J Clin Aesthet Dermatol. 2020;13(2):58–60
 by Ankita Tuknayat, MBBS, MD; Mala Bhalla, MD; Amrit Kaur MBBS; and Shimona Garg, MD
by Ankita Tuknayat, MBBS, MD; Mala Bhalla, MD; Amrit Kaur MBBS; and Shimona Garg, MD
All authors are with the Department of Dermatology, Venereology and Leprosy, Government Medical College and Hospital in Chandigarh, India.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Dermatophytes are keratinophilic fungi responsible for skin, nail, and scalp infections. Chronic dermatophytosis, defined as persistent infection for six months or more, was very rare in the 1980s and mostly limited to patients with nail involvement, but this is no longer true. Currently, patients with chronic dermatophytosis are increasing, and about 50 percent of patients with dermatophytosis have at least one other member of their family infected at the same time, sometimes with entire families being affected at once.
Objective. We sought to study the possible risk factors associated with familial dermatophytosis.
Methods. The present questionnaire-based study was conducted from May 2017 to July 2017. Patients with a clinical diagnosis of dermatophytosis and at least one other family member affected were included. A proforma was filled and history was taken, including number of family members affected, site of infection in the index case, site(s) of infection of all other subsequent family members affected, and use of over-the-counter drugs.
Results. Out of the 113 families surveyed, which included 673 subjects, a little over half (55.4%) were affected by dermatophytosis. In 103 families, the initial site of infection in the subsequent family member affected was the same site as that affected in the first member. All families reported a history of using an irritant soap and over-the-counter drugs. Washing all the family’s clothing together was a common factor. All families had a single bathroom and used the same soap and stool for bathing.
Conclusion. Through our survey, we identified possible risk factors that might be responsible for the increasing epidemic of familial dermatophytosis in India, including sharing of soaps and towels, washing clothes in the same vessel, sharing of lavatories, abuse of topical steroids and over the counter topicals, and use of antiseptic soaps that kill normal flora.
KEYWORDS: Dermatophytosis, familial, chronic, recurrent
Dermatophytes are keratinophilic fungi responsible for skin, nail, and scalp infections, which compose the most common types of superficial cutaneous fungal infections seen in humans and animals.1 A recent increase in the number of patients and the chronicity of this superficial infection has been observed, with more than 50 percent of the total daily patients visiting our dermatology department being affected with dermatophytosis. Chronic dermatophytosis, defined as a persistent infection for six months or longer, was very rare in the 1980s and was mostly limited to afflicting patients with nail involvement, but this no longer holds true.2 Currently, the number of patients with chronic dermatophytosis are increasing steadily.3 Further, 50 percent of patients with dermatophytosis have at least one other family member who is infected at the same time, sometimes with entire families being impacted.4 Recently, there has been an increase in patients presenting with dermatophytic infections and increased failure of therapy, including oral antifungal drugs, such as terbinafine, itraconazole, and griseofulvin—not only in India, but in many other countries.5,6 Dermatophytosis, which was previously relatively easy to treat, has now become a menace.
Familial dermatophytosis seems to be an important contributing factor to increasing rates of treatment failure; if one member of a family remains untreated or undetected, such leads to a recurrence in the other members. This increased prevalence has led to a search for contributing factors that might be responsible for this phenomenon. As evidenced in the literature, hidden cases of dermatophytosis might be associated with increased infection in a single family.1 Similarly, it has been observed that patients with recurrent or chronic dermatophytosis usually have more than one affected family member.4 This imposes a financial burden on the entire family. As it is an infectious disease, fomites play a major role and can vary as per the traditional culture and practices. The practice of hand-washing clothes in India in a single vessel, as opposed to the use of high-temperature washing machines in the West, is suspected to have a huge impact on the spread of infection.7 Sharing a bathing stool for sitting while taking a bath is also more prevalent in India compared to showering in the West. India, being a tropical country, has always been prone to dermatophytosis onset, but there has been a jump in the incidence and prevalence of familial dermatophytosis in recent years.4 Though genetic predisposition is known, genetic changes occur slowly over time, while this change in presentation occurred suddenly.8–10
When an entire family is affected with an infectious disease, the role of fomites cannot be excluded and, thus, their nature becomes important in any examination. Here, we investigated possible contributing factors that might be responsible for the increasing spread of familial dermatophytosis and chronic recalcitrant dermatophytosis among families in India.
