 by James Q. Del Rosso, DO
by James Q. Del Rosso, DO
Dr. Del Rosso is with JDR Dermatology Research/Thomas Dermatology in Las Vegas, Nevada. Mr. Allison is with L’Oréal Active Cosmetics in New York, New York.
FUNDING: L’Oreal USA provided funding for Konic Limited for their work related to manuscript preparation.
DISCLOSURES: Dr. Del Rosso has served as a consultant and advisor to L’Loreal.
ABSTRACT: Background. Ceramides are epidermal lipids that play an essential role in stratum corneum function, including maintaining physiologic permeability barrier properties. The role of ceramides in the maintenance and repair of epidermal barrier function is believed to be valuable in the treatment of psoriasis. Normalization of corneocyte desquamation and the incorporation of agents that promote desquamation to reduce hyperkeratosis are also regarded as key factors in psoriasis management.
Objective.We sought to evaluate the benefits of two formulations (CeraVe® Body Cleanser [Cer-PSO-BCl] and CeraVe® Body Cream [Cer-PSO-Cr]), containing ceramides, salicylic acid, and urea in patients with a history of psoriasis, including those with mild-to-moderate psoriatic flares.
Methods. This was a two-center customer usage study involving 33 male and female subjects, 18 years of age or older, with a history of mild-to-moderate psoriasis. Cer-PSO-Cr was applied liberally wherever psoriasis was present twice a day for two weeks. Cer-PSO-BCl was recommended for use twice a week. Product attributes, performance of individual test products, and use of this combination regimen (favorable or unfavorable) were assessed using a self-assessment questionnaire at Week 2.
Results.Overall, 72.7 and 75.8 percent of patients with psoriasis reported the Cer-PSO-Cr alone or Cer-PSO-Cr/Cer-PSO-BCl regimen improved the appearance of their skin. For the cleanser, 97.0 percent reported it rinsed clean with no unpleasant residue. For cream and cleanser together, 84.8 percent reported it provided relief of psoriasis, and 90.9 percent reported that their skin felt soft and smooth.
Conclusions. Based on results reported by the study patients, the evaluated ceramide/keratolytic-containing cream and cleanser both yielded a high level of patient acceptance regarding improvement in skin characteristics in patients with psoriasis, including when used as a combination adjunctive regimen.
KEYWORDS: Psoriasis, ceramides, keratolytic, moisturizer
J Clin Aesthet Dermatol. 2019;12(7):18–21
Psoriasis is a common inflammatory skin disease that develops due to a variety of genetic and epigenetic factors. Clinical experience and molecular studies have suggested that epidermal permeability barrier dysfunction contributes directly to the underlying pathogenesis of psoriasis.1–3 Improvement of epidermal permeability barrier function with the use of an occlusive agent alone can mitigate psoriasis clinically.4–7 These findings support the value of methods that normalize epidermal barrier function, primarily within the stratum corneum (SC), in the management of psoriasis. Separately, the inclusion of agents that promote physiologic desquamation and reduce hyperkeratosis are likely to provide additional benefit in the topical management of psoriasis.
Moisturizers/barrier repair formulations and keratolytic/desmolytic agents are clinically recognized as valuable topical treatment agents for psoriasis.5–8 Ceramides are the predominant lipids found within the SC, contributing to the intercellular lipid bilayer, which is involved directly in regulation of transepidermal water loss (TEWL).8,9 The depletion of ceramides in the SC is thought to be one of the etiological factors that produces dryness and barrier disruption in many skin conditions. Depletion of ceramides in the SC has been reported in patients with psoriasis, and dry skin is commonly associated.10–12 It has been suggested that not only does ceramide reduction induce defects in water retention and barrier function, but altered epidermal proliferation might also be an associated sequelae.13 Animal studies and skin biopsies from human patients with psoriasis have suggested that ceramides play a relevant role in the pathophysiology of psoriasis.14–16 However, data on the use of emollients containing ceramides for psoriasis, either alone or in combination with other topical therapies, are limited. A study of a ceramide-containing moisturizer as adjunctive and preventative therapy in psoriasis patients demonstrated superiority of the combination with mometasone furoate 0.1% cream, compared to topical monotherapy, with less relapse or rebound of psoriasis.17
Management guidelines recommend the use of keratolytics, such as topical preparations containing urea and salicylic acid, as adjuvant therapy in psoriasis.18,19 Salicylic acid, a desmolytic agent, induces physiologic desquamation, which, in turn, reduces intercellular cohesion between corneocytes by dissolving the intercellular cement within corneodesmosomes.20 Salicylic acid also promotes the reduction of the SC pH, leading to optimal epidermal barrier structure and function, which correlates with smooth, healthy, elastic skin.20 The moisturization capacity of urea, a component of natural moisturizing factor (NMF), in xerotic and scaly skin has also been well-established.7,21,22
In our study, we investigated the product attributes and performance of two ceramide/keratolytic-containing formulations (CeraVe® Body Cleanser [Cer-PSO-BCl] and CeraVe® Body Cream [Cer-PSO-Cr]; L’Oréal S. A., Clichy, France) in patients with a history of psoriasis, including those with mild-to-moderate psoriatic flares.
