J Clin Aesthet Dermatol. 2021;14(10):32–34.
 by Subuhi Kaul, MD; Ishmeet Kaur, MD; and Deepak Jakhar, MD
by Subuhi Kaul, MD; Ishmeet Kaur, MD; and Deepak Jakhar, MD
Dr. Kaul is with the Department of Internal Medicine, John H. Stroger Hospital of Cook County in Chicago, Illinois. Drs. Kaur and Jakhar are with the Department of Dermatology, North Delhi Municipal Corporation Medical College and Hindu Rao Hospital in New Delhi, India.
ABSTRACT: Use of a facial mask is a necessity during the current pandemic. The associated occlusion with extended daily use can lead to physiological changes in the skin with resultant irritation, itching, and infections. This can lead to exacerbation of pre-existing dermatoses or induction of irritant dermatitis or bacterial folliculitis. We observed several patients with previously controlled acne vulgaris who developed a flare. Also, in those without a history of pre-existing acne, an acneiform eruption was noted. The majority of patients were women who had pre-existing acne and needed to wear a N95 respirator or a surgical mask for several hours a day, every day. A few suggested simple preventative measures provided herein might help this vulnerable population.
Key words: N95, face, mask, acne, acneiform eruption, rash, COVID-19, maskne
Several countries have guidelines and policies mandating facial mask use in public places as part of the effort to contain the spread of severe acute respiratory syndrome coronavirus 2, responsible for coroanvirus disease 2019 (COVID-19). For occupations that require employees to be physically present at the workplace, such as, in the healthcare or service industries, this entails several hours of facial mask use every day. This extended mask wear can lead to prolonged cutaneous occlusion and contact with sensitizing chemicals. As a result, several dermatoses have been observed with facial mask use, including, irritant contact dermatitis, allergic contact dermatitis, flare of rosacea, and contact urticaria.1 A previous study found that skin adverse effects, including itching, rash, and acne, were common with N95 respirator use but not with surgical mask use.2 The present observational study describes cases with acne or acneiform eruption related to the use of both surgical face masks and N95 respirators.
Case Report
We report 10 cases of mask-related acne and acneiform exacerbation observed in two tertiary care centers located in New Delhi, India, and Chicago, Illinois, United States, respectively. The mean age of the patients was 26.3 years, and all were female except for one. Four of these patients (40%) were healthcare workers and wore surgical (polypropylene) masks for more than eight hours per day with intermittent N95 respirator use. One of these healthcare workers also used plastic goggles for eye protection and developed erythematous papules predominantly on the nasal bridge. Other patients were in different service settings and had to use face masks for more than six hours every day. Out of the 10 included patients, six had a previous history of acne vulgaris, which was well controlled prior to mask use. In the patients with pre-existing acne, new-onset pustules and inflammatory papules predominantly in the area covered by the mask were noticed. Four patients had no past history of acne vulgaris before wearing a face mask. In those patients, the area covered by a mask developed erythema and multiple pustules. None of the patients had a history of rosacea in the past. All patients complained of itching and irritation in the mask area, while a burning sensation was reported by four patients. Three patients had history of atopy, which was well controlled. All patients worked in an ambient temperature of 22°C to 24°C during office hours. The most commonly affected areas were the cheeks and chin, followed by the nose. The average time to onset of the flare was about 3.4 weeks (range, 2–8 weeks) after daily mask use. None of these patients used any topical or systemic medications with the potential to induce or flare up acne or cause acneiform eruptions. One patient opted to wear a cotton mask with the surgical mask over it, with a resultant decrease in irritation. The clinical and mask-related characteristics of the patients are summarized in Table 1.
