 J Clin Aesthet Dermatol. 2020;13(5):24–27
J Clin Aesthet Dermatol. 2020;13(5):24–27
by Anny Xiao, DO; Renee Lucero, DO; and William T. Kirby, DO, FAOCD
Drs. Xiao, Lucero, and Kirby are with the Western University of Health Sciences in Pomona, California. Dr. Kirby is also with LaserAway in Hermosa Beach, California.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Perioral cosmesis is an important component of facial aesthetics. The perioral region is prone to revealing signs of aging due to repetitive movements and various environmental factors. While it is well established that perioral aesthetics can be effectively treated with hyaluronic acid dermal filler, there is limited published data available on injection techniques specifically designed for perioral rejuvenation. In this article, we review the perioral anatomy and current percutaneous filler injection techniques for perioral cosmesis. We then present a novel intraoral filler injection approach to improve perioral aesthetics with minimal downtime and high patient satisfaction.
Keywords: Perioral, filler, hyaluronic acid, intraoral, injection, aesthetics
Injectable fillers for facial rejuvenation have become one of the most frequently performed nonsurgical cosmetic procedures in the United States.1 Over the last decade, soft-tissue augmentation with fillers has experienced a rapid increase in procedural volume, reflecting a growing demand for minimally invasive methods for aesthetic enhancement.2,3 Perioral aesthetics play an integral role in maintaining a youthful appearance. Aging of the perioral area can result from repetitive contraction of the perioral muscles, sun exposure, thinning of the skin, atrophy of subcutaneous fat, and ptosis of the malar fat pads.4 Volume loss from the nasolabial and labiomandibular folds leads to deeper creases and shadows. The lips become thinner with decreased definition in the vermilion border and loss of subcutaneous fat in surrounding skin accentuates the perioral fine wrinkles from repetitive orbicularis oris contraction.4 Injections of hyaluronic (HA) acid filler can address many of these concerns in the perioral region to provide optimal facial harmony and rejuvenation. In this article, we briefly review current perioral filler implementation techniques and present a novel intraoral injection technique specifically designed to improve cosmesis of the perioral region with minimal downtime and high patient satisfaction.
Perioral Anatomy and Aesthetics
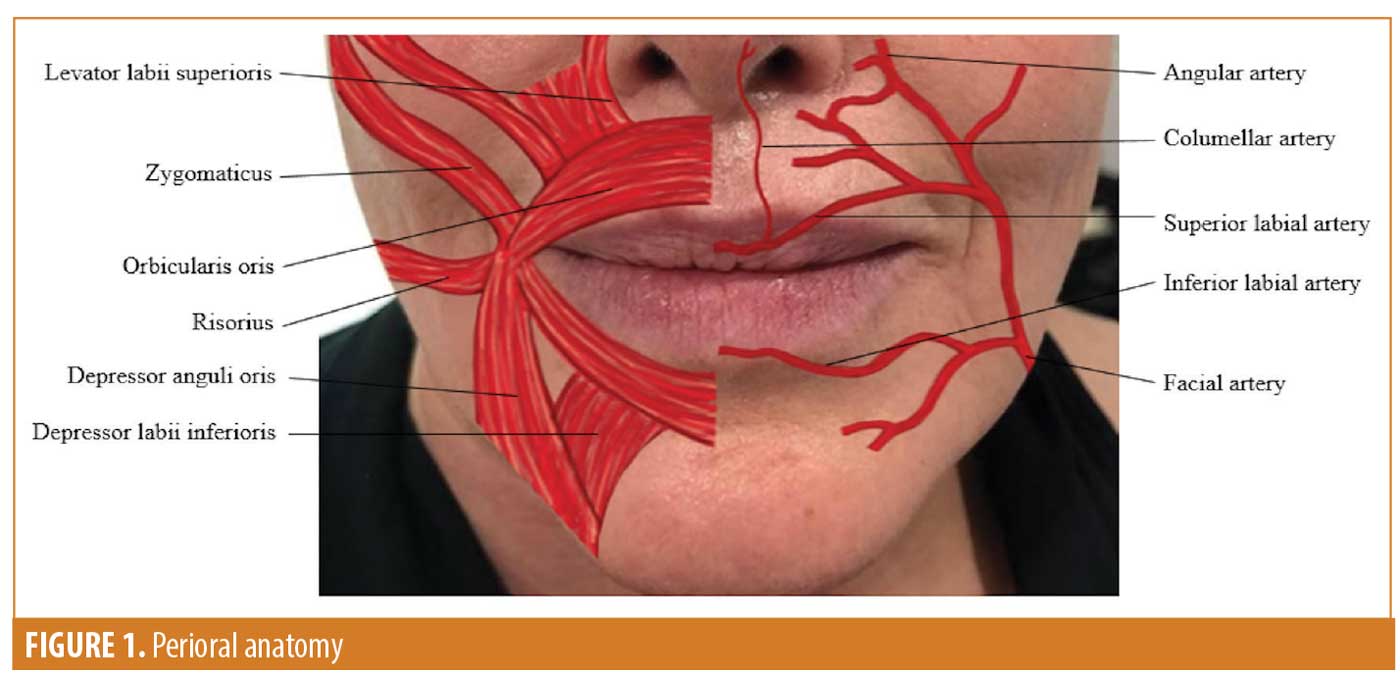
The perioral region is bound superiorly by the base of the nose, superolaterally by the nasolabial folds, inferiorly by the labiomental crease, and inferolaterally by the labiomandibular folds.4 The mandible, maxillary bones, and teeth are the bony structures that support and shape this area.5 The perioral muscles are composed of the orbicularis oris, levator labii superioris, levator anguli oris, zygomaticus, risorius, depressor anguli oris, depressor labii inferioris, and mentalis.5 Sensory innervation of the perioral region is provided by the maxillary (V2) and mandibular (V3) divisions of the trigeminal nerve. The upper lip is innervated by the superior labial and superior alveolar nerves from the infraorbital branches of the maxillary nerve. The lower lip and chin are innervated by the inferior alveolar nerve and mental nerve, which arise from the mandibular nerve.5 Perioral blood supply comes from the facial artery, which branches into the submental artery, inferior and superior labial arteries, and angular artery (Figure 1).6
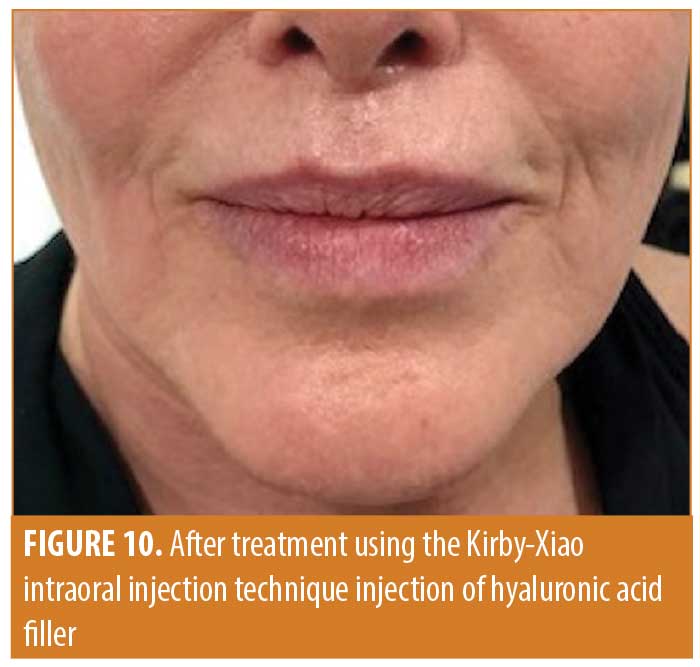
Anatomical landmarks in the perioral region include the philtrum and philtral columns, Cupid’s bow, vermillion border, oral commissures, nasolabial folds, labiomental crease, and labiomandibular folds. Perioral aesthetic concerns often involve one or more of these landmarks. Prominent radial wrinkling around the lips, downturned oral commissures, exaggerated depth of the nasolabial, labiomental, or labiomandibular folds, and flattening of the Cupid’s bow are common complaints described by patients seeking aesthetic rejuvenation (Figure 2).