Methods
Study design. This study was conducted in July 2017 at two centers in the United States. The IntegReview Institutional Review Board in Austin, Texas, approved the protocol, and the study was conducted according to the principles of the Declaration of Helsinki. All participants signed an informed consent form after reviewing the study protocol and the consent form, and having any questions addressed.
Inclusion criteria. Eligible patients were were healthy men or women, aged 18 to 75 years, with a history of psoriasis on the face or body and psoriatic skin lesions manifesting within the past year. Approximately 50 percent of the patients were required to have clinically determined, visible, mild-to-moderate psoriatic skin outbreaks, determined by a score of 1 or 2 points for erythema and scaling, according to a 4-point severity scale, where 0=none and 3=severe.
Exclusion criteria. Patients were instructed to avoid any over-the-counter medication or skin moisturizing products for at least two days prior to initial clinic visit (baseline) and to wear clothing that would allow easy assessment at baseline and Week 2. Patients could not be currently using other psoriasis therapies, have other dermatologic disorders, or be undergoing any other treatments that could interfere with study outcome assessment.
Treatment regimen. Patients were provided with preweighed units of Cer-PSO-BCl and Cer-PSO-Cr. Both formulations contain ceramides, 2% salicylic acid, and a high concentration of urea. Patients were instructed to apply the cream liberally wherever psoriasis was present twice a day for two weeks. The patients were instructed to use the cleanser twice a week.
Outcome measures. Patients were evaluated after two weeks using a self-assessment questionnaire to determine the product attributes and performance of each test material, individually and as a combination treatment regimen. Treatments were assessed through tailored questions on a number of product attributes (e.g., “cream glides onto skin easily”) and performance (e.g., “improves the appearance of my skin”), with responses either being favorable (agree completely or somewhat) or unfavorable (disagree completely or somewhat).
Statistical analyses. The significance of differences (favorable vs. unfavorable responses) was calculated from a binomial (sign) test. The testing hypothesis was that the proportion of the combined designated favorable responses would be equal to the combined designated unfavorable responses.
Results
Patients. Overall, 36 patients were enrolled in the study, with three patients lost to follow-up (n=1) or discontinued (n=2) due to nonadherence. No patient discontinued from either study due to lack of efficacy or adverse events. The intent-to-treat (ITT) and per protocol (PP) populations were the same size (n=33), with the PP population used for all analyses. Patients had a mean age of 49.2 years. In regard to race, 48.5 percent (n=16) were Caucasian, 21.2 percent (n=7) were black or African-American, and 21.2 percent (n=7) were Asian. Fitzpatrick Skin Types II (24.2%), III (27.3%), IV (21.2%), and V (27.3%) were noted. Additionally, a visible, mild-to-moderate psoriasis flare was observed in 16 patients (48.5%).
Efficacy. Overall, a statistically significant number of patients selected favorable responses compared to unfavorable responses for each test formulation individually and both test formulations used as combination treatment over two weeks (all p<0.001).
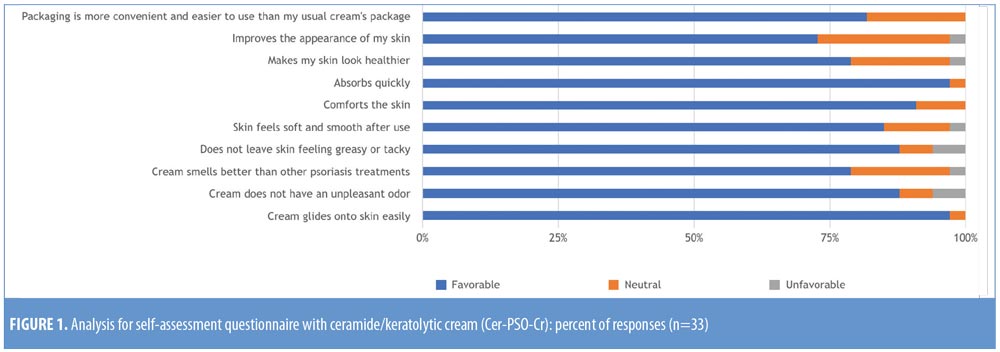
For the cream, the most favorable patient-reported aspects were “glides easily onto skin” (97.0%) and “absorbs quickly” (97.0%); 72.7 percent of patients stated that it improved the appearance of their skin. All attributes and performance of the cream were scored as “favorable” by more than 70 percent of patients. Four attributes scored no unfavorable responses (“glides easily onto skin,” “comforts the skin,” “absorbs quickly,” and “packaging more convenient”)(Figure 1).
