J Clin Aesthet Dermatol. 2024;17(2):24–28.
J Clin Aesthet Dermatol. 2024;17(2):24–28.
by Sheila C. Barbarino, MD, FACS; Doris Day, MD; Alexander Rivkin, MD; Jennifer Levine, MD; and John Fezza, MD
Dr. Barbarino is with Barbarino Surgical Arts in Austin, Texas. Dr. Day is with NYU Langone Health in New York, New York. Dr. Rivkin is with the David Geffen School of Medicine at UCLA in Los Angeles, California. Dr. Levine is with Lenox Hill Hospital and Manhattan Eye, Ear, and Throat Hospital in New York, New York. Dr. Fezza is with the Center for Sight in Sarasota, Florida.
FUNDING: Funding for this study was provided by Merz.
DISCLOSURES: Dr. Barbarino is owner/principal surgeon for Barbarino Surgical Arts in Austin, Texas, and Redondo Beach, California. She is a consultant, advisor and speaker for Merz, Galderma, Suneva and Upneeq, and a principal investigator for Merz. Dr. Day is a consultant and advisor for Allergan/Abbvie, Revance Therapeutics, and Galderma. Dr. Rivkin is a consultant, advisor and speaker for Allergan, Galderma, Merz, Suneva and Upneeq, and a principal investigator for Allergan, Galderma, and Merz. Dr. Levine is a consultant and speaker for Allergan and BTL, a consultant and advisor for Galderma and Merz, and a speaker for RVL. Dr. Fezza is a consultant for Allergan and Revance Therapeutics, and a speaker and advisor for Revance Therapeutics and Upneeq.
ABSTRACT: Background. Microgenia resulting from congenital deficiency or aging can significantly affect the facial profile and render it less attractive. This study assessed the effectiveness of treatment with incobotulinumtoxinA (Inco) and calcium hydroxylapatite with integral lidocaine (CaHA[+]) for improving chin profile.
Methods. Subjects with a hyperactive mentalis and at least moderate chin retrusion according to the Asian Chin Projection Scale (ACPS) were recruited. At Visit 1, subjects received Inco injection into the mentalis, followed by deep, pre-periosteal injections of CaHA(+) into the pogonion. The primary endpoint was an ACPS improvement of one point at one and six months. Photographs at baseline and each follow-up visit were rated by physicians using the Global Aesthetic Improvement Scale (GAIS). All subjects completed a satisfaction questionnaire.
Results. Ten female subjects were recruited. Mean age was 42.5 years and all had moderate-to-severe chin retrusion at baseline (ACPS score ≥2). All subjects demonstrated at least a one-point improvement in ACPS compared with baseline at both the one-month and six-month posttreatment visits. Physician GAIS ratings of subject appearance confirmed that 100 percent of subjects experienced improved chin projection at each follow-up visit compared to baseline. All 10 subjects were pleased with their chin profile after treatment, with 90 percent noting that it was still “very much improved” at six months.
Conclusion. Based on our results, combined treatment with CaHA and Inco appears to be effective and well tolerated for improving the facial profile of subjects with chin retrusion. Treatment was associated with a high degree of patient satisfaction and was well tolerated.
Keywords: Calcium hydroxylapatite, chin augmentation, incobotulinumtoxinA, microgenia, mentalis
In both men and women, the chin is a major contributor to lower facial features, providing definition to the jawline and enhancing the facial profile. The ideal chin profile is conventionally considered to be one that extends to 1mm to 3mm behind a vertical line descending from the vermilion border of the lower lip.1 A receding chin has a profile falling posterior to this, and the inadequate projection can create a sense of facial imbalance. Chin retrusion, also known as microgenia, meaning “small chin,” may be congenital or occur as a result of bone and tissue loss due to aging. A retruded chin can have a significant impact on an individual’s facial appearance, such as making an average sized nose appear too large and creating a weak jawline.
