 Lip tattoo darkening after Q-switched laser hair removal followed by significant spontaneous improvement
Lip tattoo darkening after Q-switched laser hair removal followed by significant spontaneous improvement
J Clin Aesthet Dermatol. 2022;15(4):10
Dear Editor:
Q-switched (QS) lasers are known to cause permanent darkening of some tattoos including those that are red, pink, or skin-colored.1 This is especially true for cosmetic lip and eyebrow tattoos.2 Hair removal using QS lasers is popular in our country as it is relatively quick and painless as compared to conventional laser hair removal (LHR) using long-pulsed mode. We report a case of lip tattoo darkening after QS LHR that spontaneously improved afterwards.
A 30-year-old female was being evaluated at our dermatology clinic for generalized vitiligo that she had for more than 10 years. She was receiving treatment with narrowband UVB and tacrolimus 0.1% ointment. During one of her follow up visits, she had prominent darkening of her lips (Figure 1). Six years ago, she had a cosmetic pink lip tattoo. A few weeks prior to her visit to our clinic, she underwent Q-switched 1064 nm LHR around the mouth (Spectra, Lutronic, Korea). Darkening of the lips developed within two days. After approximately two months, the darkening significantly improved without any treatment (Figure 1).
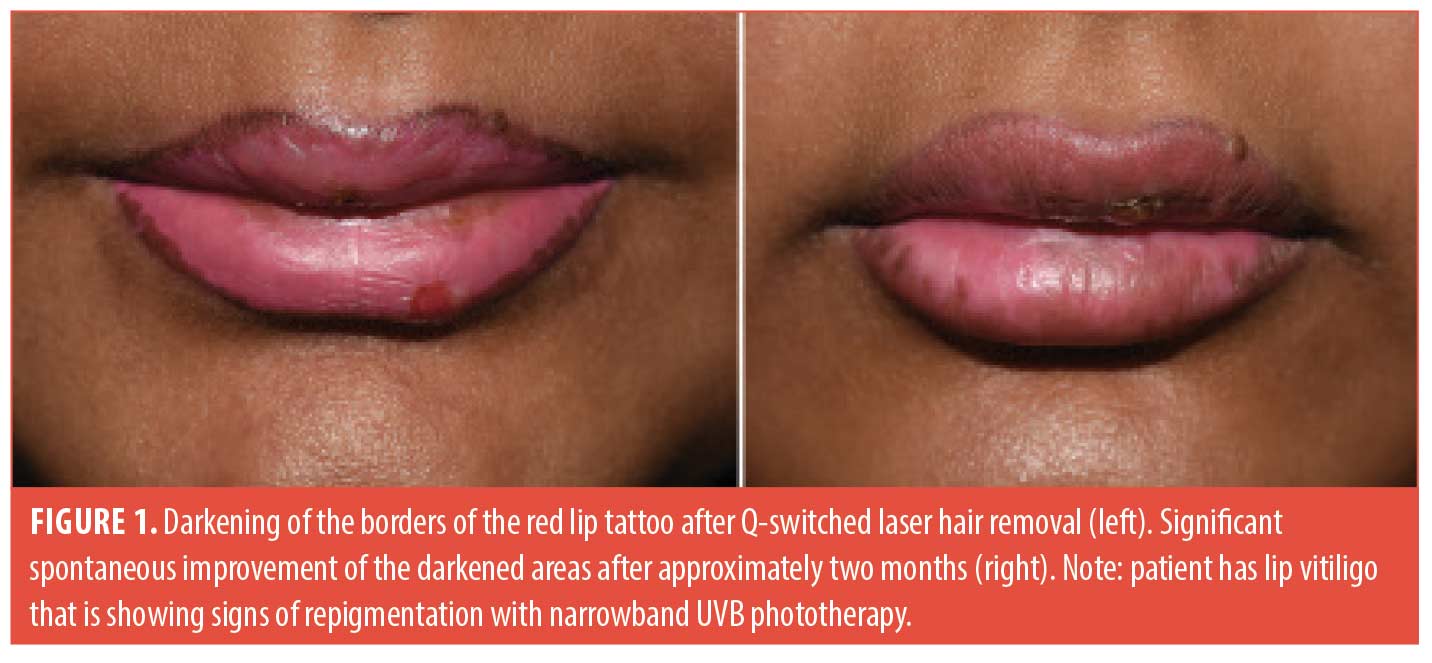
Paradoxical darkening of red or pink tattoos after QS laser usually occurs due to reduction of ferric oxide to ferrous oxide.2 This complication is thought to be irreversible. However; it can be corrected with either continued QS laser treatment or ablative laser resurfacing.2,3 Our case has two interesting points. First, paradoxical darkening occurred after an unconventional use of QS laser, which is hair removal. Second, the darkening resolved spontaneously which was never reported to the best of our knowledge.