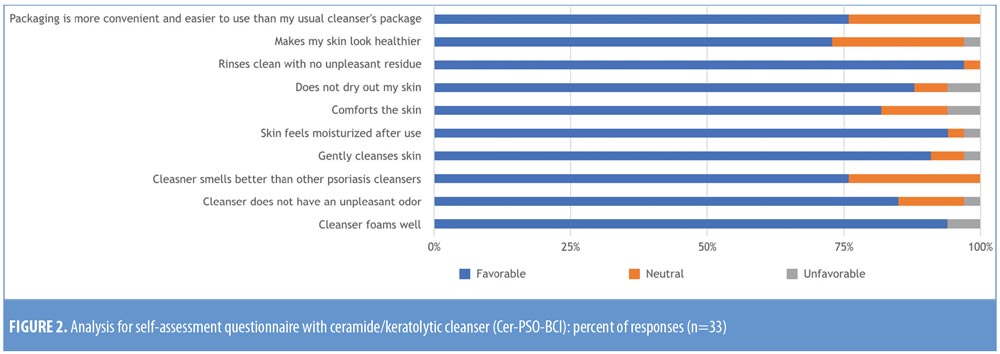
For the cleanser, the most favorable aspects were “rinses clean with no unpleasant residue” (97.0%), “skin feels moisturized” (93.9%), and “foams well” (93.9%). All attributes and performance were scored as “favorable” by more than 70 percent of patients. Three attributes scored no unfavorable responses (“cleanser smells better than other psoriasis cleansers,” “rinses clean with no unpleasant residue,” and “packaging more convenient”)(Figure 2).
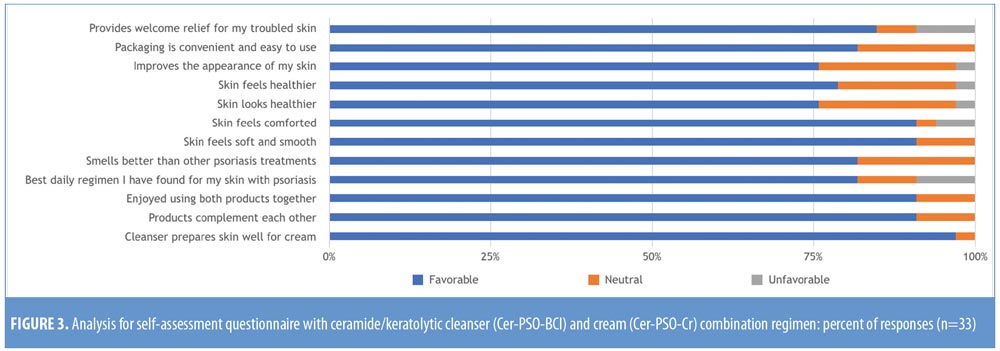
For the cleanser and cream combination treatment regimen, the most favorable aspects were “cleanser prepares skin well for cream” (97.0%), “products complement each other” (90.9%), “enjoy using both together” (90.9%), “skin feels soft and smooth” (90.9%), and “skin feels comforted” (90.9%); 75.8 percent of patients stated that the combined regimen improved the appearance of their skin. All attributes and performance of the treatment regimen were scored as “favorable” by more than 70 percent of patients. Six attributes scored no unfavorable responses (“cleanser prepares skin well for cream,” “products complement each other,” “enjoyed using both products together,” “smells better than other psoriasis treatments,” “skin feels soft and smooth,” and “packaging more convenient”)(Figure 3).
Discussion
Psoriasis is a chronic disorder, with frequent recurrences of signs and symptoms. Epidermal barrier impairment is an important manageable feature of psoriasis and appears to correlate with disease severity. Moisturizers/barrier repair formulations and keratolytic agents are recommended as part of the topical treatment strategy for psoriasis. Ceramide-containing products offer beneficial effects in improving barrier function, reducing TEWL, and maintaining SC hydration.23,24 Keratolytics, such as salicylic acid and urea, can reduce scaling and hyperkeratosis,25 and are all believed to be valuable components of psoriasis management; clinical data, however, are limited.
