J Clin Aesthet Dermatol. 2025;18(7–8 Suppl 1):10–15.
by Jodi Flynn, PA-C, DMSc, DFAAPA; Kathryn Harrison, DMSc, MMS, PA-C, CAQ-Dermatology; and Viet Le, DMSc PA-C, FACC, FAHA, HF-Cert
Dr. Flynn is with United Way Volunteer Care Clinic in Utah County, Utah, and Novartis Pharmaceuticals Company in East Hanover, New Jersey. Dr. Harrison is with Forefront Dermatology in Englewood, Colorado. Dr. Le is with Intermountain Medical Center Heart Institute in Salt Lake City, Utah.
Funding: No funding was provided for this article.
Disclosures: This publication was independently researched and written by Jodi Flynn in her personal capacity. The opinions and viewpoints expressed in this publication belong solely to the author and do not represent the position of her employer, Novartis Pharmaceuticals Corporation.
ABSTRACT: Hidradenitis suppurativa (HS) is a poorly recognized chronic skin condition that presents with inflamed recurring painful nodules, abscesses, and subcutaneous tunnels, mainly impacting intertriginous areas. Although extensively studied for its dermatological implications, recent research suggests a potential correlation between HS and cardiovascular disease. Studies reveal a heightened prevalence of cardiovascular risk factors, such as obesity, metabolic syndrome, and smoking, in individuals with HS. Most researchers attribute HS’s elevated cardiovascular risk to these coexisting factors. Objective: This review aims to identify whether or not HS’s underlying chronic inflammatory nature can contribute to atherosclerosis development, thereby elevating the risk of cardiovascular events and, specifically, major adverse cardiovascular events (MACE). Recognizing the association between HS and cardiovascular disease is crucial for comprehensive patient care. Methods: A PubMed search was performed to locate clinical trials, systematic reviews, and clinical reviews published to date concerning this topic. Results: This review consolidates existing literature on the topic, summarizing key findings and emphasizing the need for further research to clarify the mechanisms linking HS and cardiovascular conditions and delineating best clinical practices to mitigate risk. Limitations: Many publications attribute the increase in cardiovascular disease to comorbid risk factors. Despite limited research on cardiovascular (CV) risk in patients with HS, emerging evidence indicates an increased risk of adverse CV outcomes in this population, consistent with data from other chronic inflammatory diseases indicating that the inflammatory nature of the disease itself is elevating cardiovascular events. More clinical research is needed to strengthen this hypothesis and improve patient outcomes. Conclusion: An integrated, multidisciplinary approach combining dermatological and cardiovascular perspectives is vital for optimizing patient care and navigating the complexities of managing HS and its associated cardiovascular comorbidities. Keywords: Hidradenitis suppurativa, acne inversa, cardiovascular disease, risk factors, multidisciplinary, primary prevention, inflammatory dermatitis, systemic inflammation, major adverse cardiovascular events
Introduction
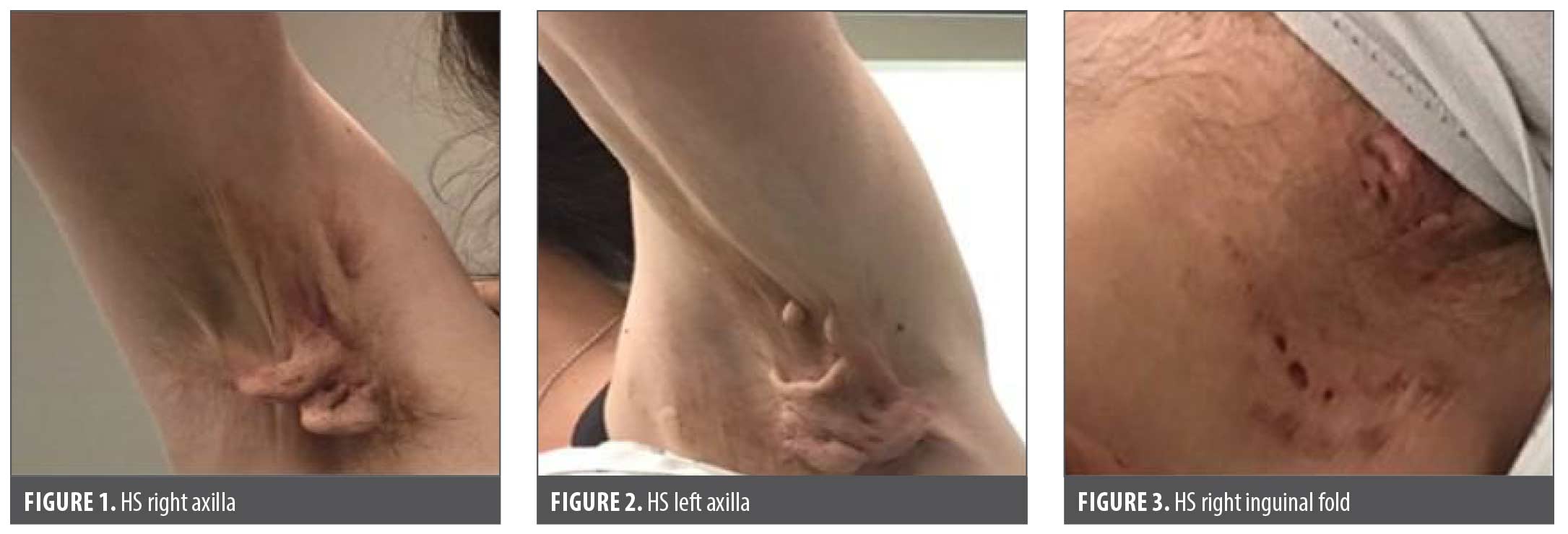
