 by Hamzah Mustak, MD; Michael Rafaelof, BS; Robert Alan Goldberg, MD; and Daniel Rootman, MD
by Hamzah Mustak, MD; Michael Rafaelof, BS; Robert Alan Goldberg, MD; and Daniel Rootman, MD
Drs. Mustak, Goldberg, and Rootman and Mr. Rafaelof are with the Stein Eye Institute, Division of Orbital and Oculoplastic Surgery at the University of California, Los Angeles in Los Angeles, California. Dr. Mustak is also with the Groote Schuur Hospital, Division of Ophthalmology, University of Cape Town in Cape Town, South Africa.
Funding: No funding was provided for this article.
Disclosures: The authors have no conflicts of interest relevant to the content of this article.
Abstract: Background: Lid margin asymmetry and its associated compensatory mechanisms might cause patients to seek treatment to improve aesthetics. Surgery might not be indicated and can potentially worsen the asymmetry in these cases. Methods: A case series of three patients was organized to illustrate the use of botulinum toxin administered to the pre-tarsal orbicularis for the correction of micro-ptosis and improved symmetry. The marginal reflex distance and tarsal platform show were measured on both sides. Measurements were made using ImageJ software on standardized frontal photographs taken pre- and post-injection. Results: The average increase in the marginal reflex distance was 0.914mm, with an average pre-tarsal botulinum toxin dose of three units. The average change in tarsal platform show between the two eyes was 0.89mm. Conclusion: Botulinum toxin application to the pre-tarsal orbicularis oculi muscle might be a suitable option for the management of small eyelid margin asymmetries.
Keywords: Botulinum toxin, ptosis, eyelid asymmetry
J Clin Aesthet Dermatol. 2018;11(4):49–51
Although eyelid ptosis has various positional definitions, it is often defined as a margin reflex distance (MRD) below 2.5mm or an asymmetry of more than 1mm between the two eyes.1 There are, however, grades of ptosis ranging from severe (with obstruction of the pupil) to mild with barely noticeable asymmetries. Near the mild end of the spectrum, micro-ptosis and the accompanying compensatory mechanisms (e.g., recruitment of the frontalis muscle in an effort to elevate the ptotic eyelid can in turn lead to asymmetry of the eyebrows) often result in aesthetic asymmetry) might motivate patients to seek treatment.
Facial symmetry is particularly obvious in the periorbital region, and even mild ptosis can heighten the perception of facial asymmetry.2 In patients with such mild or micro-ptosis, surgery is rarely indicated from a functional perspective and can lead to secondary aesthetic complications, such as contour asymmetry or crease abnormalities.2 Nonsurgical treatments might be desirable in these situations. One such treatment is botulinum neurotoxin.3 Through our review of three cases, we describe the use of pre-tarsal botulinum toxin injections to elevate the lid margin height in patients with mild ptosis.
Methods
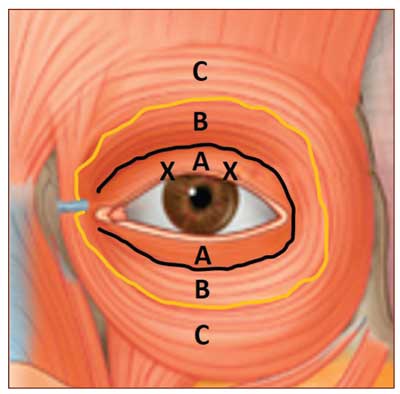
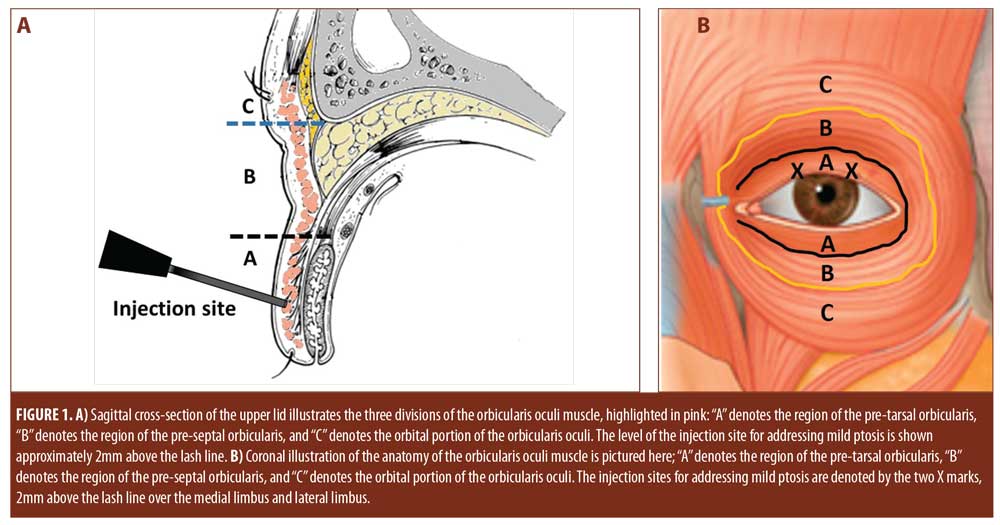
In this small case series, we review three patients with mild ptosis. The patients received pre-tarsal botulinum toxin injections via a transdermal approach. Botulinum toxin (diluted 1u/0.02cc, using a 1.0cc insulin syringe on a 30-gauge needle) was injected transdermally 2mm above the lash line in the medial and lateral third of the pre-tarsal orbicularis (Figure 1).