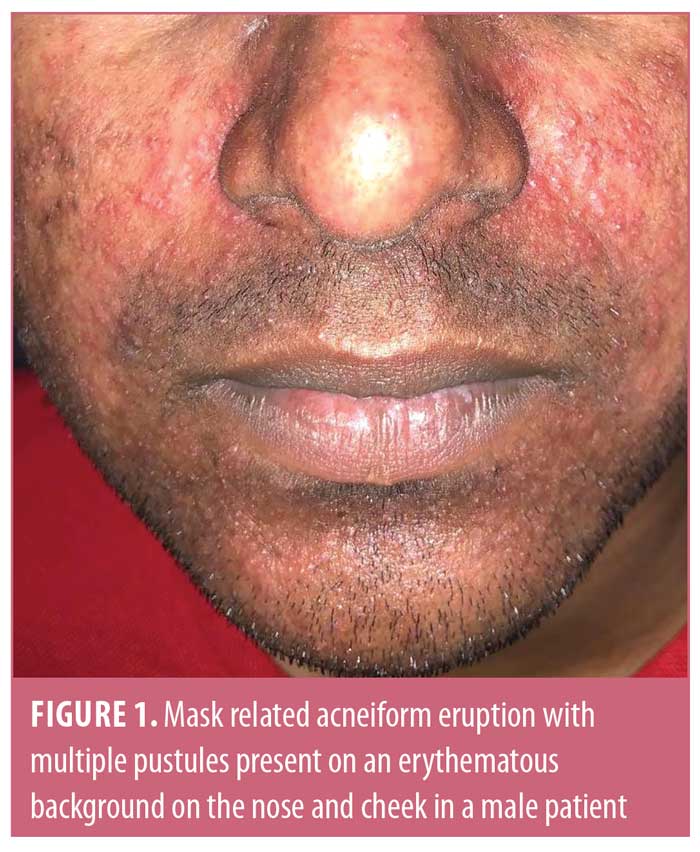
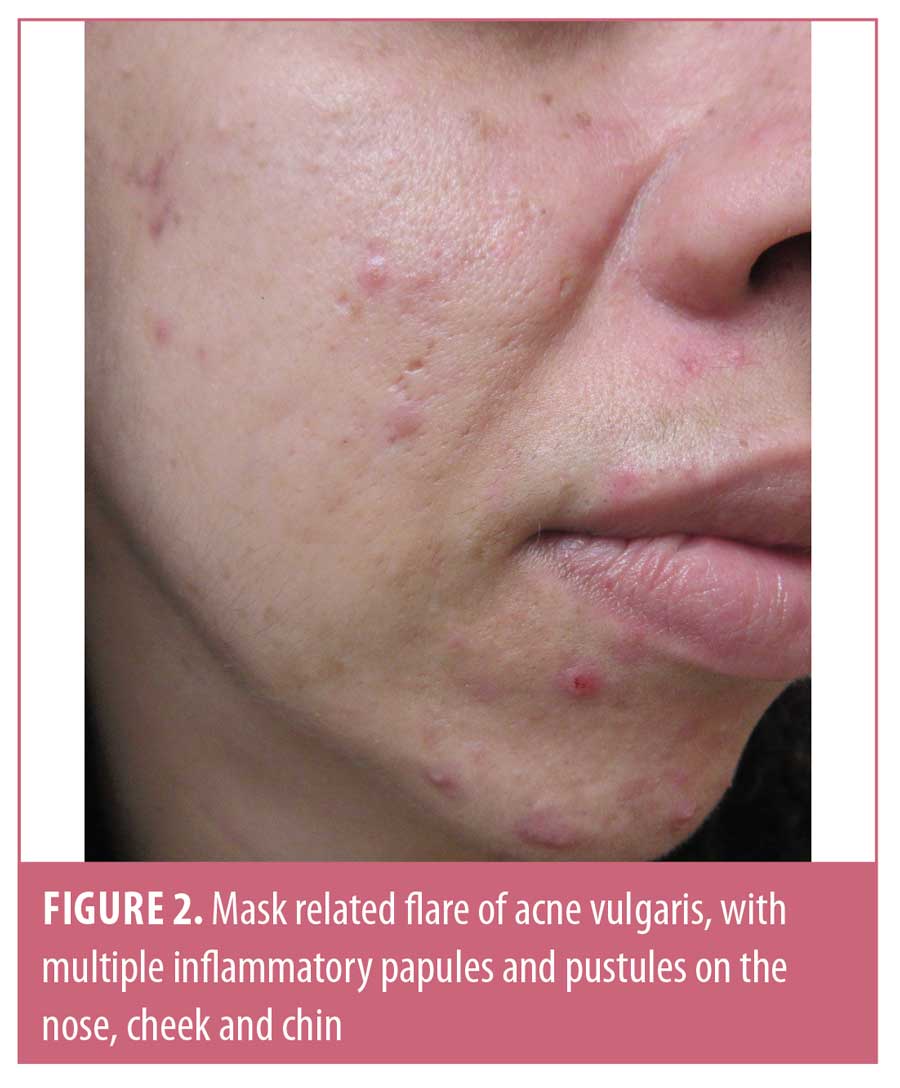

Mask-related acne and acne-like eruptions have been referred to as “maskne” in the news and on social media.3 Patient education materials, including self-care tips for the prevention and amelioration of facial mask-related skin problems, have been made available online by the American Association of Dermatology.4 Although, Foo et al5 found acne to be the most common adverse effect of face mask use, other authors did not find it to be common.6 This discrepancy might due to a decreased presentation to dermatologists given the restrictions on clinic visits brought on by COVID-19 and prolonged wait times for dermatology appointments. We observed flares of acne and the development of erythema and acneiform eruptions in several patients. This observation was made regardless of geographic location and associated differences in climates, highlighting the role of occlusion in the pathogenesis of maskne. However, our observation was limited by the lack of a control group and the absence of histopathological confirmation of diagnoses.