The inflammatory nature of hidradenitis suppurativa (HS) is revealed to be much deeper than the skin abscesses and scars that characterize this debilitating condition.1,2 HS, previously referred to as acne inversa, has historically been considered a rare disorder, but recent global population incidence and prevalence studies have shown otherwise.3 It is a skin condition characterized by flares of recurrent painful and deep abscesses, often progressing to subcutaneous tunnel formation in the intertriginous areas of the body, notably the groin, axillae, and anogenital region (Figures 1–3). While crucial topics such as etiology, pathogenesis, therapeutic options, and clinical management of HS are noteworthy, they fall outside the scope of this review. It’s important to acknowledge that these subjects have been thoroughly examined in recent publications by other authors.1,2,4,5
Historically, HS has been perceived as a rare ailment or, at the very least, as something that occurs infrequently. Healthcare professionals (HCPs) are often surprised to discover that the global estimated prevalence is between 1 to 4 percent, which is similar to the incidence of psoriasis. The true prevalence is likely higher due to frequent misidentification leading to up to a 10-year diagnostic delay.6 The presentation of HS varies depending on the disease stage, leading to frequent misdiagnosis and inadequate treatment. Research on clinical samples indicated a pooled prevalence of HS at 1.7 percent, and the overall estimates for HS prevalence align with rates observed in other inflammatory diseases. In Western societies, the prevalence of immune-mediated diseases typically falls within the range of 5 to 7 percent. Specifically, rheumatoid arthritis (RA) is at 0.5 to 1 percent in the United States (US) and Europe, while psoriasis has a prevalence of around 2 percent in North America (Table 1). The limited awareness of HS among the general public and HCPs contributes to the negative outcomes for those impacted.
HS is often acknowledged as one of the most painful dermatologic conditions.7,8 Yet many healthcare providers might not fully appreciate that HS might be a harbinger of deeper sequelae and consequences, resulting in not only debilitating skin lesions but also potentially debilitating and even life-threatening cardiac events.9 In many instances, dermatology HCPs play a pivotal role as primary healthcare professionals diagnosing HS, given that skin presentation frequently precedes the development of cardiovascular disease (CVD). Regrettably, a considerable number of patients with HS with CVD risks and subclinical CVD escape notice by dermatologists and primary care providers, resulting in the progression to active CVD without timely implementation of primary prevention strategies.3,10,11
CVD is the current leading cause of mortality in the US.12 Previous studies have identified that individuals with a history of RA and other inflammatory conditions are at increased risk of CVD. In a meta-analysis involving 15 studies, it was observed that the risk of myocardial ischemia was 60 percent greater in patients with RA compared to the general population.13 The relationship between HS and CVD is complex. Within the pathophysiology of HS, there’s an upregulation of various inflammatory immune cytokines and cells believed to contribute to the development of CVD. It is hypothesized that conventional cardiovascular risk assessment tools often fall short in accurately predicting the true cardiovascular risk in these patients.14,15 This phenomenon is well-documented in other chronic inflammatory conditions, such as psoriasis, inflammatory bowel disease (IBD), and RA.16–20
By gaining a more comprehensive understanding of the interplay between these immune-modulating factors and recognizing the elevated risk faced by patients with HS, healthcare providers can offer more effective primary prevention strategies to mitigate these CVD risks and enhance their overall well-being.
