 J Clin Aesthet Dermatol. 2021;14(3 Suppl 1):S20-S22
J Clin Aesthet Dermatol. 2021;14(3 Suppl 1):S20-S22
by Archana M. Sangha, MMS, PA-C
Ms. Sangha is a Fellow of the American Academy of Physician Assistants and Diplomate and Current President of the Society of Dermatology Physician Assistants. She practices general, surgical, and cosmetic dermatology in Bethesda, Maryland.
FUNDING: No funding was provided for this article.
DISCLOSURES: Ms. Sangha is a consultant for Sanofi/Regeneron, Incyte, Ortho Dermatologics, Pfizer, and Leo.
Population studies within the United States show that atopic dermatitis (AD) disproportionately affects African Americans (AA) in comparison to other ethnic populations. For example, approximately 19.3 percent of AA children are impacted by AD compared to 16.1 percent of European Americans (EA) and 7.8 percent of Hispanics. Worldwide, AD was found to be more prevalent in Africa and Oceania in comparison to India and Europe.1–3
AD is a multifactorial, complex skin disorder that has recently been shown to have key molecular phenotypic differences among varying ethnic populations. One study showed that AD among AA has decreased TH1 and TH17 but share similar upregulation of Th2 and Th22, as seen in EA patients.4 Another study showed that in Asian populations, there is markedly higher TH17 and TH22 and lower TH1/interferon in comparison to EA patients.5 Histologically, AD skin in both EA and Asian patients is characterized by epidermal hyperplasia. However, Asian patients show features most commonly seen in psoriasis histology, such as prominent epidermal hyperplasia, elongated rete ridges, parakeratosis, and hypogranulosis.6 These studies demonstrate that there are immunologic variabilities between various racial groups. Further studies are needed to examine and identify other phenotypic variabilities among other ethnic populations.
Varying Signs and Symptoms
While AD among all races presents with itch being the hallmark symptom, the appearance of skin lesions has variability among different skin types. In lighter skin types, AD classically presents with erythematous patches and plaques affecting flexor surfaces. In darker skin types, AD has a greater propensity for papulation, lichenification (Figure 1), and pigmentary changes. It also favors extensor surfaces in skin of color.7 Erythema in darker skin types often presents as a violaceous hue, an ashen gray or darker brown color (Figure 2). Since erythema is more difficult to detect in darker skin types, clinicians can mistakenly minimize disease severity in patients with AD. Black/African patients also have an increased tendency for hyperlinearity of the palms, periorbital dark circles, Dennie-Morgan lines, and prurigo nodularis (Figure 3).8 AD in Asian populations often has psoriasiform features,9 with lesions having more well-defined borders with increased scaling and lichenification

Treatment and Management Methods
The treatment goals of AD remain the same regardless of skin type. The goals are to prevent and manage flares while working to repair and improve the function of the skin barrier. Studies have shown that skin barrier dysfunction is the initial step in the development of AD. Many factors impact skin barrier dysfunction, including but not limited to immune dysregulation, filaggrin mutations, deficiency of antimicrobial peptides, and skin dysbiosis.10 A compromise in skin barrier causes a loss of moisture in the skin while allowing irritants and allergens to enter the skin. Discussing proper skincare is a fundamental step in the treatment of AD, but one that is often overlooked in a busy clinical practice. Studies have shown that the number of topical corticosteroids (TCs) used can be significantly reduced by proper skin hydration through regular and frequent use of unscented emollients.11
Managing exacerbations of AD depend on the severity of the flare. For mild-moderate flares, AD can often be treated with TCs, topical calcineurin inhibitors (TCIs), or phosphodiesterase-4 (PDE4) inhibitor. It is important to note that there is low risk of adverse side effects when TCs are used appropriately. Interestingly, the harm due to undertreatment of AD is greater than the potential for adverse side effects from TCs.12
Moderate-to-severe AD is often treated with systemic immunomodulators and/or phototherapy. These immunomodulators include systemic corticosteroids, cyclosporine A, methotrexate, azathioprine, and mycophenolate mofetil. The International Eczema Council (IEC) advises against the use of systemic corticosteroids for routine management of AD. Use of systemic corticosteroids should be limited for certain circumstances, such as treatment of an acute flare in need of immediate relief.12 Dupilumab, a monoclonal antibody that blocks interleukin (IL)-4 and IL-13, is the only approved biologic drug for inadequately controlled moderate-severe AD. A recent study examining the efficacy of dupilumab among various racial subgroups (i.e., White, Asian, Black/African Americans) showed that it is effective in improving AD signs, symptoms, and quality of life (QOL) irrespective of race.13
Patients with AD often report a lower QOL than patients who have other chronic illnesses, such as heart disease, diabetes, or hypertension. This decreased QOL is even greater in those who suffer with moderate-to-severe AD.13 When choosing treatment options for patients with AD, it is important to keep in mind that AA populations have a more severe disease course than EA. Therefore, AA patients might require more aggressive early management to minimize disease burden.
