J Clin Aesthet Dermatol. 2025;18(8):18–19.
by Kabir Al-Tariq, MS; Rama Abdin, BS; and Naiem T. Issa, MD, PhD
Mr. Al-Tariq is with the Georgetown University School of Medicine in Washington, District of Columbia. Ms. Abdin is with the Charles E. Schmidt College of Medicine at Florida Atlantic University in Boca Raton, Florida. Dr. Issa is with Forefront Dermatology in Vienna, Virginia, Issa Research and Consulting, LLC, in Springfield, Virginia, the Dr. Phillip Frost Department of Dermatology at the University of Miami Miller School of Medicine in Miami, Florida, and the George Washington University School of Medicine and Health Sciences in Washington, District of Columbia.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors declare no conflicts of interest relevant to the content of this article.
Abstract: Basal cell carcinoma (BCC) is the most common skin cancer in the United States. Common treatment approaches for superficial, small, and/or low grade BCCs include topical therapy or curettage plus electrodesiccation and cryotherapy. For larger, high-grade, and/or certain subtypes of BCC, surgical therapy is typically pursued, occasionally under anesthesia for large lesions. While surgical therapy provides good clearance rates, it is not feasible for all patients. Therefore, it is important for physicians to understand alternative, less invasive approaches to treating BCC in order to provide patients with the best possible evidence-based care. In this case, we describe a combination topical treatment approach for a large nodular BCC in an elderly patient in a tough to excise inguinal region. Keywords: Nodular basal cell carcinoma, combination topical therapy
Introduction
Basal cell carcinoma (BCC) is the most common skin cancer in the United States with an estimated incidence of 3.6 million cases annually.1 BCCs, which are derived from epidermal keratinocytes, are typically indolent in growth and progression, and are unlikely to metastasize. Classically, BCCs present as pearly pink papules localized to sun-damaged regions of the skin; however, the presentation can vary from patient to patient (ie, pink patches).1 Depending on the location and grade of the BCC, treatment typically involves either topical therapy for more superficial cancers or surgical excision for higher grade BCCs or BCCs in sensitive areas such as the face.2 Additionally, topical treatments may be preferred for patients who are not suitable surgical candidates despite having more aggressive BCCs.2 Currently, the only two topical therapies with a complete consensus and a grade “A” recommendation for the treatment of superficial BCC (sBCC) are 5% imiquimod and 5% 5-fluorouracil (5-FU), based on multidisciplinary expert opinion from the European Dermatology Forum, the European Association of Dermato-Oncology, and the European Organization of Research and Treatment of Cancer.2,3 With 5-FU, clearance rates are reportedly 90 to 93 percent for superficial BCCs (sBCC) and more varied for nodular BCCs (nBCC), ranging from 48 to 85 percent.3 With imiquimod, clearance rates for sBCCS and nBCCs are varied, and can range from 53 to 76 percent, depending on the regimen applied.3 Another nonsurgical option for the treatment of small or multiple BCCs on extrafacial areas is curettage plus electrodesiccation and cryotherapy; however, this approach has a Grade “B” recommendation.2 Photodynamic therapy (PDT), with photosensitizers methyl aminolevulinate (MAL) or 5-aminolevulinic acid (ALA), has also been investigated for the treatment of nBCC given the better cosmesis with outcomes compared to surgery.
Here we present a unique case of nodular BCC in the right inguinal region where surgical management was initially indicated, but due to need for general anesthesia and surgical grafting given the size and location, the patient opted for treatment with cryotherapy followed by 5-FU and topical imiquimod. The patient provided informed consent and photoconsent.
