019;12(4):38–39
by Shimona Garg, MD; Anand Kumar, MD; Mala Bhalla, MD; Amrit Kaur, MD; and Raj Pal Singh Punia, MD
Drs. Garg, Kumar, Bhalla and Kaur are with the Department of Dermatology, Venereology, and Leprosy and Dr. Punia is with the Department of Pathology—All from the Government Medical College and Hospital in Chandigarh, India
FUNDING: No funding was received for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Atypical forms of psoriasis are frequently seen. However, linear psoriasis precipitated by drugs is extremely rare. We report a case of an adult woman who presented with lithium-induced unilateral psoriasis arranged in Blaschko lines on the left leg. A brief discussion on etiology and differential diagnosis is included, as well as treatment methods.
KEYWORDS: Psoriasis, lithium, linear, Blaschko lines
Psoriasis is a common papulosquamous disorder characterized by sharply demarcated, erythematous plaques with silvery white scales. The exact etiopathogenesis is unknown but psoriasis is thought to be caused by an altered immunological response in genetically predisposed individuals that is triggered by various environmental factors, such as stress, cold environment, medication, or infection. Medications that commonly trigger or aggravate psoriasis include antimalarials, beta-blockers, lithium, and ace inhibitors.1 Psoriasis arranged linearly or along Blaschko lines is an uncommon condition.2 We were unable to find any case reports in the literature linking the onset of linear psoriasis with lithium. Here, we present the first reported case of linear psoriasis induced by lithium.
Case Report
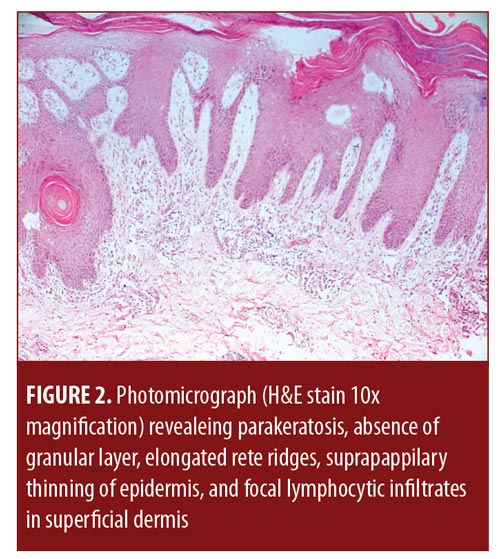
A 36-year-old woman presented with pruritic linear lesions that had appeared three weeks earlier over the posterior aspect of her left lower leg. The lesions initially appeared on the left thigh and progressed distally down to the ankle. The patient had been taking 900mg of lithium for the previous three months for treatment of bipolar disorder. There was no history of trauma or skin lesions elsewhere on the body. No other family members had similar lesions. An examination revealed well-defined, erythematous, scaly papules and plaques arranged linearly along Blaschko lines over the posterior surface of the left thigh and extending to ankle (Figure 1). Nails, hair, and mucosae were normal. There was no joint involvement. Systemic examination did not reveal any abnormality. Routine hematological investigations, including complete hemogram, liver function, and renal function, were within normal limits. Skin biopsy was taken, and histopathology revealed parakeratosis, absence of granular layer, elongated rete ridges, suprapapillary thinning of the epidermis, and focal lymphocytic infiltrates in the superficial dermis (Figure 2). Thus, the diagnosis of linear psoriasis was established. The dose of lithium was reduced to 450mg, and alternative drug therapy, olanzapine 5 mg once daily, was initiated for treatment of her bipolar disorder. The patient was also treated with topical clobetasol propionate and calcipotriol. After four weeks, the patient developed typical psoriatic lesions in a generalized distribution. The lithium was discontinued after consultation with the psychiatric team. With continued topical therapy, the lesions improved significantly over the next 2 to 3 months. Rechallenge with lithium was offered to the patient, which she refused.

