 J Clin Aesthet Dermatol. 2019;12(4):28–30
J Clin Aesthet Dermatol. 2019;12(4):28–30
by Charlene Lam, MD, MPH; Caitlyn Fuller, BA; Alexandra Flamm, MD; and Elizabeth M. Billingsley, MD
All authors are with Penn State Hershey Medical Center in Hershey, Pennsylvania.
FUNDING: No funding was received for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Nonmelanoma skin cancers, typically induced by ultraviolet light, are rarely found on the palmar aspects of the hands. Here, we describe a case of a basal cell carcinoma (BCC) and squamous cell carcinoma (SCC) collision tumor on the palm of a 71-year-old woman. A brief review of literature regarding basal cell carcinoma of the palm and hand are provided, including etiology, diagnosis, and treatment recommendations.
KEYWORDS: Collision tumor, basal cell carcinoma, squamous cell carcinoma, Mohs
Nonmelanoma skin cancers (NMSCs) are typically induced by ultraviolet light and usually involve sun-exposed areas of the body. They are rarely found on palmar aspects of the hands. We present a case of two distinct NMSCs, basal cell carcinoma (BCC) and squamous cell carcinoma (SCC), that presented as a single collision tumor on the palm of an elderly woman. An individual presenting with a BCC and SCC of the palm concurrently is rare, and, to our knowledge, a collision tumor of both entities in this area has not previously been described in the literature.
Case Presentation
A 71-year-old woman presented for Mohs micrographic surgery (MMS) for a biopsy-proven SCC in situ on her left palm. The lesion was present for five years and had become irritated from use of her walker. She had no prior surgical treatment of the lesion. The lesion was initially misdiagnosed as dermatitis and treated with topical corticosteroids. Examination of the left palm demonstrated a 2.7cm × 2.6cm, well-demarcated, erythematous, ulcerated plaque (Figure 1). The patient had no history of skin cancer, arsenic exposure, burn to the area, or ionizing radiation exposure.

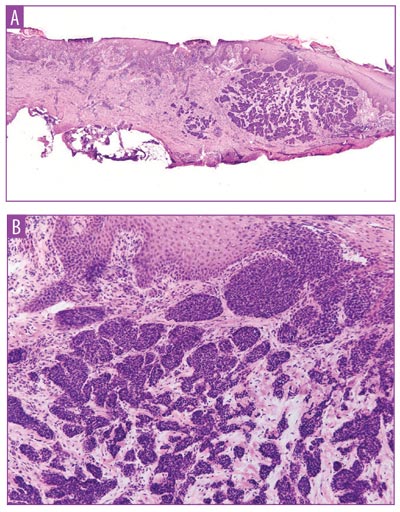
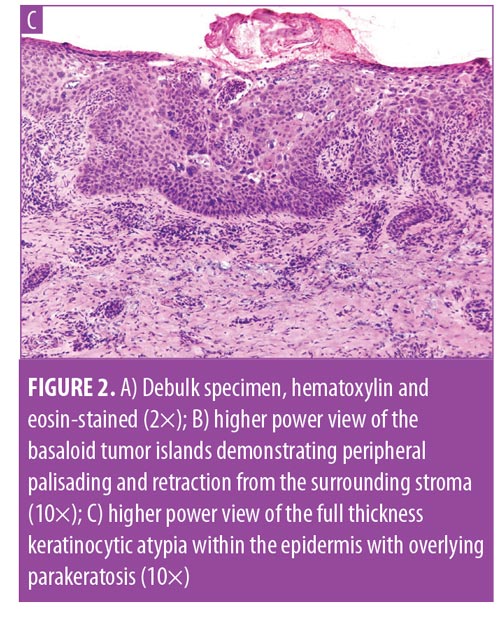
The initial biopsy revealed an area of acanthosis with keratinocyte atypia involving the full-thickness of the epidermis with overlying parakeratosis. A tumor debulk was taken during MMS. The frozen histology revealed similar findings of acanthosis with keratinocyte atypia involving the full-thickness epidermis with overlying parakeratosis (Figure 2). Separately, the dermis showed basaloid islands with peripheral palisading and stromal retraction (Figure 2c). These findings were consistent with that of a collision tumor consisting of a SCC in situ and a BCC. Clear surgical margins were obtained, and the defect was repaired with a full-thickness skin graft.