The spontaneous resolution could be due to the initial fragmentation of the tattoo particles by QS laser treatment. The fragmented darkened tattoo particles were then possibly eliminated by macrophages or via lymphatics over several months.4 Furthermore, previously reported improvement of paradoxical darkening with continued QS laser treatment might have been due to both time and additional fragmentation of tattoo particles in each session. It is not clear if tacrolimus ointment application has played a role in the observed improvement in our patient. In fact, we have seen a few patients in the past in whom paradoxical darkening spontaneously improved without tacrolimus application.
We recommend that all patients must be asked about having done a cosmetic lip and/or eyebrow tattoo before undergoing QS LHR around the mouth or for the eyebrows. Some cases of paradoxical darkening might significantly improve without further treatment. This might help in reassuring patients who develop this complication, however; more studies are required to confirm this finding.
With regard,
Mohammed I. Al-Jasser, MBBS FRCPC, and Ahmed Al-Issa, MBBS, FRCPC
Affiliations. Dr. Al-Jasser is with the Division of Dermatology at King Saud bin Abdulaziz University for Health Sciences and King Abdullah International Medical Research Center in Riyadh, Saudi Arabia. Dr. Al-Issa is with the Derma Clinic in Riyadh, Saudi Arabia.
Funding. No funding was provided for this article.
Disclosures. The authors declare no conflicts of interest relevant to the content of this article.
References
- Naga LI , Alster TS. Laser tattoo removal: An Update. American Journal of Clinical Dermatology. 2017;18(1):59–65.
- McIlwee BE , Alster TS. Treatment of cosmetic tattoos: A Review and Case Analysis. Dermatologic Surgery. 2018;44(12):1565–1570.
- Kirby W, Kaur RR , Desai A. Paradoxical darkening and removal of pink tattoo ink. Journal of Cosmetic Dermatology. 2010;9(2):149–151.
- Choudhary S, Elsaie ML, Leiva A , Nouri K. Lasers for tattoo removal: a review. Lasers in Medical Science. 2010;25(5):619–627.
Anatomical Exhortations of Botulinum Toxin Injections for Rosacea
J Clin Aesthet Dermatol. 2022;15(4):12
Dear Editor:
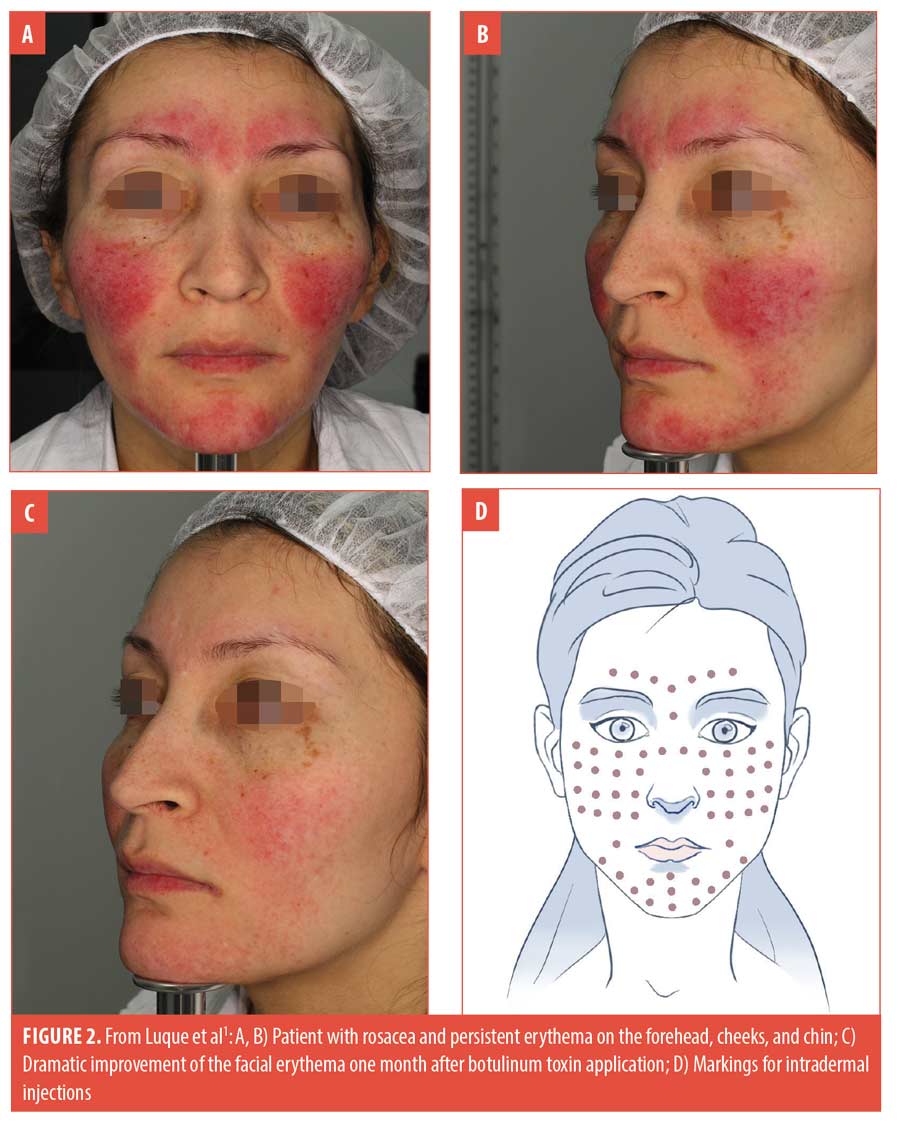