Current Techniques for Hyaluronic Acid Perioral Rejuvenation
Common techniques for the injection of HA acid filler in the perioral region include retrograde or anterograde linear threading, fanning, cross-hatching, and depot, using a percutaneous approach.7 Perioral radial fine lines are generally treated by retrograde linear threading along the vermillion border, followed by direct placement of filler in the vertical rhytids. A fanning or cross-hatching technique may be used for deeply etched lines.8,9 The oral commissures are typically improved by anterograde threading from a cutaneous insertion point inferior to each commissure.9 Some injectors favor an X-shaped linear thread or aliquot depot injection placed just below each commissure to produce an upward lift.8 This is usually performed in conjunction with treatment of the labiomandibular folds with a linear threading or fanning injection in the deep dermal or subcutaneous planes.8 Nasolabial folds can be treated by a subdermal injection with fanning technique across the fold. A deep mental crease can be softened by linear threading of HA acid into the subcutaneous plane.8 Potential injection site reactions following cosmetic injections include swelling, tenderness, bruising, and pain, which are common sequelae in all HA acid filler injections.
The Kirby-Xiao Intraoral (KXIO) Injection Technique: A Novel Technique for Perioral Enhancement
The KXIO injection technique is a novel intraoral approach to HA acid filler injections to improve overall perioral cosmesis. This technique was developed by Dr. William Kirby and inspired by multiple patients who reported an improvement in their perioral aesthetics while wearing dental retainers. As such, this technique is designed to place HA acid filler intraorally in the same areas that would be volumized by dental retainers. Previous intraoral injection techniques have been described for the correction of volume deficiencies in the midface, with placement of filler in the deep subcutaneous and supraperiosteal planes to restore volume in the malar cheeks.10,11 We propose that the KXIO injection technique is a new application of the intraoral injection approach specifically designed for perioral aesthetic rejuvenation.
Implementation of the KXIO injection technique.