The aesthetic importance of the chin has made chin implant surgery or osseous genioplasty popular aesthetic procedures. In the United States alone, an estimated 43,900 surgical chin augmentations were performed in 2020.2 Overall, such procedures are safe and effective, and complications are rare, but regardless of the technique, all surgery carries an inherent risk for complications.3 Chin implants are the most common form of chin augmentation but are also a more frequent source of complications, including infections, extrusions, and bone erosion.3 Some chin implants may also lead to unwanted imperfections, including accentuation of the prejowl sulcus, either because they lack lateral extension or because of implant-associated bone erosion combined with aging-associated mandibular bone resorption, soft tissue descent, and skin laxity.4
In recent years, dermal fillers have provided an alternative, less invasive option for enhancing the volume of the chin and creating a stronger jawline and facial profile. They provide a nonsurgical, temporary method of correcting moderate chin deformities with minimal downtime. Calcium hydroxylapatite (CaHA; Radiesse®; Merz North America, Raleigh, North Carolina), in particular, has been extensively studied for jawline rejuvenation including the chin, with or without integral lidocaine.5−10 CaHA has a higher G’ and viscosity than commercially available hyaluronic acid (HA) fillers; properties that allow it to resist forces exerted by overlying facial muscles, and to provide structural support.11 When placed in the supraperiosteal plane of the chin, the high G’ and viscosity are focused upon lifting and expanding the overlying tissues.12 A further advantage is its ability to offer continued stimulation of collagen Type I, Type III, and elastin deposition around the microspheres, providing long-lasting treatment results.13
In addition to underlying bony anatomy, a hyperactive mentalis muscle can also contribute to a receding chin. Botulinum neurotoxin injections into the mentalis can relax the muscle tissue, creating a fuller appearance.14,15 The combined actions of CaHA with botulinum neurotoxin to improve chin profile have not previously been studied. In the present study, the authors investigated the effects of CaHA with 0.3% integral lidocaine (CaHA(+); Radiesse® (+), Merz North America, Inc, Raleigh, North Carolina) and incobotulinumtoxinA (Inco; Xeomin®, Merz Pharmaceuticals GmbH, Frankfurt am Main, Germany) injected in the same treatment session to improve the profile of subjects with a hyperactive mentalis and moderate to severe chin retrusion.
Methods
Study design. This multi-site, single-injector study, conducted at a private facial and cosmetic plastic surgery practice, recruited male and female subjects aged 22 to 70 years old with at least moderate chin retrusion according to the Asian Chin Projection Scale (ACPS; 0=full chin projection, 1=mild chin retrusion, 2=moderate retrusion, 3=severe retrusion, and 4=very severe chin retrusion).16 In addition to an under-projected bony chin, patients were required to have a pronounced cobblestone appearance to their chin upon mentalis muscle activation. Subjects were not eligible for treatment if they had undergone dermal filler, toxin, device or other treatment to the lower face in the last two years, or had current active local or systemic disease, or excessive scarring in the area of treatment. Pregnant or breastfeeding women or those planning a pregnancy were also excluded. All participants were required to show willingness and ability to adhere to protocol requirements, including returning for follow-up visits and abstaining from any other procedures in the treated area throughout the study. All subjects provided signed, informed consent to the procedures and to the subsequent use of identifiable photographs for scientific purposes. The study was approved by a centralized institutional review board (Advarra, Columbia, Maryland) and adhered to the tenets of the Declaration of Helsinki as amended in 2008 and was compliant with the Health Insurance Portability and Accountability Act (HIPAA) which ensures protection of individually identifiable health information, unless consented by the patient.
The study comprised four visits over a six-month period with the same physician performing all treatments to ensure consistency of technique. At Visit 1, patients were screened and those meeting the inclusion criteria had topical anesthesia applied in the form of a betacaine, 20%/lidocaine, 10%/tetracaine, 10% cream and ice prior to receiving a maximum of 10U of Inco, reconstituted using 2.5mL of bacteriostatic NaCl, into the mentalis muscle. This was followed at the same visit by deep, pre-periosteal injections of CaHA(+), injected using a 27-gauge needle as multiple boluses into the pogonion, with an insertion point where the highest degree of projection was intended. A maximum of two syringes (3mL) was used. After the injection, ice was applied to minimize bruising.