We read Luque and colleague’s informative series on the use of botulinum toxin in the treatment of flushing and erythema in rosacea with interest.1 The authors mark the sites for the intradermal injections in Figure 2 (D). Extreme caution is required when injecting in this area since the depressor anguli oris muscle has a medial border which overlaps with the depressor labii inferioris. We note that the injection points on the chin in their image are on the “no-go zone” on the depressor labii inferioris and injecting into this area might result in drooping of the lower lip, slurring, drooling and dribbling in patients receiving the botulinum toxin. This protrusion of the lower lip has been referred to as a Gomer Pyle appearance.2 This can lead to the appearance of asymmetry in the perioral region possibly resulting in the need for a further botulinum injection on the contralateral side so that both sides are symmetrical. In addition, if botulinum is injected too laterally, the buccinator muscle might be reached causing the patient to bite down and damage their buccal mucosa.2 A thorough understanding of the anatomy of the facial muscles is therefore essential when treating the perioral area with botulinum toxin to ensure the safe delivery of this medication.
With regard,
Tamara Searle, BSc; Faisal R. Ali, PHD, MRCP; and Firas Al-Niaimi, MRCP
Affiliations. Dr. Searle is with the University of Birmingham Medical School in Birmingham, United Kingdom. Dr. Ali is with the Dermatological Surgery & Laser Unit, St John’s Institute of Dermatology, Guy’s and St Thomas’ NHS Foundation Trust in London, United Kingdom. Dr. Al-Niaimi is with the Department of Dermatology, and Aalborg University Hospital in Aalborg, Denmark.
Funding. No funding was provided for this article.
Disclosures. The authors declare no conflicts of interest related to the content of this article.
References
- Luque A, Rojas AP, Ortiz-Florez A, Perez-Bernal J. Botulinum Toxin: An Effective Treatment for Flushing and Persistent Erythema in Rosacea. J Clin Aesthet Dermatol. 2021;14(3):42–45.
- Mostafa D. Botulinum Toxin in Dentistry, Botulinum Toxin, Nikolay Serdev, IntechOpen, 2018; Available from: https://www.intechopen.com/books/botulinum-toxin/botulinum-toxin-in-dentistry.