Ptosis was evaluated by measuring MRD values before and several weeks (6–11 weeks) after the injection to assess improvement. Tarsal platform show was also measured in both eyes to assess symmetry. Measurements were made using ImageJ software (a public domain, Java-based, image-processing software program developed by the National Institutes of Health) on frontal photographs perpendicular to the camera plane with standard lighting. The central corneal diameter was used as a reference for measurements based on the normal values of 11.77 for men and 11.64 for women.4 The efficacy of the treatment was defined by improvement in ptosis to less than a 0.5mm difference in MRD between the two eyes, as well as a reduction in the difference between the tarsal platform show.
Informed consent and photoconsent was received from the patients.
Results
The average increase in MRD was 0.914mm, with an average pre-tarsal botulinum toxin dose of three units. The average change in TPS between the two eyes was 0.89mm.
Case 1. A 38-year-old man presented with a history of congenital ptosis of the left eye. This patient had two previous surgeries to repair ptosis, with the most recent one being eight years previously, with recurrence after both procedures (Figure 2, A1). Botulinum toxin was administered (Figure 2, A2), including two units injected into the pre-tarsal orbicularis of the left eye. On examination six weeks after the botulinum toxin injection, MRD had increased in the left eye by 0.993mm. The tarsal platform show difference also decreased by 0.149mm (Figure 2, A3).
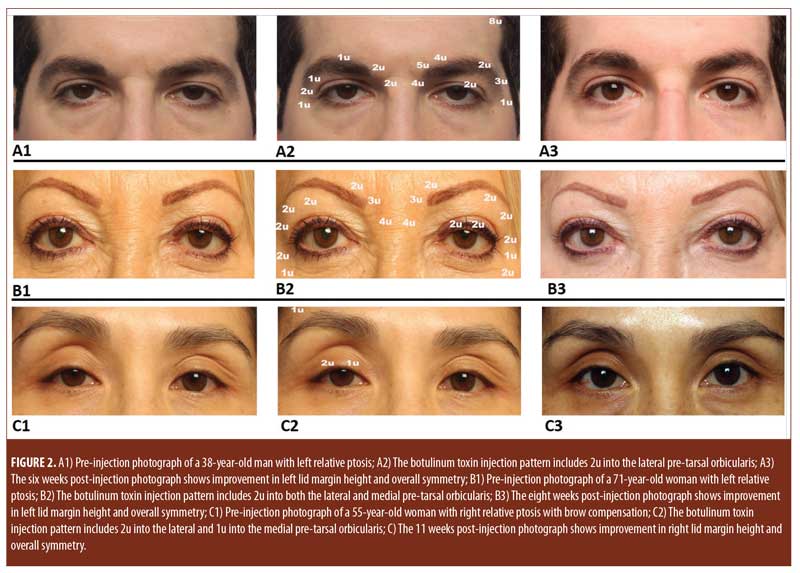
Case 2. A 71-year-old woman with a history of thyroid-associated orbitopathy presented with left-sided ptosis appearing greater than right-sided ptosis. On examination, the left MRD was 1.85mm (Figure 2, B1) compared to a right MRD of 2.77mm. Botulinum toxin was injected (Figure 2, B2), including two units injected into the lateral and medial pre-tarsal orbicularis of the left eye. Eight weeks after the botulinum toxin injection, MRD had increased in the left eye by 0.919mm (Figure 1, B3).
Case 3. A 55-year-old woman presented with right-sided ptosis (Figure 2, C1). Botulinum toxin was injected (Figure 2, C2), including two units to the lateral and one unit to the medial right pre-tarsal orbicularis, as well as one unit to the right frontalis. Eleven weeks after the botulinum toxin injection, MRD had increased in the left eye by 0.83mm and the size of the palpebral fissure had increased by 1.048mm. The tarsal platform show difference also had decreased by 2.044mm (Figure 2, C3).