The objective was to correct each subject to either full chin projection (Grade 0) or mild chin retrusion (Grade 1) according to the ACPS scale. Follow-up visits took place at one, four and six months after treatment. At the four-month posttreatment visit, subjects received re-treatment with the same amount of Inco as at the initial visit. At each posttreatment visit, the treating investigator and four blinded evaluators completed the ACPS. All subjects also rated their appearance using GAIS and completed a patient satisfaction survey at six months. Standardized profile-view photographic images were taken by the treating investigator at each visit. In addition, the treating investigator and the four blinded evaluators, all of whom were facial plastic surgeons, evaluated each patient’s before and after photos and assessed improvement using a five category Global Aesthetic Improvement Scale (GAIS; very much improved, much improved, improved, no change, worse).
The primary outcome was an improvement of one point in sagittal chin projection on the ACPS as evaluated by the primary investigator at one and six months. Secondary outcomes were blinded evaluator GAIS rating of aesthetic improvement and patient satisfaction.
Results
The study enrolled 10 female subjects ranging in age from 22 to 70 years old (mean age 42.5 years old). At baseline, four subjects had moderate chin retrusion (ACPS Grade 2), five subjects had severe chin retrusion (ACPS Grade 3), and one subject had very severe retrusion (ACPS Grade 4). All subjects attended all visits. The number of Inco units injected ranged from 5 to 10 (the same unit range was injected at the four-month touch-up if required; four subjects did not receive a four-month touch-up), and the volume of CaHA injected per patient was 1.5 to 3.0mL.
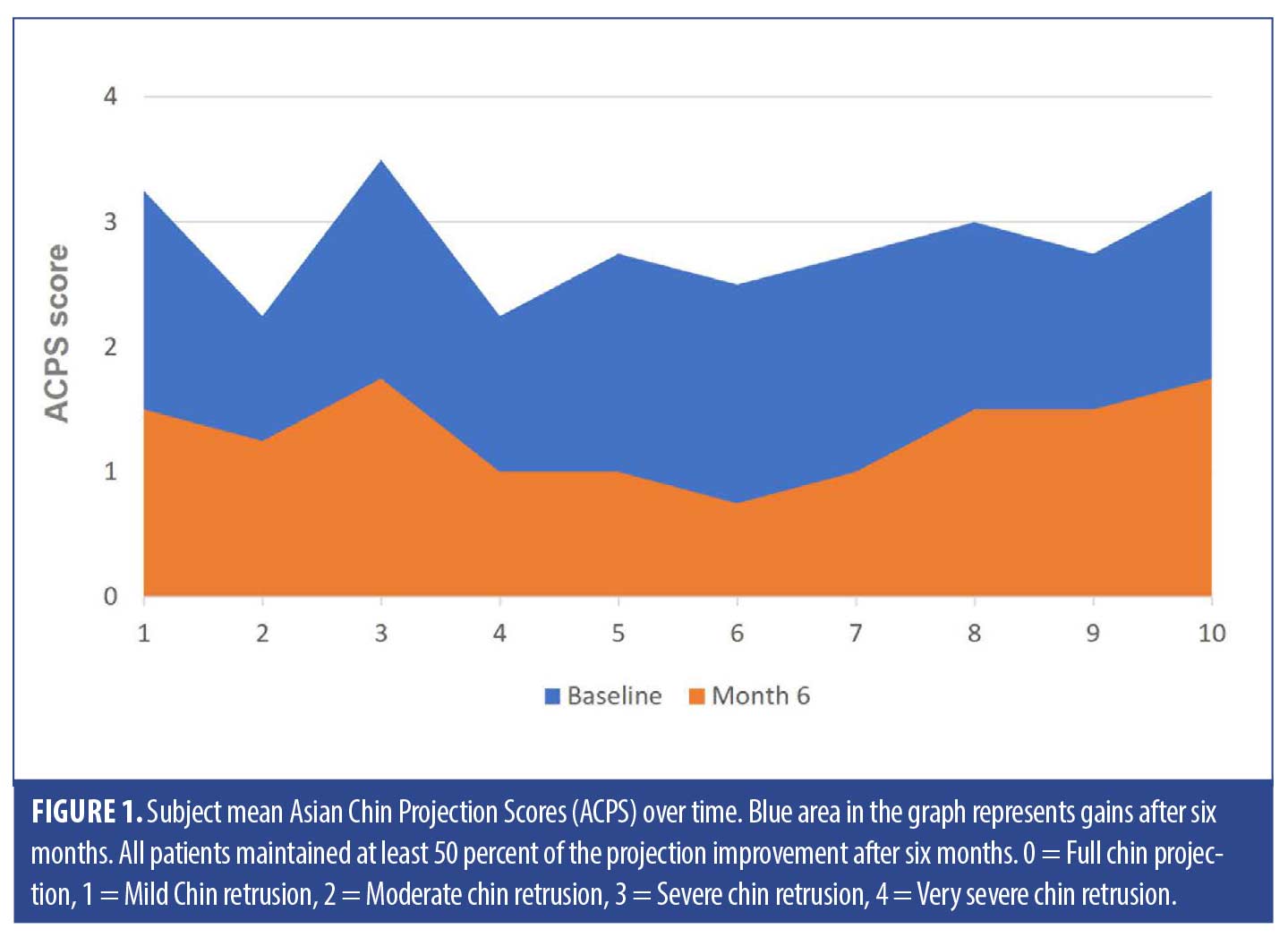