Discussion
Pathogenesis. BCCs on the palm, while rare, occur relatively more often in patients with basal cell nevus syndrome (BCNS). BCNS is inherited as an autosomal dominant trait that results in an upregulation of cell proliferation and presents with multiple BCCs over the patient’s lifetime.1 One report describes a case of recurrent BCC of the palm in a 55-year-old woman with a prior diagnosis of BCNS.2 Additionally, this patient had multiple BCCs removed from her scalp, face, neck, and trunk. Several other factors can predispose BCC development on the palm, including harmful chemical exposure (arsenic), ionizing radiation, or other hereditary syndromes, such as xeroderma pigmentosum.3
Factors responsible for the anatomic distribution of BCC are unknown, but typically, sun-exposed sites are more prone to BCC development. Up to one third of BCC cases, however, occur in sun-protected areas.4 A study by Graham and McGavran5 found the incidence of BCC on sun-exposed skin to be directly proportional to the sebaceous gland-density of the area. This might explain why these cancers are more rarely found in nonglaborous regions, such as the palm. Mleczko et al6 postulated that palmar BCCs originate from progenitor cells of eccrine glands. Based on this theory, the high density of eccrine glands on the palm might actually predispose to BCC formation in this area.
Because of its rarity, SCC of the palm might frequently be misdiagnosed, as was the case in our patient. In one case report, an SCC on the palm was described as a nonhealing ulcerated lesion in an area of previous trauma with positive axillary lymphadenopathy.7 Risk factors for palmar SCCs include arsenic ingestion, genetic syndromes, immunosuppression, viral infection, local radiation exposure, trauma, and chronic ulcers.8
It is not entirely uncommon for a BCC to develop alongside another cutaneous neoplasm. The most commonly reported combination of skin tumors is that of BCC and a melanocytic nevus.9 Cutaneous collision tumors are defined as two independent tumors that are anatomically close, yet separated from one another by a well-defined boundary.10 Various hypotheses exist regarding the pathophysiology behind collision tumor formation. Some theorize it to be purely coincidental, while others postulate that it might be the result of paracrine effects of one tumor influencing growth of nearby cell populations.11,12 In our case, the collision between the tumors did not appear to have an impact on the course of each neoplasm, as they continued to behave independently.13
Diagnosis. Collision tumors between BCC and SCC are not to be confused with basosquamous carcinoma (BSCC), characterized by aggressive growth.9 BSCC, also known as metatypical carcinoma, has the histological characteristics of both BCC and SCC within the tumor. The increased local aggressiveness associated with BSCC is hypothesized to be caused by the totipotent cells in BCC that are responsible for the squamous differentiation.14 In a study examining staining patterns of BSCC, investigators found distinct transition zones within the lesion, suggestive of its own neoplastic properties as opposed to simply being a collision tumor.15 True collision tumors do not display a gradual transition zone and instead present a tumor-free zone between the two neoplasms on pathology, as seen in this case.12
Treatment recommendations. Treatment of these neoplasms is usually driven by tumor type, size, location, and depth of the tumor.9 Low-risk cutaneous lesions can be managed with cryotherapy, electrosurgery, topical treatment, or surgical excision.8,16 Cryotherapy can be used in cases of low-risk, well-defined tumors as it is fast and cost-effective, but this method does not allow for the histologic confirmation of tumor margins.16 Electrodissection and curettage destruction is also time-efficient and well-tolerated, but similarly does not allow for the histological confirmation of tumor margins.16 Topical 5-fluorouracil and imiquimod are approved by the United States Food and Drug Administration (FDA) as treatment options for superficial lesions and can provide superior cosmetic outcomes when compared with surgical options; however, results are dependent on patient adherence with multiple treatments over a long term of time.3,17 Standard wide, local excision is also an option with histologic margin confirmation; however, it can be more debilitating, compared to tissue sparing MMS, as more tissue is removed and positive margins will necessitate additional surgery.16 Radiation is also a treatment option for nonsurgical candidates; however, radiation often requires multiple treatments and can have acute and chronic side effects.16 Our patient’s tumor was treated with MMS for margin control and tissue sparing, given its location. Prognosis of these patients is favorable, but routine follow-up should be performed.