Methods
PubMed database was utilized for the initial search. A PubMed query yielded 153 results for HS and CVD. The search was first narrowed by filtering studies published since 2010, which produced 140 results and was further filtered for systematic reviews (47), randomized controlled trials (0), and meta-analyses (6), which produced a total of 53 results. The outcomes presented in the results are from articles that pinpointed comorbid cardiovascular risks in individuals with HS and assessed the potential heightened risk beyond conventional factors. Studies that included specific statistics related to the most serious nature of CVD with data citing major adverse cardiovascular events (MACE) were also included.
Results
Relevant studies documenting CV risk in HS. HS has been the subject of recent interest as novel therapeutics emerge from the pharmaceutical industry. However, there remains a scarcity of evidence in the literature regarding life expectancy and the long-term systemic effects of HS’s chronic inflammatory implications on the cardiovascular system. CVD encompasses a diverse range of disorders affecting the heart and both arterial and venous blood vessels. CVDs account for 30 percent of global deaths, making them the leading cause of death worldwide. Arterial CVDs, primarily linked to atherosclerosis, include ischemic heart disease (angina pectoris, myocardial infarction), cerebrovascular disease (stroke, transient ischemic attacks), and peripheral arterial disease. Venous CVDs encompass conditions such as deep vein thrombosis and pulmonary embolism, along with other notable CVDs like arrhythmias and congestive heart failure. This article focuses on arterial CVDs and their associated risk factors in the context of HS with special attention directed at the risk of MACE.
Egeberg et al10 published a large Danish population cohort study (n=35,368) that revealed a markedly elevated risk of myocardial infarction (57%), ischemic stroke (33%), cardiovascular (CV) death (95%), MACE (53%), and all-cause mortality (35%) among patients with HS compared to the control group (Table 3). The adjusted confounders in this study were of age, sex, socioeconomic status, smoking, and medications. HS was associated with an elevated risk of MACE and all-cause mortality, irrespective of traditionally cited CV risk factors. Particularly noteworthy was the finding that the risk of CV death was 58 percent higher in patients with HS compared to those with severe psoriasis, indicating a substantial disparity.10 These findings might not be applicable to the US population, where African American individuals are more heavily impacted by HS and where the baseline prevalence of CVD could be higher. These authors concluded that HS is an independent risk factor for CVD.10
Tiri et al published a large (n=93,986) retrospective national registry study based on the Finnish population and reported a significantly diminished life expectancy in individuals with HS.22 Individuals with HS experienced a shortened life span of approximately five years compared to the controls. The study found that for individuals with HS, the mean age at death was 60.5 years. This compared to a mean of 71.1 years for patients with psoriasis and 75.2 years for the patients serving as controls (Table 2). However, this study differed from others by attributing the increased risk of mortality to the prolonged and intense systemic inflammation observed in HS. Chronic inflammation is known to be linked to conditions such as atherosclerosis and the development of cancer.22 Many publications cite HS as having multiple comorbidities, of which several are additionally listed as traditional CV risk factors like smoking, overweight or obesity, high cholesterol, hypertension, metabolic syndrome, and diabetes mellitus. Atherosclerosis is also a chronic inflammatory disease. Other chronic inflammatory diseases such as psoriasis, RA, and IBD, have been linked with an increased risk of CV disease independent of traditional CV risk factors. This phenomenon could be partially explained by shared inflammatory mechanisms.11,17,18,23–25
Reddy et al performed a large, retrospective, observational cohort study involving 49,862 individuals with HS and found an elevated risk of experiencing a myocardial infarction (MI) or cerebrovascular accident (CVA) in comparison to the control group.11 The data reported in this study showed that in comparison to the control group, individuals with HS demonstrated a 23 percent higher risk of experiencing a new MI or CVA. These findings were adjusted for pertinent CV factors and illustrate that the CVD risk of HS persists independently of the additional risk posed by traditional CV factors, such as smoking, obesity, hypertension, and Type 2 diabetes.11
A systematic review and meta-analysis to study the association of HS and stroke were reported by Phan et al.26 They observed a significantly elevated proportion of strokes in HS cases compared to controls (odds ratio [OR]: 1.74, 95% confidence interval [CI]: 1.45–2.09; p<0.00001). This analysis contributes to the growing body of evidence that HS is a systemic condition linked to life-threatening comorbidities. Dermatologic providers should be aware of this association to appropriately treat patients with HS and refer them to appropriate consultants for risk modification.