ACPS improvement in sagittal chin projection. All subjects demonstrated and maintained at minimum a one-point improvement in ACPS at six months compared with baseline (Table 1). Mean blinded evaluator ACPS score was 1 at each posttreatment visit compared with 3 at baseline, demonstrating a lasting two-point improvement in chin projection. In all patients, improvements in chin protrusion compared with baseline were maintained to the end of the study (Figure 1).
Physician GAIS ratings. Physician ratings of subject appearance according to GAIS confirmed that 100 percent of subjects experienced improved chin projection at each follow-up visit compared with baseline (Figure 2). At six months, ratings of some patients’ level of improvement had changed from “very much improved” to “much improved” or “improved”. However, all patients maintained a level of improvement in chin projection throughout the study, indicating that the treatments were effective for at least six months and possibly longer.
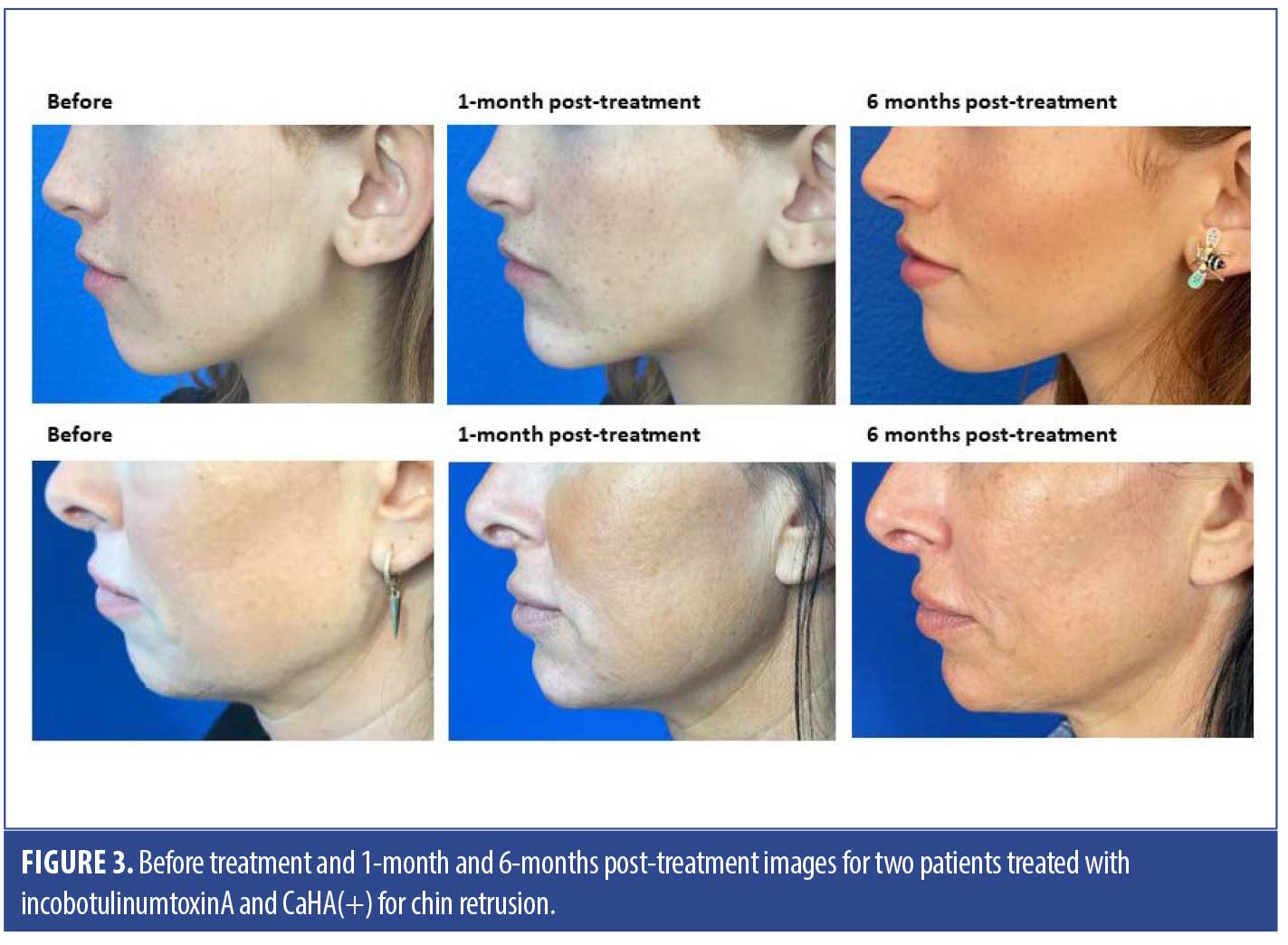
Subject satisfaction rating. Before and after images for two patients treated with Inco and CaHA(+) are shown in Figure 3. All 10 subjects were pleased with their chin profile after treatment with 90 percent noting that it was “very much improved” at six months. Furthermore, 90 percent of subjects indicated that they would pursue further similar treatments in the future (one subject somewhat agreed with this statement). All subjects stated they would recommend the treatment to others considering improving their chin profile.
Adverse events. No treatment complications were observed after either Inco or CaHA(+) injection. When asked what they found to be “the worst part of the treatment”, 40 percent of subjects noted nothing, while 60 percent noted bruising; one subject mentioned bruising was accompanied by an initial “tightness.”
Discussion
Chin shape plays an essential role in overall facial attractiveness in both men and women.17,18 This study met the primary endpoint of treating subjects with CaHA(+) and Inco to full chin projection or mild chin retrusion at the assessment visits at one, four, and six months. This was despite all subjects having at least moderate chin retrusion at baseline.