Conclusion
Concurrent but separate BCC and SCC of the palm is a rare diagnosis. BCC and SCC as a collision tumor in this area has not previously been described in the literature. While keratinocytic malignancies are uncommon on the palm, it is important to biopsy any suspicious lesion to prevent diagnostic delay. In our case, there was an absence of known risk factors. When diagnostic biopsy is unclear, patient history and clinical impression should be carefully considered to avoid misdiagnosis and delay in treatment. This type of lesion has been successfully treated with a variety of approaches, including cryotherapy, electrosurgery, topical treatment, and surgical treatment. The clinician should carefully consider tumor type, size, location, and depth before deciding on a treatment method. MMS allows for histologic confirmation, better control of margins, and minimal involvement of healthy tissue, compared with other treatment options, and was successfully used in our patient. The prognosis of these patients is largely favorable with complete excision.
References
- Crowson AN. Basal cell carcinoma: biology, morphology and clinical implications. Mod Pathol. 2006;19 Suppl 2:S127–S147.
- Taylor WB. Nevoid basal cell carcinoma of the palm. Arch Dermatol. 1970;102(6):654–655.
- Lateo S, Charlton FG, Ormond P. A palmar injury that failed to heal diagnosis: basal cell carcinoma of the palm. Clin Exp Dermatol. 2006;31(5): 731–732.
- West JR, Berman B. Basal cell carcinoma presenting as a chronic finger ulcer. J Am Acad Dermatol. 1990;23(2 Pt 1):318–319.
- Graham PG, McGavran MH. Basal cell carcinoma and sebaceous glands. Cancer. 1964;17:803–806.
- Mleczko A, Franke I, Pokrywka A, et al. BerEP4- negative basal cell carcinoma on the palm: case report and review of the literature. J Dtsch Dermatol Ges. 2011;9(2):140–143.
- Gonzalez-Sosa D, Beatriz BG, Couto-Gonzalez I, et al. Moderately differentiated squamous cell carcinoma of the palm: an extremely infrequent tumour. BMJ Case Reports. 2014 Oct 14. pii: bcr2014206350.
- Cohen PR, Jiang SB. Finger pad squamous cell carcinoma: report of squamous cell carcinoma of the distal palmar digit and review of associated risk factors, mimickers, and treatment of squamous cell carcinoma of ventral hand digits. J Clin Aesthet Dermatol. 2017;10(8):42–48.
- Medeiros PM, da Silva CC, Barcaui CB, et al. Collision of malignant neoplasms of the skin: basosquamous cell carcinoma associated with melanoma. An Bras Dermatol. 2015;90(3 Suppl 1):39–42.
- Ayva SK, Tepeoglu M, Gunduz O, et al. A case of two synchronous cutaneous collision tumors. Gazi Med J. 2017;28(2):127–128.
- Papa G, Grandi G, Pascone M. Collision tumor of malignant skin cancers: a case of melanoma in basal cell carcinoma. Pathol Res Pract. 2006;202(9):691–694.
- Boyd AS, Rapini RP. Cutaneous collision tumors: an analysis of 69 cases and review of the literature. Am J Dermatopathol. 1994;16(3):253–257.
- Piérard GE, Fazaa B, Henry F, et al. Collision of primary malignant neoplasms on the skin: the connection between malignant melanoma and basal cell carcinoma. Dermatology. 1997;194(4):378–379.
- Credid HM, Menezes AS, Aikaiwa KF, et al. Tumor de colisão de pele do pescoço. Rev Col Bras Cir. 2011;38:66–70.
- Jones MS, Helm KF, Maloney ME. The immunohistochemical characteristics of the basosquamous cell carcinoma. Dermatol Surg. 1997;23(3):181–184.
- Mendez BM, Thornton JF. Current basal and squamous cell skin cancer management. Plast Recon Surg. 2018;142(3):373e–387e.
- Salomao P, Kopke LF, MacHado-Pinto J. Palmar basal cell carincinoma: case report and literature review. Dermatol Surg. 1999; 25(11):908–910.