One additional consideration that needs to be factored in is the underlying treatment modalities for HS including biologics and systemic steroids. Adalimumab (a tumor necrosis factor [TNF] inhibitor) was approved to treat HS in 2016, but a small study in 2023 documented that in the best case scenario, adalimumab did not lower risk, and in the worst case scenario, it contributed to increased CV risk.26 Oba et al studied a group of 30 patients with moderate-to-severe HS being treated with adalimumab for at least six months compared to a group of 30 healthy individuals. The study’s limitations include the small study group and the absence of a patient group receiving nonbiologic therapies or untreated patients with HS. However, severe HS typically warrants systemic treatments, making it challenging to have a cohort of untreated patients with HS. Therefore, the impact of the disease itself on carotid intima-media thickness (CIMT) progression remains uncertain in this study. They could not definitively demonstrate causality regarding whether TNF inhibitors have a favorable or detrimental effect on the observed increase of CIMT during treatment. Nevertheless, these findings illustrated significant subclinical atherosclerosis disease progression in patients with severe HS undergoing biologic TNF inhibitor therapy.27 Patients with HS frequently receive short-term, high-dose steroid pulses during disease flares. The literature remains uncertain regarding the long-term CV consequences of such intermittent therapy.
Mechanism underlying HS and CVD. The precise underlying biological mechanism of HS remains incompletely defined. However, in studies specifically looking at HS skin lesions, there is documentation of increased immune mediators like interleukin-1beta (IL-1β), interleukin 17 (IL-17), TNF, and others.1 Studies have revealed that blood levels of TNF are increased, suggesting systemic inflammation. In addition, a recent study28 adds to this body of knowledge by quantifying that individuals with HS exhibit unfavorable systemic inflammatory burden, as evidenced by high serum leukocyte counts and C-reactive protein (CRP) levels. The elevation is even more notable compared to patients with psoriasis.
Discussion
This review consolidates existing literature on the topic. It emphasizes the need for further research to clarify the mechanisms linking HS and CV conditions, as well as delineating best clinical practices to mitigate risk. The current evidence does suggest that HS is an independent CV risk factor. As the global prevalence of both HS and CV diseases rises, acknowledging and addressing this correlation can shape holistic care strategies, potentially enhancing outcomes for affected individuals.
The connection between HS, CVD, and MACE is believed to originate from persistent systemic inflammation. Individuals with HS have documented lower levels of serum endothelial progenitor cells, which play a role in safeguarding the vascular endothelium. Additionally, elevated levels of proinflammatory cytokines such as IL-6, IL-17, and TNF contribute to atherosclerosis and thrombosis.29 Effective interventions addressing HS could potentially mitigate the risk of CVD and MACEs but long-term CV-focused research in this population is currently a gap in our collective knowledge base and additional studies are needed.
Clinical relevance of HS and CVD. Garg et al30 have published evidence-based recommendations for systematically screening comorbidities in patients with HS focused on US and Canadian populations.They evaluated the evidence’s strength and weighed the risks, benefits, and costs associated with screening for various comorbidities. The recommendation for screening for CV risk is rated II for level of evidence and B for strength of recommendation, which is the highest level and strength given for any of the comorbidities included in their comprehensive assessment. Current reports on comorbidity in HS show significant variability study design, focus, and methodological rigor. As such, recommendations continue to focus primarily on addressing the significant comorbid risk factors, which remain crucial until additional research has been completed to identify strategies aimed directly at systemic inflammation. They advocate for screening to involve a comprehensive review of systems, documentation of tobacco utilization, and laboratory evaluation for patients displaying signs and symptoms of diabetes.30 Flood et al published a visit guide for the management of HS, and in it they also advocate for comorbidity monitoring, which includes the screening for tobacco use and obesity with subsequent monitoring for metabolic syndrome and diabetes5 (Table 4). For patients with HS and existing comorbidities, dermatologists play a crucial role in supporting treatment adherence and patient monitoring. Dermatology specialists need to use the opportunity of a patient visit to stress the significance of healthy habits, especially in relation to smoking and alcohol use, diet, and physical activity. Regarding the screening for cardiac and metabolic comorbidities and the associated major adverse outcomes, Carton and Driscoll31 propose that traditional coronary risk assessment tools might not be sufficient, and a carotid ultrasound might be considered an additional modality to enhance the accuracy of CV risk stratification.
