J Clin Aesthet Dermatol. 2020;13(1):37–37
 by Marcella Leal Novello D’Elia, MD; Kelly K. Park, MD, MSL; and Eduardo Weiss, MD
by Marcella Leal Novello D’Elia, MD; Kelly K. Park, MD, MSL; and Eduardo Weiss, MD
Dr. D’Elia is with the Department of Dermatology at Pedro Ernesto University Hospital (HUPE) of Rio de Janeiro State University (UERJ) in Rio de Janeiro, Brazil. Dr. Park is with Edward Hines, Jr. Veterans Affairs Medical Center in Hines, Illinois and is an Affiliate Faculty Member at Loyola University Stritch School of Medicine. Dr. Weiss is a Clinical Professor of Dermatology and Dermatological Surgery at the Miller School of Medicine at University of Miami in Miami, Florida.
FUNDING: No funding was provided.
DISCLOSURES: The authors report no conflicts of interest related to the content of this article.
ABSTRACT: Acral myxoinflammatory fibroblastic sarcoma (AMFS) represents a low-grade sarcoma with a high rate of local recurrence that commonly affects the distal extremities. The lesion often presents as a painless mass in the hands or feet. There is no formal standardized treatment protocol for this tumor, but wide surgical excision, with or without adjuvant radiation therapy, is the conventional treatment. We report a case of a patient with an AMFS treated with Mohs micrographic surgery (MMS) without recurrence. Because of the propensity of this tumor to involve acral sites where tissue conservation is important, MMS might be an alternative treatment modality for this rare entity.
KEYWORDS: Acral myxoinflammatory fibroblastic sarcoma; Mohs micrographic surgery, radiation
Soft tissue sarcomas represent approximately one percent of all adult malignancies.1 Acral myxoinflammatory fibroblastic sarcoma (AMFS) is an extremely rare form of sarcoma first described in 1998.1,2 Due to the scarcity of these tumors, few surgeons consider AMFS as a differential diagnosis of a painless mass in acral sites. We describe a case of this rare entity that was treated with Mohs micrographic surgery (MMS) without recurrence. MMS has not been deemed conventional therapy in comparison to wide local excision, but adoption of this technique may improve margin control and tissue conservation and should be considered a viable treatment modality.
Case Report
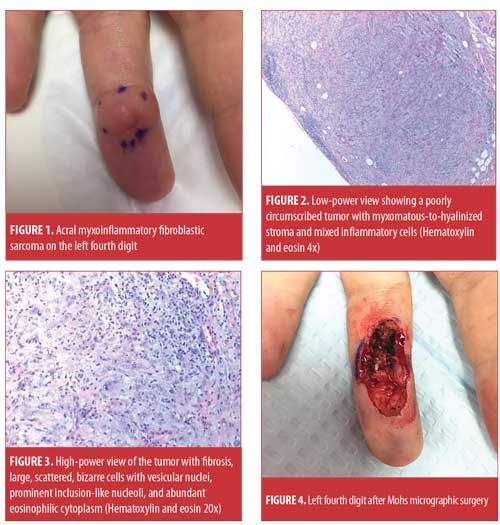
A 42-year-old Caucasian male patient presented with a painless growing tumor that first appeared six months previously on his left fourth finger. The patient was otherwise healthy and denied trauma or previous surgery in the area. Family history was noncontributory. On clinical examination, there was a firm, flesh-colored, subepidermal nodule measuring 1cm on the volar aspect of the left fourth finger (Figure 1). A skin biopsy by punch method was performed and submitted for histopathological evaluation (Figures 2 and 3). This revealed a dermal proliferation of atypical epithelioid cells with large nuclei and prominent nucleoli alone with mixed inflammatory cell infiltrate. A diagnosis of acral myxoinflammatory fibroblastic sarcoma was made. Due to the unusual nature of the tumor and location, the patient underwent Mohs micrographic surgery, with complete clearance of the tumor achieved after six stages (Figure 4). The defect was repaired using a guiding suture technique, and the patient was referred to Radiation Oncology for adjuvant radiation, but declined further treatment. Patient had no evidence of recurrence four months after MMS (Figure 5). In addition, the patient did not report recurrence three years later.