Discussion
Botulinum toxins are neuromuscular-blocking agents produced by the bacteria Clostridium botulinum. They weaken targeted muscles by inhibiting the release of acetylcholine from the presynaptic terminal of the neuromuscular junction.3 In this small case series, we found that neurotoxin application to the pre-tarsal orbicularis was effective in raising eyelid position and decreasing TPS asymmetry.
The orbicularis oculi muscle is divided into three segments: pre-tarsal, pre-septal, and orbital (Figure 1).5 Anatomic studies have shown that each segment of the muscle plays a specific role in eyelid physiology.5 The orbital portion is involved in forceful and sustained closure, the pre-septal portion closes the eyelid during a blink, and the pre-tarsal orbicularis is postulated to play a role in lid margin tone.5
Ptosis pathophysiology is complex and cannot be perfectly explained by a simple model of discordance between the eyelid protractors and retractors. The botulinum toxin injections are hypothesized to work by weakening the pre-tarsal orbicularis selectively, tending toward a balance of force favoring retraction. This would be similar to the eyelid position dysregulation found in patients with facial nerve palsy.6
While the MRD improvements provided patients with substantial aesthetic enhancements, the effectiveness of botulinum toxin for functional ptosis is still uncertain. Our case series shows just under 1mm of improvement. More severe ptosis might not respond to botulinum toxin in such a fashion and thus requires further study. The effects of botulinum toxins tend to be dose-dependent.7 As such, injecting increased doses of botulinum toxins into the pre-tarsal orbicularis could potentially yield greater improvements in MRD. However, larger doses could induce other complications, including lagopthalmos, exposure keratitis, and even worsening ptosis if the toxin diffuses to the Mueller/levator complex.
Addressing periorbital asymmetry with botulinum toxins must be tailored to each patient, and involves the treatment of several areas, requiring a targeted approach with a thorough understanding of the muscles involved. Treatment in this region commonly involves addressing the protractor muscles aimed at elevating the brow. An argument can be made that the elevation of the brow might also play a role in the upper lid margin position. The results from Case 3 might provide some evidence for the role of specifically targeting the pre-tarsal orbicularis. In this case, botulinum toxin was administered to the right frontalis region in order to drop the right eyebrow. Intuitively, a drop in the brow should lower the ptotic lid further; however, we saw an improvement in the lid margin position, presumably from the pre-tarsal botulinum toxin treatment.
One adverse effect of botulinum toxin application is the inadvertent induction of ptosis, which occurs at a rate of approximately 0.5 to 1 percent.8 Inadvertent induction of ptosis can be mitigated by careful injection of the toxin in a standardized location; however, there is no way to completely eliminate the risk.3 Patients should be counseled regarding this.
Conclusion
In patients with mild or micro-ptosis, corrective surgery might not be indicated but cosmetic improvement might be desired. In such cases, botulinum toxin application to the pre-tarsal orbicularis oculi muscle might be a suitable option for the management of small eyelid margin asymmetries.
References
- Ahmad K, Wright M, Lueck CJ. Ptosis. Pract Neurol. 2011;11(6):332–340.
- Lew H, Goldberg R. Maximizing symmetry in upper blepharoplasty: the role of microptosis surgery. Plast Reconstr Surg. 2016;137(2):296e–304e.
- Fagien S. Temporary management of upper lid ptosis, lid malposition, and eyelid fissure asymmetry with botulinum toxin type A. Plast Reconstr Surg. 2004;114(7):1892–1902.
- Rufer F, Schroder A, Erb C. White-to-white corneal diameter: normal values in healthy humans obtained with the orbscan ii topography system. Cornea. 2005;24(3):259–261.
- Lander T, Wirtschafer J, McLoon L. Orbicularis oculi muscle fibers are relatively short and heterogeneous in length. Invest Ophthalmol Vis Sci.1996;37(9):1732–1739.
- Sinha KR, Rootman DB, Azizzadeh B, Goldberg RA. Association of eyelid position and facial nerve palsy with unresolved weakness. JAMA Facial Plast Surg. 2016;18(5):379–384.
- Francisco GE. Botulinum toxin: dosing and dilution. Am J Phys Med Rehabil. 2004;83(10 Suppl):S30–S37.
- Chen AH, Frankel AS. Altering brow contour with botulinum toxin. Facial Plast Surg Clin North Am. 2003;11(4):457–464.

