J Clin Aesthet Dermatol. 2024;17(1):13–14.
J Clin Aesthet Dermatol. 2024;17(1):13–14.
by Jay Patel, MD; Danielle Morin; BS, Ted Rosen, MD; Carina Wasko, MD; Leah Douglas, MD
Drs. Patel, Rosen, Wasko, and Douglas are with the Department of Dermatology, Baylor College of Medicine in Houston, Texas. Ms. Morin is with the Baylor College of Medicine in Houston, Texas.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors have no conflicts of interest relevant to the contents of this article.
ABSTRACT: Kaposi sarcoma can have a myriad cutaneous presentation, but an underrecognized one is an initial manifestation of simply edema. Herein, we highlight a series of cases where edema was the presenting feature of Kaposi Sarcoma and emphasize the importance of recognizing this finding as a possible sign of KS. Keywords: Kaposi Sarcoma, HIV, edema
Kaposi sarcoma (KS), when related to those individuals with human immunodeficiency virus (HIV), is considered an Acquired Immunodeficiency Syndrome (AIDS)-defining illness.1 Lesions may appear in varying colors, such as purpuric, violaceous, and erythematous, and can have protean morphologic appearances, ranging from macules to plaques to nodules.2 However, KS initially manifesting as non-specific edema-like swelling is unusual and, thus, not reported widely in the literature. This series is unique, highlighting an important and easily overlooked morphologic presentation. Recognizing localized edema-like swelling as a distinct form of KS, therefore, increases the likelihood of early diagnosis and prompt therapeutic intervention, possibly preventing disease progression.
Report of cases
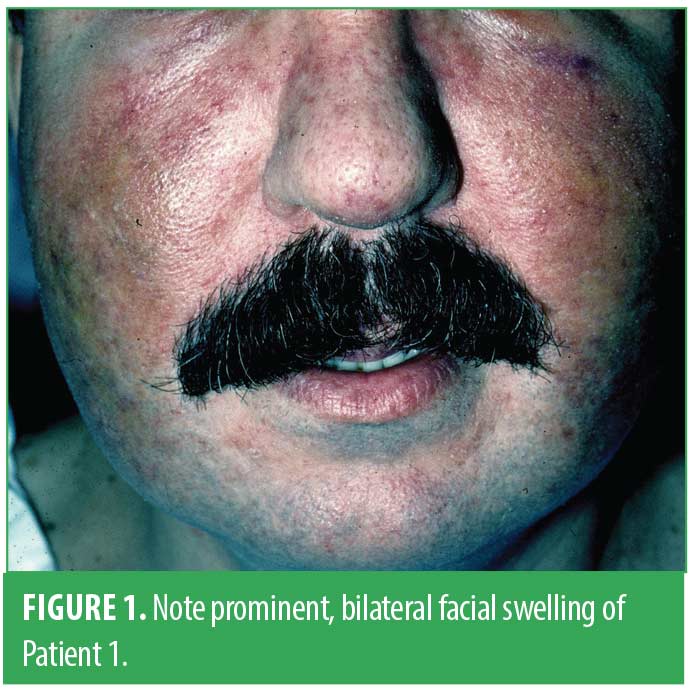
Case 1. A 33-year-old gay male presented to the emergency department with a chief complaint of facial swelling associated with mild erythema. He was sent for dermatologic consultation with a provisional diagnosis of rosacea. Physical examination disclosed indurated swelling of both nasolabial folds and the left cheek (Figure 1). There was some mild superficial erythema, but neither papules nor pustules were noted. A punch biopsy taken through the right nasolabial fold revealed histologic features classic for KS; subsequent lab studies disclosed a positive HIV test, a Cluster of differentiation 4 (CD4) count of 225 cells/mm3, and a viral load of 25,000 copies/mL. The patient was started on antiretroviral therapy with improved facial swelling.
