Dear Editor:
Onychocryptosis, or ingrown nail (IN) is a common problem in dermatology clinical practice. Its prevalence is estimated to be from 2.5 to 5 percent, with a predominance in males.1 The incidence has a bimodal age-related peak: it appears to be higher among teenagers and young adults, but also shows a strong predominance in individuals who are 60 or older.1
Generally a post-traumatic condition, onychocryptosis of the fingernails is uncommon, with few literary cases,2 and lacks consensus for correct management. Here, we report the case of a patient with recurring onychocryptosis affecting the fourth finger of the left hand.
Case report. A 24-year-old female patient was admitted to our surgery with a bilateral periungual granuloma of the fourth finger of the left hand caused by damage to the lateral skin due to improper blade placement during an aesthetic treatment. No traumatic stress of the nail was reported. The patient reported spontaneous pain, bleeding, swelling, and infection, and had pluri-recurrent ingrown nail consecutively treated by four different surgeons performing different procedures informed by the literature: several partial wedge resections, two laser removals of the granulomas, a total avulsion of the nail and a partial bilateral matricectomy of the lateral nail plate by electrocauterization.3,4
The patient was treated with antibiotics and steroids before and after any interventions and silver nitrate for the devascularization of the granuloma. None of these treatments was resolutive, and the nail continued to grow and pierce the lateral skin, even after the partial matricectomy.
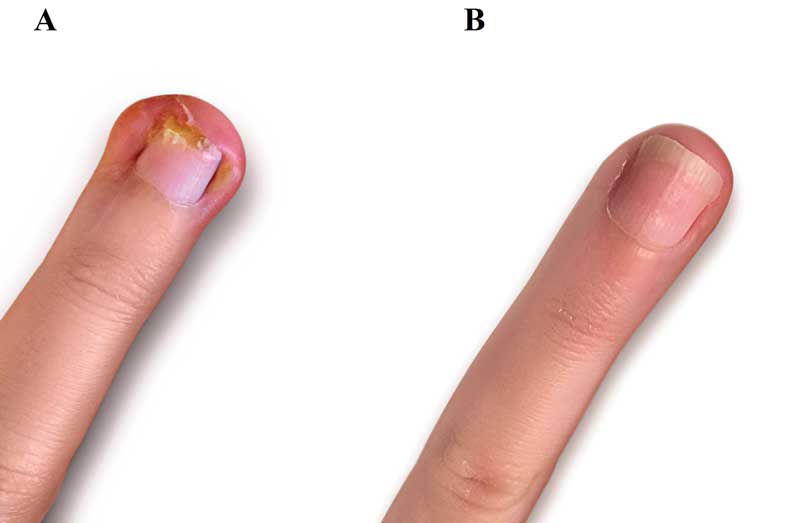
As a tenth treatment attempt, we opted for an outpatient Vandenbos procedure,5 which consisted of the excision of the skin fold only, and without partial nor total removal of the nail. It allowed the nail to grow normally and avoided any trauma to the matrix. We performed a small cut of the edges of the nail to allow healing of the lateral skin before nail growth (Figure 1).
Our first intervention was a nerve block anesthesia with 5cc lidocaine, made on both lateral bases of the finger, with local anesthesia on the top of the finger to provide less operative and postoperative pain. The nail and the matrix were left intact, and the wounds were left open to granulate and epithelialize.
Hemostasis was obtained by a very tight dressing, changed after two days and then after a week. The patient reported postoperative pain because of the open wounds and was treated with ketorolac for four days. Complete wound re-epithelization was obtained after four weeks, with a reduction of lateral skin tissue. After complete nail growth, a new granuloma emanated from the skin above the medial edge of the nail.
To avoid another surgical operation, we opted for the insertion of a wound closure strip under the nail, to separate it from the nail bed. It was removed after skin fold healing with no infection or granuloma formation. At the six-month follow-up visit, the patient showed no signs of recurrence (Figure 2).
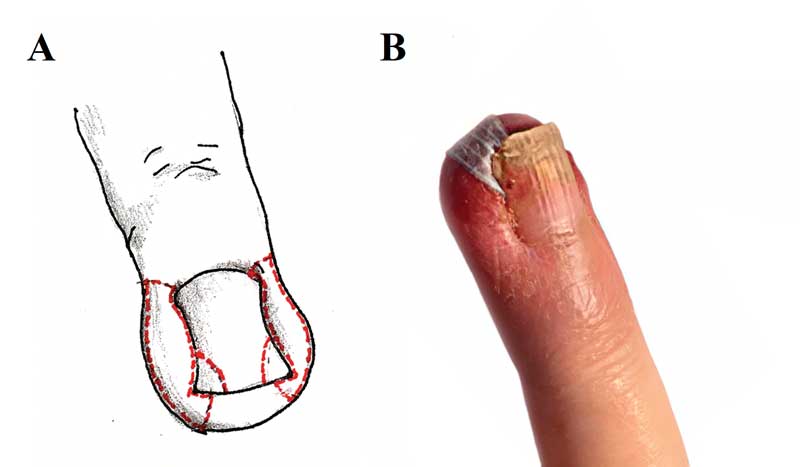
In conclusion, we believe that for the anecdotal cases of ingrown fingernail, and for the more uncommon cases of recurrent and pluri-recurrent ingrown fingernail, a good alternative treatment could consist of combining the Vandenbos procedure with a small cut of the edges of the nail, followed by the placement of a wound closure strip under the nail, in order to reduce the trauma and to gain a better aesthetic result and in shorter time compared to the nail’s total avulsion.
Acknowledgment. We wish to thank the Scientific Bureau of the University of Catania for language support. Our thanks also go to the Prof. Angelo Di Chio, Associate Professor of the Department of Engineering at Mediterranea University of Reggio Calabria in Italy, for the creation of Figure 2.
Michela Zanatta, MD; Francesco Basile, MD; Guido Basile, MD; and Marcello Donati, MD
Affiliations. Drs. Zanatta, Donati, and F. Basile are with the Department of Surgery and Medical-Surgical Specialties for the Surgical Clinic Unit at the University Hospital of Catania, University of Catania in Italy. Dr. G. Basile is with the Department of Surgery and Medical- Surgical Specialties for the Emergency and Abdominal Surgery Unit at the University Hospital of Catania, University of Catania in Italy.
Funding. No funding was provided.
Disclosures. The authors have no conflicts of interest relevant to the content of this article.
REFERENCES
- Cho SY, Kim YC, Choi JW. Epidemiology and bone-related comorbidities of ingrown nail: A nationwide population-based study. J Dermatol. 2018;45(12):1418–1424.
- Eke N, Little K. An embedded fingernail. Postgrad Med J. 1982;58(32).
- Heidelbaugh JJ and Lee H. Management of the ingrown toenail. Am Fam Physician. 2009;79(4). 303–308.
- Haneke E. Controversies in the treatment of ingrown nails. Dermatol Res Pract. 2012;2012(783924).
- Livingston MH, Coriolano K, Jones SA. Nonrandomized assessment of ingrown toenails treated with excision of skinfold rather than toenail (NAILTEST): An observational study of the Vandenbos procedure. European J Pediatr Surg Rep. 2017;52:832–836.