Possible mechanisms of maskne include follicular plugging from trapped oils and altered skin flora subsequent to prolonged cutaneous occlusion. Theoretically, these changes can lead to increased inflammation; however, the exact mechanism of acne exacerbation or acneiform eruption is uncertain. Additionally, occlusion can lead to deleterious changes in the skin barrier, which can explain the increased cutaneous irritation accompanying mask wear. The commonly described changes are an increase in passive transepidermal water loss (TEWL), a change in skin flora composition, increased bacterial counts, and increased pH, all of which can lead to compromised barrier function.7,8 These changes can increase the predilection for contact irritant dermatitis, infections such as bacterial folliculitis, or a flare of pre-existing dermatoses like atopic or seborrheic dermatitis.9 Occlusion can also potentiate the irritative potential of any topical products.8
The physiological effects of donning medical masks and N95 respirators among patients without pre-existing skin conditions were evaluated by Hua et al,6 who found that, with both N95 respirator and surgical masks, TEWL, erythema, skin pH, skin hydration, and sebum production were increased in the area covered, and these changes persisted even after mask removal in the case of N95 respirators.6 Furthermore, a survey found that about 50 percent of patients who used facial masks experienced pruritus and erythema, with longer times of face mask or goggle use associated with two times higher odds of skin damage.10
Suggested general preventive measures include 1) daily changing of masks, in the case of surgical masks; 2) washing the mask after every use, in the case of cloth masks; 3) avoidance of occlusive substances like oil- or petrolatum-based emollients or cosmetic products; 4) use of a mild non-soap-based cleanser for the cleaning face; and 5) regular break times with removal of masks for 15 minutes every four hours in a socially distant space, such as outdoors or in one’s own car.4 Specific therapeutic modalities include the use of a mild retinoid at night (short contact period), either daily or on alternate nights as tolerated, especially in those with pre-existing acne. Although retinoids can help prevent acne flares and might be preferred over benzoyl peroxide for this reason, they can also cause significant irritant dermatitis. This adverse effect is particularly pronounced when combined with the occlusive effect of a mask; therefore, care should be taken to avoid prolonged contact times and combination with other irritants such as salicylic acid or benzoyl peroxide, and the use of a noncomedogenic emollient prior to mask use should be encouraged. The use of oral antibiotics, topical antibiotics, and oral isotretinoin can be decided on a case-by-case basis.
Conclusion
Mask-related skin eruptions are not uncommon and are especially associated with prolonged wearing of masks. Patients and the general population should be educated regarding the general measures required to minimize these side effects.
References
- Aerts O, Dendooven E, Foubert K, et al. Surgical mask dermatitis caused by formaldehyde (releasers) during the COVID-19 pandemic. Contact Dermatitis. 2020;83(2):172–173.
- Hu K, Fan J, Li X, et al. The adverse skin reactions of health care workers using personal protective equipment for COVID-19. Medicine (Baltimore). 2020;99(24):e20603.
- Rubin C. Maskne is the new acne, and here’s what is causing it. https://www.nytimes.com/article/maskne-acne.html. Accessed August 8, 2020.
- American Association of Dermatology. 9 ways to prevent face-mask skin problems. https://www.aad.org/public/everyday-care/skin-care-secrets/face/prevent-face-mask-skin-problems. Accessed August 8, 2020.
- Foo CCI, Goon ATJ, Leow Y, Goh C. Adverse skin reactions to personal protective equipment against severe acute respiratory syndrome—a descriptive study in Singapore. Contact Dermatitis. 2006;55(5):291–294.
- Hua W, Zuo Y, Wan R, et al. Short-term skin reactions following use of N95 respirators and medical masks. Contact Dermatitis. 2020;83(2):115–121.
- Aly R, Shirley C, Cunico B, Maibach HI. Effect of prolonged occlusion on the microbial flora, pH, carbon dioxide and transepidermal water loss on human skin. J Invest Dermatol. 1978;71(6):378–381.
- Zhai H, Maibach HI. Skin occlusion and irritant and allergic contact dermatitis: an overview. Contact Dermatitis. 2001;44(4):201–206.
- Bolognia JL, editor. Dermatology: Expert Consult. 3rd edition. Edinburgh, Scotland: Elsevier; 2012.
- Lan J, Song Z, Miao X, et al. Skin damage among health care workers managing coronavirus disease-2019. J Am Acad Dermatol. 2020;82(5):1215–1216.