Materials and Methods
This was a questionnaire-based study performed from May 2017 to July 2017. Patients with chronic (lasting more than 6 months) or recurrent (more than one episode in the past year) dermatophytosis attending the outpatient department of dermatology clinic at the Government Medical College and Hospital in Chandigarh, India, who also had at least one affected family member, were recruited into the study. Specific inclusion criteria were patients of any age with a clinical diagnosis of dermatophytosis by at least two dermatologists and potassium hydroxide (KOH) test positivity in at least one family member. The exclusion criterion was an inability to provide reliable history information. Informed consent was received from all included patients and the study was approved by the institutional review board.
Eligible patients with chronic or recurrent dermatophytosis who had an additional family member affected were identified and the proforma was filled out by the investigator. There was a 100-percent participation rate among those identified; a proforma was completed for all patients and a detailed history was taken, including information regarding possible contributing risk factors, such as the first family member affected, number of family members affected, site of infection in the index case, site(s) of infection of all other subsequent family members affected, occupation, animal contact, soap/detergent used to bathe/wash, number of lavatories in the house, daily washing/ironing of clothes, use of over-the-counter drugs, the type of lavatory in the house, sharing of clothes/towels, use of antiseptic soaps, washing all the clothes in the same vessel, use of the same bathing stool, use of the same soap, any discoloration of the nails, and history of ironing clothes. One proforma each was dedicated to one family. A total of 113 families were included. Data were analyzed and correlated.
Results
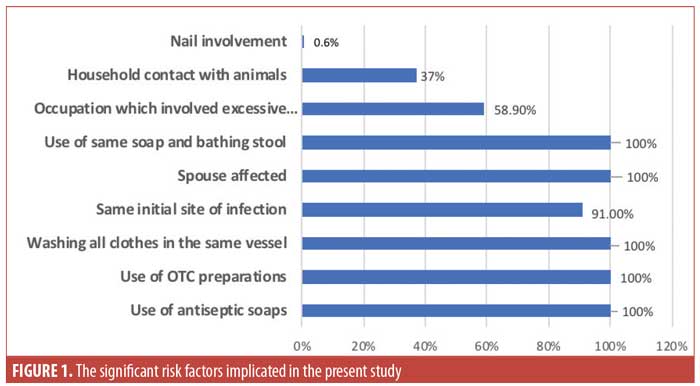
Out of the 113 families included, which encompassed 673 subjects, 373 (55.4%) were affected by dermatophytosis. The study population was 54 percent male (n=202) and 45 percent female (n=171). In 17 percent (n=20) of families, all members (n=89) were affected, including 50 adults and 39 children (aged younger than 12 years). Men were more often the first to be affected (index cases). Cruris was the initial site of infection in most patients (n=87 families; 76.9%) of patients. The spouse of the affected patient was always affected. In 91 percent (n=103) families, the initial site of infection in the subsequent member affected was the same site as that affected in the first member. All families reported a history of using an antiseptic/irritant soap and detergent and using over-the-counter drugs before responding to us. Washing all of the clothes together was also a common factor in all cases. Further, all affected families had a single bathroom and used the same soap and stool for bathing. Fifty-two families (46%) had a Western type of lavatory in their homes. while 42 families (37%) reported the practice of sharing towels. Out of 373 affected by dermatophytosis, 220 (58.9%) had an occupation which involved excessive sweating; meanwhile, 42 (37%) families had a household contact with animals (Figure 1). Nail involvement was reported in seven (0.6%) families and these were those families in which all members were affected.
Discussion
The pattern of superficial dermatophytosis has changed in the past few years and the disease is quickly emerging as a chronic and recalcitrant disease. The routine regimens found in the literature are no longer as effective as they were in the past.5,6
In the past, superficial dermatophytosis was easy to treat, so the risk factors for spreading the disease were not studied in detail. However, the recent increases in infection and recurrence rates has led to more interest in potential risk factors as a means to improve treatment outcomes. Familial dermatophytosis might be an important contributor to treatment failure.1 In our study, the spouse of the index case was always affected. This conjugal spread demonstrates transfer by close physical contact and might also be a reason for tinea cruris being the most common presentation.