- Review informed consent with the patient and discuss the potential side effects of any HA filler injections, including swelling, tenderness, bruising, erythema, nodules, and vascular compromise. Inform patient that the KXIO injection technique is off-label.
- Have hyaluronidase, nitroglycerine paste, and aspirin available in case of suspected vascular compromise.
- Provide the patient with a mirror and review their perioral anatomy to discuss goals and realistic expectations. Assess the extent of perioral lines, folds, and shadows to customize treatment to each patient.
- Determine which HA filler with low elasticity and low viscosity will be used for enhancement.
- Intraoral topical anesthetics are not routinely used for this technique since patients have reported that intraoral injections are less painful than traditional percutaneous perioral injections. If desired, benzocaine 20% gel can be used to decrease patient discomfort.
- Cleanse the oral cavity with a chlorhexidine-based mouthwash to minimize infection risk.
- Use the nondominant hand to manually evert the patient’s lower lip to expose the interior mucosal side of the lip (Figure 3).

- With the dominant hand, inject approximately 0.1cc of filler in four evenly spaced depot aliquots in the lower mucosal lip, for a total of 0.4cc of filler. The size of the aliquots and total amount injected can be adjusted according the specific deficits of each patient (Figures 4 and 5).


- Repeat the same technique on the upper lip; use the nondominant hand to manually evert the patient’s upper lip to expose the interior mucosal side of the lip (Figure 6).

- With the dominant hand, inject approximately 0.1cc of filler in four, evenly spaced depot aliquots for a total of 0.4cc of filler in the upper lip. The size of the aliquots can be tailored to the specific deficits of each patient (Figures 7 and 8).