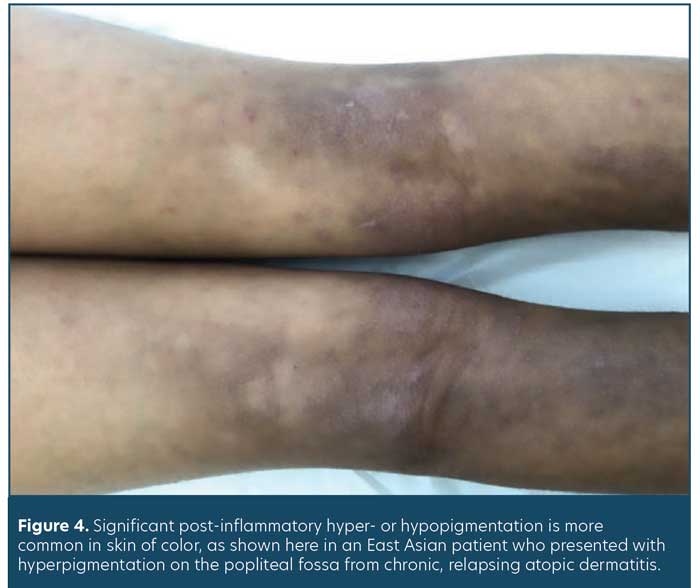
Another nuance when treating skin of color is to understand the impact of post-inflammatory pigmentary changes. Often when AD skin lesions resolve, they can either leave post-inflammatory hyper- or hypo-pigmentation (PIH) (Figure 4). This dyspigmentation can be as equally bothersome to patients as their active AD lesions. When choosing treatments, it is important to educate patients on potential side effects (e.g., hypopigmentation with chronic and/or inappropriate TCI use) and to also develop a plan to manage PIH should it occur.
Summary
In summary, AD is the most common chronic inflammatory skin disease. Its clinical presentation varies based on skin color and racial subgroup. Asian patients often present with psoriasiform features. While treatment and management goals remain the same, AA patients may require earlier and more aggressive treatment due to their propensity for greater disease severity than EA patients. Further research is needed to learn how AD impacts other racial subgroups.
References
- Fu T, Keiser E, Linos E, et al. Eczema and sensitization to common allergens in the United States: a multiethnic, population-based study. Pediatr Dermatol. 2013;31(1):21–26.
- Poladian K, De Souza B, McMichael AJ. Atopic dermatitis in adolescents with skin of color. Cutis. 2019;104(3):164–168.
- Brunner P, Guttman-Yassky E. Racial differences in atopic dermatitis. Ann Allergy Asthma Immunol. 2019;122(5):449–455.
- Sanyal RD, Pavel AB, Glickman J, et al. Atopic dermatitis in African American patients is TH2/TH22-skewed with TH1/TH17 attenuation. Ann Allergy Asthma Immunol. 2019;122(1):99–110.e6.
- Noda S, Suárez-Fariñas M, Ungar B, et al. The Asian atopic dermatitis phenotype combines features of atopic dermatitis and psoriasis with increased TH17 polarization. J Allergy Clin Immunol.
2015;136(5):1254–1264. - Lopez Carrera YI, Al Hammadi A, Huang YH, et al. Epidemiology, diagnosis, and treatment of atopic dermatitis in the developing countries of Asia, Africa, Latin America, and the Middle East: a review. Dermatol Ther (Heidelb).2019;9:685–705.
- Kaufman, BP, Guttman-Yassky, E, Alexis, AF. Atopic dermatitis in diverse racial and ethnic groups—Variations in epidemiology, genetics, clinical presentation and treatment. Exp Dermatol. 2018;27:340–357.
- Kim BE, Leung DYM. Significance of skin barrier dysfunction in atopic aermatitis. Allergy Asthma Immunol Res. 2018;10(3):207–215.
- Correa MCM, Nebus J. Management of patients with atopic dermatitis: the role of emollient therapy. Dermatol Res Pract. 2012;2012:e836931.
- Eichenfield LF, Tom WL, Berger TG, et al. Guidelines of care for the management of atopic dermatitis: section 2. Management and treatment of atopic dermatitis with topical therapies.
J Am Acad Dermatol. 2014;71(1):116–132. - Drucker AM, Eyerich K, de Bruin-Weller MS, et al. Use of systemic corticosteroids for atopic dermatitis: International Eczema Council consensus statement. Br J Dermatol. 2018;178(3):768–775.
- Alexis AF, Rendon M, Silverberg JI, et al. Efficacy of dupilumab in different racial subgroups of adults with moderate-to-severe atopic dermatitis in three randomized, placebo-controlled phase 3 trials. J Drugs Dermatol.
2019 Aug 1;18(8):804–813. - Silverberg J, Gelfand J, Margolis D, et al. Patient burden and quality of life in atopic dermatitis in US adults. Ann Allergy Asthma Immunol. 2018 Sep;121(3):340–347.