In our study, all families (100%) reported the use of antiseptic and neem soaps. Because of excessive advertisement, many people have recently begun using antiseptic soaps in an attempt to decrease skin infection;2 however, the recent increase in dermatophytic infection might be an indicator that these soaps are interfering with the normal commensal skin flora, which might be an important part of the innate defense mechanism of the body.11 Such soaps are usually irritants, which can lead to an increase in itching, and thus make it easy for the microorganisms to break the barrier and cause infection. The excessive commercialization and marketing of these soaps imparts a false sense of security in those who purchase them; however, these antiseptics might be further exaggerating the problem. Cleaning practices also vary, but in the Indian homes that have shifted to the Western lavatory system, there is a wide variability in cleaning practices. Generally, toilets are cleaned once a day in the house and not after every use by a different member of the family. Toilet seat cover tissues are not commonly used.11 All of these factors point toward poor hygiene, which is a well-known risk factor for acquiring dermatophytosis. Further, even using strong disinfectants to clean the toilet seats that come into direct contact with the skin might cause irritant reactions, and thus, lead to an increase in the entry of infective organisms.
All families (100%) reported a positive history of use of various over-the-counter combination creams.12 Schaller et al13 noted that the addition of a corticosteroid cream to an antifungal agent decreases the inflammatory symptoms and increases patient adherence and efficacy of the antigungal agent, while abuse of these therapies leads to adverse effects and recalcitrant infection.
However, this is a double-edged sword.13 The increasing use of over-the-counter “steroid cocktail” preparations, which include antifungal, antibacterial, and potent topical steroids in various combinations, have contributed to facilitating recurrent and recalcitrant infections.14 Quadriderm (Schering-Plough, Kenilworth, New Jersey), which is available in India over the counter, includes betamethasone, tolnaftate, clioquinol, and gentamicin. Topical steroids decrease inflammation and the immune response, leading to a persistence of infection as the inflammatory response is the key to promoting the clearance of infection.14 These medications also reduce scaling, which is responsible for false-negative KOH tests. The use of topical steroids has seen emergence of atypical tinea infections, such as pseudoimbricata and eczematous dermatitis.14
The use of the same stool and the same soap for bathing were reported in all affected families is an important potential contributing factor to consider; this might also be a reason for tinea cruris being the most common site of infection. Washing all clothing together in the same vessel was reported in all affected families (100%) as well. Fifty-two families (46%) had a Western-type lavatory in their homes, which might also lead to increased transference of infection. In a study from Hammer et al,15 it was found that Trichophyton rubrum survived for about 12 weeks on a towel, whereas Trichophyton mentagrophytes survived for more than 25 weeks. Trichophyton can survive off the host body as spores and infect when they find a suitably warm temperature. Thus, the spores might be surviving on fomites, leading increased infections within families.7 Using radioactively labeled carbon, Hammer et al15 also demonstrated that up to 10 percent of the fungal spores transfer from contaminated to sterile clothes during storage at the same place and up to 16 percent of the spores transfer during washing in the same vessel. Thus, it might be of benefit to counsel patients about the importance of disinfecting clothes and storing and washing all contaminated clothes separately. Clothes should be washed in hot water at 60°C and dried in sunlight, as this is the most effective natural way of disinfection.7,16 In our study, there was also a lack of ironing of clothes in all included families, which might also have contributed to the persistence of infection.
Lifestyle changes also have a major role. There has been growing wear of more occlusive and synthetic clothes, such as jeans and lycra, which increases irritation and sweating, thus increasing the chances of infection. Sweating has been well established as a risk factor for increasing the prevalence of dermatophytosis. This has been highlighted by the various eponyms used in dermatophytosis, such as Jock’s itch, Dhobis itch, and athlete’s foot.17,18 Sweating in conjunction with other factors, such as poor hygiene, might further increase the incidence of dermatophytosis. In a study by Ranganathan et al,18 the authors found that people who were engaged in occupations associated with increased sweating (58.9%), such as laborers, exhibited increased incidence rates of dermatophytosis relative to those who were not engaged in such occupations. Ranganathan et al also reported that chronic and extensive dermatophytosis is most prevalent in very low and low-income groups.18 This is similarly corroborated in our study, where most of the patients belonged to a low-income group. Another potentially important factor is the recent change of the causal agent of dermatophytosis from Trichophyton rubrum to Trichophyton mentagrophytes, which might change efficacy of the existing oral and topical antifungals.3,4 Nail involvement was reported in seven families (0.6%) in this study. In these families, all members were affected. Early unnoticed nail involvement was considered an important factor responsible for chronicity and the relapse of infection but, in this study, it seems to be of minor significance.13 However, although nail involvement was uncommon among our participants, over time, all family members eventually contracted the infection, which highlights nail involvement as an important potential contributing factor to disease spread.