Physician GAIS ratings of subject appearance confirmed the effectiveness of CaHA(+) and Inco for improving chin projection, with all subjects maintaining an improved profile compared with baseline through to the end of the study.
Inco and CaHA(+) treatment were associated with very high levels of patient satisfaction. All subjects continued to note improvement at six months, and 90 percent noted that their profile continued to be “very much improved.” Further evidence of their satisfaction was implied by the fact that 90 percent would repeat similar treatments, and all would recommend the treatment to others. In the current study, CaHA(+) and Inco were very well tolerated; injection-related bruising was the main side effect, observed in 40 percent of subjects.
A retruded chin that slopes back towards the neck creates a weak jawline and is subconsciously perceived as a sign of a weak personality and social submissiveness.19 In men, a weak chin and jawline convey a lack of strength and masculinity, while in women the lack of definition between the jawline and neck can age the face and create the appearance of an overly prominent nose. Chin profile can influence an individual’s self-esteem and psychosocial well-being, and studies of chin shape have shown that chin projection is related to high scores of self-perceived attractiveness.20
The data from this proof-of-concept study compare well with those from a recent trial of HA filler injection for chin augmentation. Similar to the current study, participants were aged 22 years or older with moderate or severe chin retrusion and received a median total initial injection volume of 2.2mL (range, 0.7–4.0mL).21 Responder rate (≥1-point improvement on a five-point photo-numeric chin rating scale) was only 56 percent at six months, whereas in the current study all subjects demonstrated at least a one-point improvement in the ACPS at this time point.