Case Description
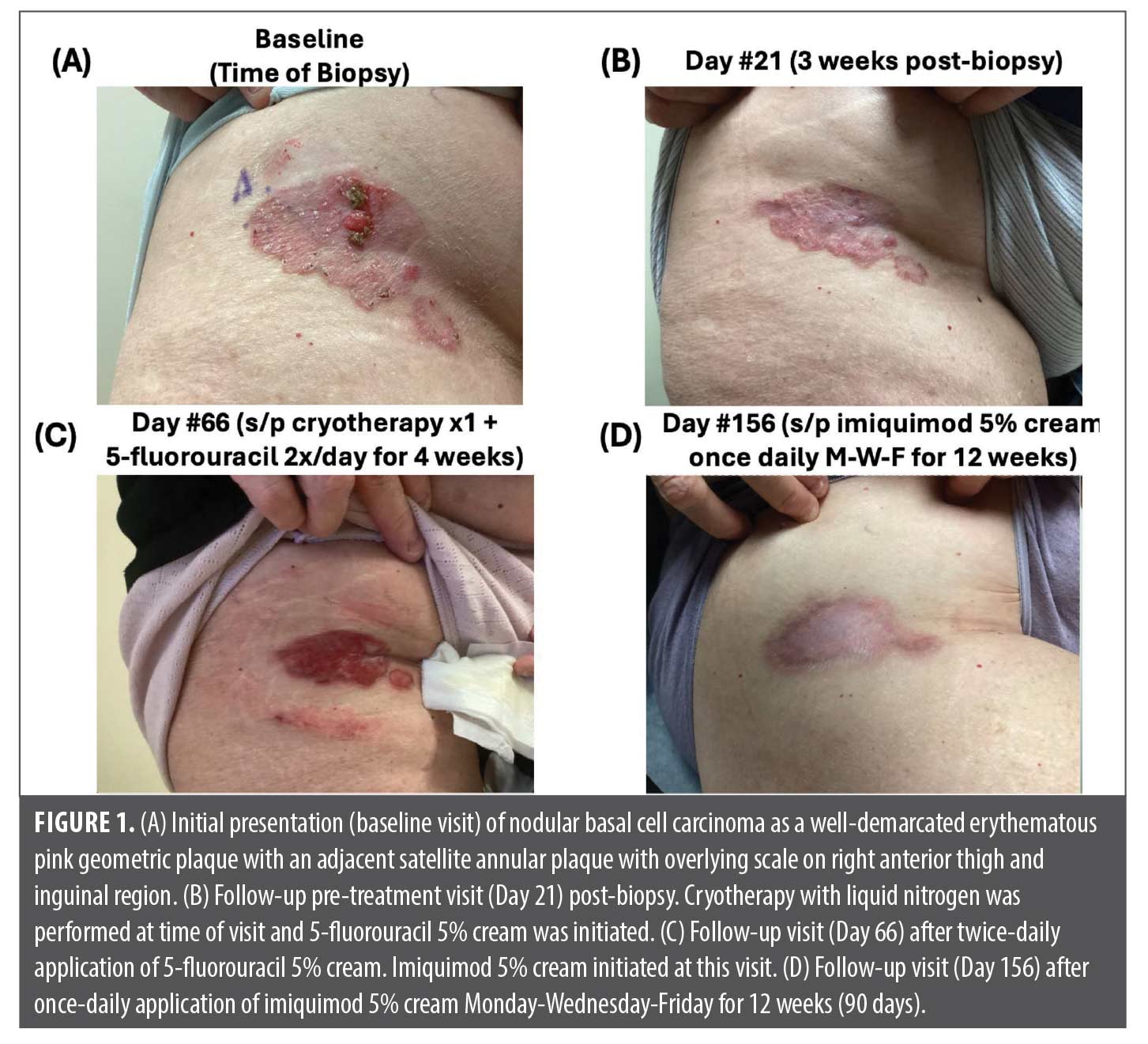
A 72-year-old White woman with unremarkable past medical history presented with a pruritic and painful lesion on her right anterior thigh that extended into the inguinal area. Examination revealed a 3.5 x 2.0cm, well-demarcated, pink geometric plaque with a palpable pink nodule medially, and a medially adjacent satellite arcuate pink plaque. Both lesions had an overlying thin white scale with discrete eroded areas (Figure 1A). Tangential shave biopsies of the lateral edge, medial nodular component, and medial satellite lesion revealed a histopathologic diagnosis of nodular basal cell carcinoma. Given the lesion’s large size, location in a high-movement area, and the patient’s reduced skin elasticity and body habitus, primary closure was deemed difficult due to the risk of excessive tension, wound dehiscence, and infection. Additionally, the patient’s preference for optimal cosmesis and preserved functionality indicated a need for grafting to provide a more natural appearance at the surgical site and mitigate the risk of contracture formation. Thus, the patient elected for a non-invasive treatment with local destruction and topical therapeutics.