Traditional and novel CV risk factors. The spectrum of traditional CV risk factors for arterial CV diseases falls into three categories: behavioral, metabolic, and other. Behavioral risk factors comprise tobacco use, an unhealthy diet, and a lack of physical activity. Metabolic risk factors include diabetes, hypertension, dyslipidemia, and obesity. Additional recognized CV risk factors encompass age, male gender, psychological factors (eg, stress), genetics, excess homocysteine, and socioeconomic status. Clinically, healthcare providers often categorize these risk factors into nonmodifiable and modifiable aspects to prioritize actionable strategies for prevention or treatment.
Chronic inflammatory conditions like HS and psoriasis are often excluded from conventional CV risk listings, despite evidence to the contrary in clinical studies. Additional research is needed to fill the gap between simply identifying the risk and developing meaningful tools to appropriately risk stratify these patients along with providing evidence-based therapeutic interventions. For example, traditional CV risk calculators (based on the Framingham data) do not include systemic inflammation in the 10-year risk prediction. In addition, there are few studies to propose mechanisms for addressing the underlying chronic inflammation’s effect on the cardiovascular system.16,23,32,33
Conclusion
HS is not an uncommon inflammatory condition occurring in 1 to 4 percent of the US population with a previously unrecognized markedly elevated risk of adverse CV outcomes and overall mortality, independent of the accounted confounding factors. The risk of CV-associated death in HS was higher than those with severe psoriasis. These findings underscore the need for heightened awareness of this association and the necessity for further research into its clinical implications. Recognizing the association between HS and CV disease is crucial for comprehensive patient care. Collaboration between dermatologists, primary care providers, and CV specialists is imperative to assess and manage the overall health of patients with HS. Early identification and intervention for CV risk factors in HS individuals might alleviate CV comorbidities’ impact. In conclusion, individuals experiencing HS should be educated to their heightened risk of MACEs. All patients with HS should be screened early and provided with evidence-based primary prevention strategies tailored to their individual risks. As the global prevalence of both HS and CV diseases rises, acknowledging and addressing this correlation can shape holistic care strategies, potentially enhancing outcomes for affected individuals. An integrated, multidisciplinary approach that combines dermatological and CV perspectives is vital for optimizing patient care and navigating the complexities of managing HS and its associated CV comorbidities.
References
- Goldburg SR, Strober BE, Payette MJ. Hidradenitis suppurativa. J Am Acad Dermatol. 2020;82(5):1045–1058.
- Goldburg SR, Strober BE, Payette MJ. Hidradenitis suppurativa. J Am Acad Dermatol. 2020;82(5):1061–1082.
- González-López MA, Hernández JL, Lacalle M, et al. Increased prevalence of subclinical atherosclerosis in patients with hidradenitis suppurativa (HS). J Am Acad Dermatol. 2016;75(2):329–335.
- Martorell A, Jfri A, Ochando G, Mayo F. Present and future trends of biologic therapies and small molecules in hidradenitis suppurativa. J IMIDs. 2022;2(1):7591.
- Flood KS, Porter ML, Kimball AB. A visit guide for hidradenitis suppurativa—Managing a complex disease in a busy clinic. J Am Acad Dermatol. 2021;84(3):e155–e160.
- Dufour DN, Emtestam L, Jemec GB. Hidradenitis suppurativa: a common and burdensome, yet under-recognised, inflammatory skin disease. Postgrad Med J. 2014;90(1062):216–221.
- Krajewski PK, Matusiak L, VonStebut E, et al. Pain in hidradenitis suppurativa: A cross-sectional study of 1,795 patients. Acta Derm Venereol. 2021;101(1):1485.
- Chadha SA, Stout MA, Goyal PK, et al. Assessing unmet needs in patients with hidradenitis suppurativa. Arch Dermatol Res. 2023;315(9):2555–2560.
- Smith S. Hidradenitis suppurativa: Managing a complex disease with multiple comorbidities. J Dermatol Physician Assist. 2022;16(2).
- Egeberg A, Gislason GH, Hansen PR. Risk of major adverse cardiovascular events and all-cause mortality in patients with hidradenitis suppurativa. JAMA Dermatol. 2016;152(4):429–434.
- Reddy S, Strunk A, Jemec GBE, Garg A. Incidence of myocardial infarction and cerebrovascular accident in patients with hidradenitis suppurativa. JAMA Dermatol. 2020;156(1):65–71.
- Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics–2020 update: A report from the American Heart Association. Circulation. 2020;141(9):e139–e596.