A retrospective review of 345 cases of chin microgenia treated with either surgical sliding genioplasty, alloplastic implants, or HA filler injection, found that HA filler was effective for all but the most severe cases, albeit with the requirement for repeat injections.22 Minimally-invasive chin augmentation with dermal fillers has become increasingly popular in recent years, as evident from a review of the published literature.10,21,23−26 However, this is the first study to publish data for a combined approach to chin augmentation using both a filler (CaHA[+]) and botulinum neurotoxin (Inco). The two treatments complement each other in that Inco relaxes the hyperactive mentalis fibers thereby altering the position of the pogonion and improving chin contour,15 while CaHA(+) augments the chin and stimulates collagen synthesis to further enhance chin profile.10
Our findings complement those of a previous study with CaHA(+) alone for chin augmentation, which also reported high rates of satisfaction and persistent results at six months with no reported complications.10 The high G prime of CaHA provide it with greater lifting capacity than HA fillers,27 but at the same time allows it to be molded and sculpted into shape. In addition, CaHA provides long-term stimulation of the patient’s own collagen production13 leading to a longer duration of effect. CaHA(+) is also the only U.S. Food and Drug Administration (FDA)-approved injectable treatment for jawline contour improvement, including the chin.
Alternative treatments for chin enhancement include alloplastic implants and surgical genioplasty. While both are effective, surgical approaches can involve extensive dissection and are associated with other inherent complications including implant migration, scarring, infection, bone resorption, and mental nerve injury. Injectable treatments offer subtle enhancement with immediate results typically lasting 8 to 12 months,8 depending on the filler used. They are associated with minimal downtime and are a solution for patients wanting to experience a new chin profile without wanting to commit to a permanent change.
Limitations. This was a small study to assess effectiveness and subject satisfaction with a combination of CaHA(+) and Inco for chin augmentation. The study has several limitations, mainly related to the small number of subjects studied. Further research is now warranted to determine whether the results are replicated in men and other subject groups of different ethnicities. It will also be important to define the baseline level of chin retrusion severity most suited to this treatment, and the repeat treatment intervals required for optimal effect.
Conclusion
In this small case series, injection of CaHA(+) and Inco was effective at improving overall chin profile and was associated with high levels of patient satisfaction. Both subjects and evaluating physicians indicated aesthetic results at six months were still improved compared with baseline. A combination of CaHA(+) and Inco treatment for a mild to moderate chin retrusion offers an effective and minimally-invasive alternative to surgical procedures.
References
- Fanous N, Yoskovitch A. Estimating implant size in chin augmentation: A simplified approach. Can J Plast Surg. 2003 Fall;11(3):161–165.
- American Society of Plastic Surgeons. Plastic Surgery Statistics Report 2020. https://www.plasticsurgery.org/documents/News/Statistics/2020/plastic-surgery-statistics-full-report-2020.pdf.
- White JB, Dufresne CR. Management and avoidance of complications in chin augmentation. Aesthet Surg J. 2011;31(6):634–642.
- Yeung AWK, Wong NSM. Mandibular bone resorption following chin augmentation: a systematic review. Front Surg. 2022;9:815106.
- Baspeyras M, Dallara JM, Cartier H, et al. Restoring jawline contour with calcium hydroxylapatite: A prospective, observational study. J Cosmet Dermatol. 2017;16(3):342–347.
- Dallara JM, Baspeyras M, Bui P, et al. Calcium hydroxylapatite for jawline rejuvenation: consensus recommendations. J Cosmet Dermatol. 2014;13(1):3–14.
- Van Loghem JV, Yutskovskaya YA, Philip Werschler W. Calcium hydroxylapatite: over a decade of clinical experience. J Clin Aesthet Dermatol. 2015;8(1):38–49.