The patient was treated with one session of liquid nitrogen cryotherapy (two freeze cycles of 60 seconds with a thawing interval of 90 seconds) and was started on 5% 5-FU twice daily for four weeks (Day 21, Figure 1B). At follow-up (Day 66), there was appreciable inflammation due to 5-FU treatment (Figure 1C). She was then started on topical imiquimod 5% cream applied three times a week for 12 weeks. After 12 weeks of treatment with imiquimod (Day 156), the lesion regressed to a flat, shiny white scar without clinical evidence of active malignancy, as indicated by the resolution of ulceration and pearly rolled borders (Figure 1D). Additionally, dermoscopy revealed no concerning features such as arborizing telangiectasias, a milky red background, or blue ovoid nests. The patient also opted not to undergo re-biopsy for histopathologic confirmation of malignancy resolution.
Discussion
This case represents the successful treatment of nodular BCC with combination topical therapy that otherwise required surgical intervention.2 Reported clearance rates of nBCC with 5-FU and imiquimod range from approximately 48 to 85 percent and 53 to 75 percent, respectively; however, complete clearance rates have also been reported, depending on the regimen used.3 The use of combination therapy with 5-FU and imiquimod leverages their unique mechanisms of action to facilitate the destruction of neoplastic cells via inhibition of cell growth and stimulation of the local immune system, respectively. On the other hand, cryotherapy is able to destroy neoplastic cells via local interruption of metabolic cycles, destabilization of cell membranes, and release of local tumor antigens that lead to an enhanced immune response.6 Therefore, the rationale and benefit behind using combination topical therapy is to target tumor cells through different mechanisms, enhancing the overall efficacy.
The use of topical combination therapy for both sBCCs and nBCCs has been previously documented in a case series investigating combination 5% imiquimod, 2% 5-FU solution, and tretinoin 0.1% cream five times a week for six weeks.7 Of the malignancies that were treated with this combination topical therapy, the largest documented neoplasm was a 15mm sBCC on the right forearm. Thus, these patients likely would not have required surgical excision and grafting in the operating room.4 A different study investigating the efficacy of treating imiquimod-resistant BCC with cryotherapy followed by imiquimod achieved resolution in 83 percent of cases.3 While this study was able to demonstrate the utility of combining cryotherapy and imiquimod, the lesions ranged from 1 to 2cm in diameter and therefore were unlikely to require surgical intervention under general anesthesia, unlike the case presented here.3 This case is unique as topical therapy was successfully used to treat a large nodular BCC of the anterior thigh and groin, allowing the patient to avoid surgery and its associated complications. Topical therapy may be a viable alternative to surgery for certain nodular BCCs, particularly for patients at higher risk for surgical complications. This approach could reduce the need for invasive procedures, minimize recovery time, and avoid the risks associated with general anesthesia and surgery.
References
- Tan IJ, Pathak GN, Silver FH. Topical Treatments for Basal Cell Carcinoma and Actinic Keratosis in the United States. Cancers. 2023;15(15):3927.
- Peris K, Fargnoli MC, Garbe C, et al. Diagnosis and treatment of basal cell carcinoma: European consensus-based interdisciplinary guidelines. Eur J Cancer. 2019;118:10–34.
- Algarin YA, Jambusaria-Pahlajani A, Ruiz E, Patel VA. Advances in Topical Treatments of Cutaneous Malignancies. Am J Clin Dermatol. 2023;24(1):69–80.
- Koumprentziotis IA, Rompoti N, Liopyris K, et al. Photodynamic Therapy for the Treatment of Basal Cell Carcinoma: A Comprehensive Review of Randomized Controlled Trials. Dermatol Pract Concept. 2024;14(2):e2024105.
- Hernandez LE, Mohsin N, Levin N, et al. Basal cell carcinoma: An updated review of pathogenesis and treatment options. Dermatol Ther. 2022;35(6):e15501.
- Messeguer F, Serra-Guillen C, Echeverria B, et al. A pilot study of clinical efficacy of imiquimod and cryotherapy for the treatment of basal cell carcinoma with incomplete response to imiquimod. J Eur Acad Dermatol Venereol. 2012;26(7):879–881.
- Nahm WJ, Badiavas EV, Kirsner RS, et al. Treating keratinocyte carcinomas with a combination of imiquimod, 5-fluorouracil, and tretinoin using store-and-forward telemedicine in the age of coronavirus disease 2019 to promote social distancing. JAAD Case Rep. 2020;6(9):931–934.