 Discussion
Discussion
AMFS was first described in 1998 by three separate groups of authors and is generally considered a low-grade soft tissue tumor, although 23 high-grade cases have been reported.2 These tumors typically affect middle-aged men and occur on the distal extremities, with a predilection for the fingers and hands in 75 to 80 percent of cases.1,3–5 They have a high propensity for local recurrence (>50%) and a low rate of metastasis.1,3,4
Patients affected by this tumor often present with an indolently growing, painless mass for several months. These tumors have been reported to range in size from 1.5 to 18cm, are generally well-demarcated, and can be lobular, yellowish in color, and occasionally mucoid. Occasionally, areas of necrosis and hemorrhage are found.4
Lesions can be initially misdiagnosed as an infectious or chronic, inflammatory process; primary cutaneous lymphoma, including cutaneous Hodgkin’s disease; or a benign condition, such as a ganglion cyst, giant cell tumor of the tendon sheath, or other benign tumors of the hand. A certain degree of suspicion should be held particularly with recurrence or progression of the tumor.1 Unfortunately, misdiagnosis of AFMS can lead to inappropriate management or delay in treatment, with frequent local recurrences and potential regional and distant metastasis. This can lead to major morbidity, including amputation.1,5
Histopathologically, AMFS is characterized by a multinodular and poorly circumscribed tumor that often invades into adjacent structures, including tendon sheaths, synovial lining, subcutaneous fat, and muscle. There is a dense chronic inflammatory infiltrate with a myxomatous-to-hyalinized background stroma. The myxoid matrix has been described as containing numerous types of inflammatory cells, fibrosis, and large, scattered, bizarre cells with vesicular nuclei, prominent inclusion-like nucleoli, and abundant eosinophilic cytoplasm with features of modified fibroblasts.1 The inflammatory infiltrate typically includes polymorphonuclear leukocytes, lymphocytes, granulocytes, eosinophils, and plasma cells with germinal centers.1 The immunohistochemical phenotype is nonspecific; the tumor cells express vimentin (in all reported cases), CD68 (66%), CD34 (28%), smooth muscle actin (6%) and cytokeratin (KL1) (11%).4 They do not express epithelial membrane antigen, protein S100, desmin, CD15, HMB45, CD45, or Epstein-Barr virus (EBV) latent membrane protein (LMP1).4
We recommend a biopsy to obtain a sufficient tissue, such as a punch biopsy, although an incisional or core needle biopsy was originally recommended.1 Once the tumor is diagnosed, there is no standardized treatment protocol, but wide surgical excision is the conventional treatment.1,5 Mohs micrographic surgery has been used to treat AFMS without recurrence after five years and, depending on the location of the tumor, can be considered a viable treatment.5 Local recurrence ranges from 22 to 67 percent, at a median of 4 to 10 months.4 Tejwani et al3 reported excellent local control with preoperative radiation therapy (RT) in 14 patients with only one recurrence in almost three years of follow-up, and it should be considered adjuvant therapy for AFMS. Perioperative and postoperative RT can also be used as adjuvant treatment in addition to excision.3,5 RT has been reported to have been used preoperatively and intraoperatively in some patients and preoperatively and postoperatively in other patients.3 Radiation can be used for adjuvant therapy after positive surgical margins following resection, recurrent disease, or to avoid amputation.3 Due to difficulties with margin control with AFMS, postoperative radiation can be useful.3 The potential morbidity of surgery and RT should be taken into consideration in the treatment of patients with AMFS.3 However, fibrosis, edema, and joint stiffness can be long-term consequences of radiation therapy on the extremities.6 Due to the propensity of AMFS to involve acral sites, where both tissue conservation and margin control are important, Mohs micrographic surgery followed by RT might be a preferential treatment option.5 In our case, the tumor location and characteristics, including poor differentiation, hampered the feasibility of wide-margin surgical resection; thus, MMS was performed and adjuvant RT was recommended, but declined by the patient. Postoperative tumor surveillance should include a physical examination for the presence of local or regional metastatic disease and a chest radiograph to detect distant metastatic disease. Evaluations should be performed quarterly for the first two years and then every six months for up to five years.5
Conclusion
AMFS is a rare tumor occurring on acral areas. Due to reports of high-grade subtypes and risk of recurrence, Mohs micrographic surgery, with or without adjuvant radiation, might be a viable treatment option.
References
- Silver AG, Baynosa RC, Mahabir RC, et al. Acral myxoinflammatory fibroblastic sarcoma: a case report and literature review. Can J Plast Surg. 2013 Summer;21(2):92–94.
- Michal M, Kazakov DV, Hadravský L, et al. High-grade myxoinflammatory fibroblastic sarcoma: a report of 23 cases. Ann Diagn Pathol. 2015 Jun;19(3):157–163.
- Tejwani A, Kobayashi W, Chen Y, et al. Management of acral myxoinflammatory fibroblastic sarcoma. Cancer. 2010 Dec 15;116(24):5733–5739.
- Chahdi H, Damiri A, Oukabli M, et al. Acral myxoinflammatory fibroblastic sarcoma. Orthop Traumatol Surg Res. 2010 Sep;96(5):597–599.
- Tivoli YA, Thomas JA, Chen AF, Weiss ET. Acral myxoinflammatory fibroblastic sarcoma successfully treated using Mohs micrographic surgery. Dermatol Surg. 2013 Nov;39(11): 1709–1711.
- Davis AM, O’Sullivan B, Turcotte R, et al. Late radiation morbidity following randomization to preoperative versus postoperative radiotherapy in extremity soft tissue sarcoma. Radiother Oncol. 2005 Apr;75(1):48–53.