Discussion
Psoriasis is commonly triggered or aggravated by antimalarials, beta-blockers, lithium, nonsteroidal anti-inflammatory drugs, angiotensin-converting enzyme inhibitors, interferons, selective serotonin reuptake inhibitors, benzodiazepines, and the immediate withdrawal of systemic or potent topical corticosteroids.1 Lithium has been linked to exacerbation of pre-existing psoriasis or inducing psoriasis de novo.3 The exact mechanism by which lithium affects psoriasis is unknown, but it is thought to modulate adenyl cyclase and inositol monophosphate-mediated pathways, resulting in a reduced intracellular concentration of calcium as well as increased proliferation and reduced differentiation of keratinocytes. Lithium-induced psoriasis reported in the literature includes new onset of chronic plaque psoriasis, pustular psoriasis, palmoplantar pustulosis, erythroderma, psoriasiform dermatitis, psoriatic arthropathy, and psoriasis involving the nail and scalp.4 The most common presentation of lithium-induced psoriasis is psoriasis vulgaris.5 Lithium-induced psoriasis can become treatment-resistant, which might warrant the discontinuation of lithium.6 Reduction in the dosage of lithium is another option for treatment-resistant cases.4 However, lithium-induced psoriasis has been reported to occur at varying therapeutic levels and is not believed to be dose-related.6
Linear psoriasis is a rare variation of psoriasis that can occur as an isolated form or with other psoriatic lesions,2 though its exact pathogenesis is unknown. It is hypothesized that a patient affected by linear psoriasis is heterozygous for one or more of the genes linked to psoriasis vulgaris; however, in order for linear psoriasis to manifest, an external/environmental factor or trigger must also be present, in addition to the genetic component.7 In the literature, linear psoriasis induced by lithium has not been reported. In our case, lithium acted as the external precipitating factor that led to the appearance of psoriasis in a linear distribution.
Linear psoriasis might be confused with inflammatory linear verrucous epidermal nevus (ILVEN), which tends to develop during the early years of life, is slowly progressive, and is usually unresponsive to treatment.8 Linear psoriasis, on the other hand, tends to develop later in life, is rapidly progressive, and responds to antipsoriatic treatment.9 The histological features of ILVEN include hypergranulosis and parakeratosis alternating with hypogranulosis and orthokeratosis. The classic histological features of psoriasis include hyperkeratosis, parakeratosis, the absence of granular cell layers, an elongation of rete ridges, suprapapillary thinning, and Munro’s microabscesses, which can also be seen in ILVEN.10
Like common forms of localized psoriasis, linear psoriasis usually responds to topical steroids, keratolytics, and calcipotriol, but recurrences are common. Lithium-induced psoriasis typically does not respond to antipsoriatic treatment and might warrant the discontinuation of lithium.
References
- Brauchli YB, Jick SS, Curtin F, Meier CR. Lithium, antipsychotics, and risk of psoriasis. J Clin Psychopharmacol. 2009;29(2):134–140.
- Chien P Jr, Rosenman K, Cheung W, et al. Linear psoriasis. Dermatol Online J. 2009;15(8):4.
- Sarantidis D, Waters B. A review and controlled study of cutaneous conditions associated with lithium carbonate. Br J Psychiatry. 1983;143: 42–50.
- Jafferany M. Lithium and psoriasis: what primary care and family physicians should know. Prim Care Companion J Clin Psychiatry. 2008;10(6):435–439.
- O’Brian M, Koo J. The mechanism of lithium and beta-blocker agents in inducing and exacerbating psoriasis. J Drugs Dermatol. 2006;5(5):426–433.
- Tsankov N, Kazandjieva J, Drenovska K. Drugs in exacerbation and provocation of psoriasis. Clin Dermatol. 1998;16(3):333–351.
- Happle R. Somatic recombination may explain linear psoriasis. J Med Genet. 1991;28(5):337.
- De Jong E, Rulo HF, Van De Kerkhof PC. Inflammatory linear verrucous epidermal naevus (ILVEN) versus linear psoriasis. a clinical, histological and immunohistochemical study. Acta Derm Venereol. 1991;71(4):343–346.
- Saraswat A, Sandhu K, Shukla R, Handa S. Unilateral linear psoriasis with palmoplantar, nail, and scalp involvement. Pediatr Dermatol. 2004;21(1):70–73.
- Miteva LG, Dourmishev AL, Schwartz RA. Inflammatory linear verrucous epidermal nevus. Cutis. 2001;68(5):327–330.