- Juhász MLW, Marmur ES. Examining the efficacy of calcium hydroxylapatite filler with integral lidocaine in correcting volume loss of the jawline – a pilot study. Dermatol Surg. 2018;44(8):1084–1093.
- Moradi A, Shirazi A, David R. Nonsurgical chin and jawline augmentation using calcium hydroxylapatite and hyaluronic acid fillers. Facial Plast Surg. 2019;35(2):140–148.
- Hartstein M, Fezza J. Chin augmentation and reshaping: using calcium hydroxylapatite with lidocaine filler. Am J Cosmetic Surg. 2020;10: 1–7.
- Lorenc ZP, Bass LM, Fitzgerald R, et al. Physiochemical characteristics of calcium hydroxylapatite (CaHA). Aesthet Surg J. 2018 Apr 6;38(suppl_1):S8–S12.
- Lorenc ZP, Lee JC. Composite volumization of the aging face: supra-periosteal space as the foundation for optimal facial rejuvenation. J Drugs Dermatol. 2016;15(9):1136–1141.
- Yutskovskaya Y, Kogan E, Leshunov E. A randomized, split-face, histomorphologic study comparing a volumetric calcium hydroxylapatite and a hyaluronic acid-based dermal filler. J Drugs Dermatol. 2014;13(9):1047–1052.
- Papel ID, Capone RB. Botulinum toxin A for mentalis muscle dysfunction. Arch Facial Plast Surg. 2001;3(4):26826–26829.
- Hsu AK, Frankel AS. Modification of chin projection and aesthetics with onabotulinumtoxinA injection. JAMA Facial Plast Surg. 2017;19(6):522–527.
- Suwanchinda A, Seo K, Geister TL, et al. A validated assessment scale for Asian chin projection. Dermatol Surg. 2019;45 Suppl 1:S30–S37.
- Naini FB, Donaldson ANA, McDonald F, Cobourne MT. Assessing the influence of chin prominence on perceived attractiveness in the orthognathic patient, clinician and layperson. Int J Oral Maxillofacial Surg. 2012;41(7):839–846.
- Ren H, Chen X, Zhang Y. Correlation between facial attractiveness and facial components assessed by laypersons and orthodontists. J Dent Sci. 2021;16(1):431–436.
- Sinko K, Tran US, Wutzl A, et al. Perception of aesthetics and personality traits in orthognathic surgery patients: A comparison of still and moving images. PLoS One. 2018;13(5):e0196856.
- Kanavakis G, Halazonetis D, Katsaros C, et al. Facial shape affects self-perceived facial attractiveness. PLoS One. 2021;16(2):e0245557.
- Beer K, Kaufman-Janette J, Bank D, et al. Safe and effective chin augmentation with the hyaluronic acid injectable filler, VYC-20L. Dermatol Surg. 2021;47(1):80–85.
- Bertossi D, Galzignato PF, Albanese M, et al. Chin microgenia: a clinical comparative study. Aesthetic Plast Surg. 2015;39(5):651–658.
- Chen B, Ma L, Wang J. Chin augmentation with hyaluronic acid: an injection technique based on anatomical morphology. Dermatol Surg. 2022;48(7):747–751.
- Vanaman Wilson MJ, Jones IT, Butterwick K, et al. Role of nonsurgical chin augmentation in full face rejuvenation: a review and our experience. Dermatol Surg. 2018;44(7):985–993.
- Marcus K, Moradi A, Kaufman-Janette J, et al. A randomized trial to assess effectiveness and safety of a hyaluronic acid filler for chin augmentation and correction of chin retrusion. Plast Reconstr Surg. 2022;150(6):1240e–1248e.
- Sahan A, Karaosmanoglu N, Ozdemir Cetinkaya P. Chin augmentation with the use of cannula from a single, midline entry point: evaluation of 50 patients. J Cosmet Dermatol. 2020;19(6):1301–1306.
- Sundaram H, Voigts B, Beer K, et al. Comparison of the rheological properties of viscosity and elasticity in two categories of soft tissue fillers: calcium hydroxylapatite and hyaluronic acid. Dermatol Surg. 2010;36(Suppl 3):1859–1865.