A new term, “unresponsive dermatophytosis,” has been introduced for cases that cannot be characterized as chronic or recalcitrant.11 It is unknown whether patients with this condition have relapsed due to unnoticed nail infection or have been reinfected by an unidentified family member.
Conclusion
India is a tropical country. Recently, there has been a rise in chronic and recalcitrant dermatophytosis cases across India. The causes for this change are unknown and it is not clear whether to attribute the observation to changes in the host, environment, or the causative organism. Here, we identified potential risk factors among our participants that might contribute to the increasing epidemic of dermatophytosis, including sharing of soaps and towels, washing clothes in the same vessel, sharing of lavatories, abuse of topical steroids and over the counter topicals, and use of antiseptic soaps that kill normal flora. Further studies are required to offer corroborating evidence.
References
- Verma S, Madhu R. The great Indian epidemic of superficial dermatophytosis: an appraisal. Indian J Dermatol. 2017;62(3):227–236.
- Panda S, Verma S. The menace of dermatophytosis in India: the evidence that we need. Indian J Dermatol Venereol Leprol. 2017;83(3):281.
- Putta SD, Kulkarni VA, Bhadade AA, et al. Prevalence of dermatophytosis and its spectrum in a tertiary care hospital, Kolhapur. Indian J Basic Appl Med Res. 2016;5(3):595–600.
- Bhatia VK, Sharma PC. Epidemiological studies on Dermatophytosis in human patients in Himachal Pradesh, India. Springerplus. 2014;3:134.
- Yamada T, Maeda M, Alshahni MM, et al. Terbinafine resistance of Trichophyton clinical isolates caused by specific point mutations in the squalene epoxidase gene. Antimicrob Agents Chemother. 2017;61(7). pii: e00115–17.
- Martinez-Rossi NM, Bitencourt TA, Peres NTA, et al. Dermatophyte resistance to antifungal drugs: mechanisms and prospectus. Front Microbiol. 2018;9:1108.
- Amichai B, Grunwald MH, Davidovici B, et al. The effect of domestic laundry processes on fungal contamination of socks. Int J Dermatol. 2013;52(11):1392–1394.
- Zaugg C, Monod M, Weber J, et al. Gene expression profiling in the human pathogenic dermatophyte Trichophyton rubrum during growth on proteins. Eukaryot Cell. 2008;8(2):241–250.
- Serjeantson S, Lawrence G. Autosomal recessive inheritance of susceptibility to tinea imbricata. Lancet. 1977;1(8001):13–15.
- Zhan P, Dukik K, Li D, et al. Phylogeny of dermatophytes with genomic character evaluation of clinically distinct Trichophyton rubrum and T. violaceum. Stud Mycol. 2018;89:153–175.
- Dogra S, Uprety S. The menace of chronic and recurrent dermatophytosis in India: Is the problem deeper than we perceive? Indian Dermatol Online J. 2016;7(2):73–76.
- Erbagci Z. Topical therapy for dermatophytoses: should corticosteroids be included? Am J Clin Dermatol. 2004;5(6):375–384.
- Schaller M, Friedrich M, Papini M, et al. Topical antifungal–corticosteroid combination therapy for the treatment of superficial mycoses: conclusions of an expert panel meeting. Mycoses. 2016;59(6): 365–373.
- Verma SB. Topical corticosteroid misuse in India is harmful and out of control. BMJ. 2015;351:h6079.
- Hammer TR, Mucha H, Hoefer D. Infection risk by dermatophytes during storage and after domestic laundry and their temperature-dependent inactivation. Mycopathologia. 2011;171(1):43–49.
- Amichai B, Grunwald MH, Davidovici B, et al. “Sunlight is said to be the best of disinfectants”: the efficacy of sun exposure for reducing fungal contamination in used clothes. Isr Med Assoc J. 2014;16(7):431–433.
- Brodin MB. Jock Itch. Phys Sportsmed. 1980;8(2):102–108.
- Ranganathan S, Menon T, Selvi SG, et al. Effect of socio-economic status on the prevalence of dermatophytosis in Madras. Indian J Dermatol Venereol Leprol.1995;61(1):16–17.