- Wassif H, Saad M, Desai R, et al. Outcomes following acute coronary syndrome in patients with and without rheumatic immune‐mediated inflammatory diseases. J Am Heart Assoc. 2022;11(18):e026411.
- Lloyd-Jones DM, Braun LT, Ndumele CE, et al. Use of risk assessment tools to guide decision-making in the primary prevention of atherosclerotic cardiovascular disease. J Am Coll Cardiol. 2019;73(24):3153–3167.
- González I, Pascual JC, Corona D, et al. European heart systemic coronary risk evaluation may underestimate cardiovascular risk after assessing cardiovascular disease with carotid ultrasound in hidradenitis suppurativa. Br J Dermatol. 2018;178(1):e22–e23.
- Studziński K, Tomasik T, Krzysztoń J, et al. Effect of using cardiovascular risk scoring in routine risk assessment in primary prevention of cardiovascular disease: an overview of systematic reviews. BMC Cardiovasc Disord. 2019;19(1):11.
- Karbach S, Hobohm L, Wild J, et al. Impact of psoriasis on mortality rate and outcome in myocardial infarction. J Am Heart Assoc. 2020;9(18):e016956.
- Garshick MS, Berger JS. Psoriasis and cardiovascular disease—An ounce of prevention is worth a pound of cure. JAMA Dermatol. 2022;158(3):239–241.
- Berna-Rico E, Abbad-Jaime De Aragon C, Garcia-Aparicio A, et al. Cardiovascular screening practices and statin prescription habits in patients with psoriasis among dermatologists, rheumatologists and primary care physicians. Acta Derm Venereol. 2023;103:adv5087.
- Mehta NN, Azfar RS, Shin DB, et al. Patients with severe psoriasis are at increased risk of cardiovascular mortality: cohort study using the General Practice Research Database. Eur Heart J. 2010;31(8):1000–1006.
- Dregan A, Chowienczyk P, Molokhia M. Cardiovascular and Type 2 diabetes morbidity and all-cause mortality among diverse chronic inflammatory disorders. Heart. 2017;103:1867–1873.
- Tiri H, Jokelainen J, Timonen M, et al. Substantially reduced life expectancy in patients with hidradenitis suppurativa: a Finnish nationwide registry study. Br J Dermatol. 2019;180(6):1543–1544.
- Lockshin B, Balagula Y, Merola JF. Interleukin 17, inflammation, and cardiovascular risk in patients with psoriasis. J Am Acad Dermatol. 2018;79(2):345–352.
- Takeshita J, Grewal S, Langan SM, et al. Psoriasis and comorbid diseases. J Am Acad Dermatol. 2017;76(3):393–403.
- Bigeh A, Sanchez A, Maestas C, Gulati M. Inflammatory bowel disease and the risk for cardiovascular disease: Does all inflammation lead to heart disease? Trends Cardiovasc Med. 2020;30(8):463–469.
- Phan K, Ng WHS, Lai B, et al. Hidradenitis suppurativa and association with stroke: systematic review and meta-analysis. J Dermatol Treat. 2022;33(4):2309–2316.
- Oba MC, Askin O, Gunver MG, et al. Subclinical atherosclerosis in patients with hidradenitis suppurativa treated with TNF inhibitors. Skin Res Technol. 2023;29(3):e13302.
- Riis PT, Søeby K, Saunte DM, Jemec GBE. Patients with hidradenitis suppurativa carry a higher systemic inflammatory load than other dermatological patients. Arch Dermatol Res. 2015;307(10):885–889.
- Bailey AMJ, Li HOY, Tan MG, Kirchhof MG. Hidradenitis suppurativa and major adverse cardiac events: A systematic review and meta-analysis. J Am Acad Dermatol. 2021;84(3):844–848.
- Garg A, Malviya N, Strunk A, et al. Comorbidity screening in hidradenitis suppurativa: Evidence-based recommendations from the US and Canadian Hidradenitis Suppurativa Foundations. J Am Acad Dermatol. 2022;86(5):1092–1101.
- Cartron A, Driscoll MS. Comorbidities of hidradenitis suppurativa: A review of the literature. Int J Womens Dermatol. 2019;5(5):330–334.
- Tsiogka A, Gregoriou S, Stratigos A, et al. The impact of treatment with IL-17/IL-23 inhibitors on subclinical atherosclerosis in patients with plaque psoriasis and/or psoriatic arthritis: A systematic review. Biomedicines. 2023;11(2):318.
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults. J Am Coll Cardiol. 2018;71(19):e127–e248.