- The appropriate placement of filler is dependent on the patient’s individual anatomy and perioral deficits. The authors suggest using the following anatomical landmarks to guide placement of the aliquots: The aliquots in the lower lip should be placed approximately halfway down the vertical length of the inferior mucosal lip, with each aliquot directly opposing one of the four mandibular incisors. The aliquots in the upper lip should be placed approximately halfway up the vertical length of the superior mucosal lip, with each aliquot directly opposing one of the four maxillary incisors. The depth of the injections is approximately 3mm.
- To minimize the risk of vascular compromise, we propose the following safety considerations: Avoid injecting in the submucosal plane near the vermilion-mucosa junction in the upper lip to minimize the risk of injury to the superior labial arteries. Tansatit et al12 described the typical position of the superior labial artery along the upper lip between the oral mucosa and the orbicularis oris muscle just above the vermilion-mucosa junction. As such, intraoral filler injections in the upper lip should be placed at an adequate distance from the vermilion-mucosa junction, as described above, to reduce the risk of intravascular injury to the superior labial arteries. Injections in the lower lip have minimal risk of intravascular injury due to the minute size of the ascending arteries.12 As with all aesthetic injections, the intravascular injection risk can be minimized with precise needle placement and very slow injection.9
- Aluminum chloride 20% solution can be applied to injection areas to minimize postinjection bleeding and subsequent bruising.
- Manually massage the injected areas by pinching the upper and lower lips with the index fingers located intraorally and thumbs placed on the external cutaneous lip. Apply gentle to moderate pressure to smooth out superficial lumps and contour irregularities.
- Cool compresses or ice packs can be used to minimize postprocedural swelling.


Conclusion
The importance of the perioral region in overall facial aesthetics is demonstrated by the high volume of patients seeking perioral rejuvenation. While it is well established that perioral aesthetic concerns can be treated with existing superficial filler injection techniques, the KXIO technique facilitates more precise placement of filler with less discomfort, leading to high patient satisfaction coupled with minimal and predictable side effects. The KXIO technique can be customized to each patient to effectively correct volume deficiencies and enhance perioral aesthetics to maintain a youthful appearance. Because the KXIO technique can be more technically challenging for novice injectors, a thorough understanding of the relevant anatomical features, proper patient selection, and realistic patient expectations, and a precise evaluation of a patient’s personal corrective needs are paramount for optimal outcomes.
Acknowledgments
The authors would like to thank William “Cash” Kirby, a fourth grader at Center Street School in El Segundo, California, for his contribution in inspiring this technique through a series of questions about lip augmentation.
References
- Ibrahim O, Berson DS, Rohrer TE. Trends in Dermatologic Surgery: Results of the American Society for Dermatologic Surgery Procedure and Consumer Surveys. Dermatol Surg. 2019;45(2):303–306.
- Tierney EP, Hanke CW. Recent trends in cosmetic and surgical procedure volumes in dermatologic surgery. Dermatol Surg. 2009;35(9):1324–1333.
- Kim S, Kim M. Trends of noninvasive radiofrequency and minimally invasive treatment for the management of facial aging. J Chem Dermatol Sci Appl. 2019;9(1):30.
- Ponsky D, Guyuron B. Comprehensive surgical aesthetic enhancement and rejuvenation of the perioral region. Aesthet Surg J. 2011;31(4): 382–391.
- Wollina U. Perioral rejuvenation: restoration of attractiveness in aging females by minimally invasive procedures. Clin Interv Aging. 2013;8:1149.
- Pinar YA, Bilge O, Govsa F. Anatomic study of the blood supply of perioral region. Clin Anat. 2005;18(5):330–339.
- Klein AW. Techniques for soft tissue augmentation. Am J Clin Dermatol. 2006;7(2):107–120.
- Buckingham ED, Glasgold R, Kontis T, et al. Volume rejuvenation of the lower third, perioral, and jawline. Facial Plast Surg. 2015;31(1):70–79.
- Chiu A, Fabi S, Dayan S, Nogueira A. Lip injection techniques using small-particle hyaluronic acid dermal filler. J Drugs Dermatol. 2016;15(9): 1076–1082.
- Dayan SH, Bassichis BA. Facial dermal fillers: selection of appropriate products and techniques. Aesthet Surg J. 2008;28(3):335–347.
- Anand CV. Intraoral approach: a newer technique for filler injection. J Cutan Aesthet Surg. 2010;3(1):23–24.
- Tansatit T, Apinuntrum P, Phetudom T. A typical pattern of the labial arteries with implication for lip augmentation with injectable fillers. Aesthetic Plast Surg. 2014;38(6):1083–1089.
- Sito G. Transoral injection of Restylane SubQ for aesthetic contouring of the cheeks. Aesthet Surg J. 2006;26(1S):S22–S27.