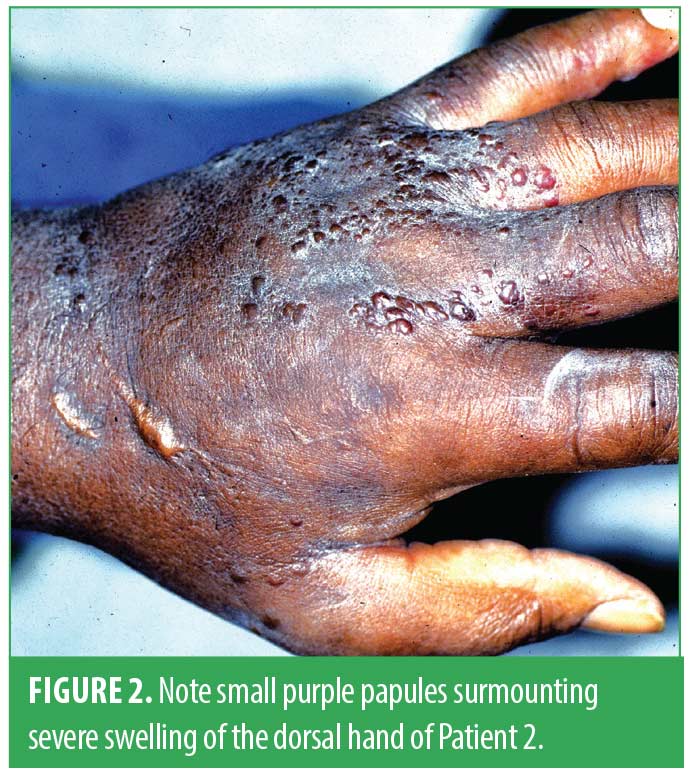
Case 2. A 43-year-old female with a history of intravenous drug use presented with the gradual onset of indurated swelling of the left hand, making digital movements difficult. Eventually, multiple small brown to purple papules surmounted the swollen dorsal hand and adjacent fingers (Figure 2). Biopsies of both the papular lesions and the diffuse swelling of the hand disclosed classic histologic findings of KS. She was found to be HIV positive and had a CD4 count of 200 copies/mm and a viral load of 53,670 copies/mL. Antiretroviral therapy was instituted, but the patient was lost to follow-up.
Case 3. A 36-year-old male with known HIV on highly active antiretroviral therapy previously complicated by KS of the upper extremities, for which he had received intralesional chemotherapy 18 years prior, presented several months previously at an outside hospital due to painful right lower extremity swelling. He developed an ulcer on the ipsilateral plantar foot that was subsequently debrided due to concern for infectious etiology. The patient was initially lost to follow-up but presented again several months later due to the progression of the lesion with worsening pain, erythema, and malodorous drainage of the affected foot. Lab results showed a CD4 of 257 cells/mm3 with a viral load of 1,010 copies/mL. Physical examination now demonstrated significant right lower extremity edema, a destructive gangrenous ulcer of most of the right plantar foot, and numerous violaceous papules over the dorsal and plantar foot surfaces (Figures 3 and 4). Magnetic resonance imaging (MRI) showed concern for osteomyelitis. A right below-knee amputation was performed, and tissue pathology of the foot was positive for KS with positive human herpes virus-8 (HHV-8) staining. The patient was subsequently lost to follow-up. The characteristics of these patients are summarized in Table 1.
Discussion
KS is a tumor that can be encountered in both immunocompromised or immunocompetent settings with five clinical subtypes currently known: classic KS, endemic KS, iatrogenic KS, AIDS-KS, and, discovered in 2019, HIV-negative men who have sex with men KS.1 As was true in all our cases, KS accompanied the diagnosis of HIV infection, as immunosuppression enables infection by HHV-8 and results in the vast majority of clinical KS cases.3 It is noteworthy also that our three patients showed decreased CD4 counts, which remained above 200 cells/mm3. This finding is somewhat atypical in that KS usually appears when the CD4 count falls below 150 cells/mm3.4
Conclusion
Upon reviewing the literature, we could not identify reported cases of KS initially manifesting as diffuse cutaneous edema-like swelling. This series of cases highlights that the localized edematous appearance of varying body parts in a patient with known or suspected HIV infection should raise suspicion for the possibility of underlying KS. Early recognition of “edema” actually being due to tissue infiltration with KS might facilitate early biopsy, proper diagnosis, and timely institution of antiretroviral therapy. Case 3 also vividly illustrates how delay can lead to a worsening of the clinical situation. It is thus of paramount importance to start patients with AIDS-related KS on antiretroviral therapy, as this may result in the resolution of cutaneous lesions. Widespread forms of KS impacting viscera may necessitate systemic chemotherapy such as taxanes or liposomal daunorubicin.1
References
- Dupin N. Update on oncogenesis and therapy for Kaposi sarcoma. Curr Opin Oncol. 2020. 32(2):122-128.
- Wang J, et al. An unusual series of patients with Kaposi sarcoma. JAAD Case Reports. 2019. 5(8):646-649.
- Gao SJ et al. Seroconversion to antibodies against Kaposi’s sarcoma-associated herpesvirus-related latent nuclear antigens before the development of Kaposi’s sarcoma. N Engl J Med. 1996. 335(4):233-241.
- Maurer T, M Ponte, Leslie K. HIV-associated Kaposi’s sarcoma with a high CD4 count and a low viral load. N Engl J Med. 2007. 357(13):1352-1353.