In this study, application of a ceramide/keratolytic-containing cream and/or cleanser provided significant patient-perceived benefits within two weeks. Nearly all patients responded positively to the aesthetic attributes of each formulation (i.e., nongreasy, absorbed quickly and easily) and overall product performance (i.e., skin looks and feels healthier). In addition, a treatment regimen of twice-daily cream application with twice-weekly cleanser use appeared to provide additional benefits based on the perceptions of the study patients. Patients responded positively regarding using the two products together, with self-reported improvements in their skin (e.g., improved feel, appearance, and symptom relief), even in those who experienced psoriatic flares. Further clinical studies using the ceramide/keratolytic-containing cream and cleanser regimen, in combination with topical therapy, in patients with psoriasis would provide clearer insight into the importance of barrier repair in patients with psoriasis and the potential benefit of this approach in reducing flares of the disease.
Limitations. The primary objective of the present study was to evaluate skin care product attributes in a population of patients with chronic plaque psoriasis. Major study limitations include small size, lack of blinding, lack of control group, and lack of an active psoriasis severity definition on study entry.
Conclusion
Use of a designated ceramide/keratolytic-containing cream and cleanser provided a high level of patient acceptance when used individually or as a combination skin care regimen for the management of psoriasis.
Acknowledgment
We thank Brian Bulley, MSc (Konic Limited, Glasgow, United Kingdom) for assisting in the preparation of this manuscript.
References
- Ye L, Lv C, Man G, et al. Abnormal epidermal barrier recovery in uninvolved skin supports the notion of an epidermal pathogenesis of psoriasis. J Invest Dermatol. 2014;134(11):2843–2846.
- Wolf R, Orion E, Ruocco E, et al. Abnormal epidermal barrier in the pathogenesis of psoriasis. Clin Dermatol. 2012;30(3):323–328.
- Bergboer JG, Zeeuwen PL, Schalkwijk J. Genetics of psoriasis: evidence for epistatic interaction between skin barrier abnormalities and immune deviation. J Invest Dermatol. 2012;132(10): 2320–2321.
- Fredman SJ. Management of psoriasis vulgaris with a hydrocolloid occlusive dressing. Arch Dermatol. 1987;123(8):1046–1052.
- Draelos ZD. Moisturizing cream ameliorates dryness and desquamation in participants not receiving topical psoriasis treatment. Cutis. 2008;82(3):211–216.
- Ghali FE. Improved clinical outcomes with moisturization in dermatologic disease. Cutis. 2005;76(6 Suppl):13–18.
- Fluhr JW, Cavallotti C, Berardesca E. Emollients, moisturizers, and keratolytic agents in psoriasis. Clin Dermatol. 2008;26(4):380–386.
- Elias PM, Menon G, Elias PM. Structural and lipid biochemical correlates of the epidermal permeability barrier. Adv Lipid Research. 1991;24:1–26.
- Del Rosso JQ, Levin J. The clinical relevance of maintaining the functional integrity of the statum corneum in both healthy and disease-affected skin. J Clin Asthet Dermatol. 2011;4(9):22–42.
- Imokawa G, Abe A, Jin K, et al. Decreased level of ceramides in stratum corneum of atopic dermatitis: an etiologic factor in atopic dry skin. J Invest Dermatol. 1991;96(4):523–526
- Matsumoto M, Umemoto N, Sugiura H, et al. Difference in ceramide composition between “dry” and normal skin in patients with atopic dermatitis. Acta Derm Venereol (Stockh). 1999;79(3):246–247.
- Chung S, Kong S, Seong K, et al. Gamma-Linolenic acid in borage oil reverses epidermal hyperproliferation in guinea pigs. J Nutr. 2002;132(10):3090–3097.
- Lew BL, Cho Y, Kin J, et al. Ceramides and cell signaling molecules in psoriatic epidermis: reduced levels of ceramides, PKC-theta and JNK. J Korean Med Sci. 2006;21(1):95–99.
- Nakajima K, Terao M, Takaishi M, et al. Barrier abnormality due to ceramide deficiency leads to psoriasiform inflammation in a mouse model. J Invest Dermatol. 2013;133(11):2555–2565.
- Cho Y, Lew BL, Seong K, Kim NI. An inverse relationship between ceramide synthesis and clinical severity in patients with psoriasis. J Korean Med Sci. 2004;19(6):859–863.
- Hong KK, Cho HR, Ju WC, et al. A study on altered expression of serine palmitoyltransferase and ceramidase in psoriatic skin lesion. J Korean Med Sci. 2007;22(5):862–867.
- Liu M, Li X, Chen XY, et al. Topical application of a linoleic acid-ceramide containing moisturizer exhibit therapeutic and preventive benefits for psoriasis vulagris: a randomized controlled trial. Dermatol Ther. 2015;28(6):373–382.
- Menter A, Korman NJ, Elmets CA, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: section 4. Guidelines of care for the management and treatment of psoriasis with traditional systemic agents. J Am Acad Dermatol. 2009;61(3):451–485.
- Nast A, Boehncke WH, Mrowietz U, et al. German S3-guidelines on the treatment of psoriasis vulgaris (short version). Arch Dermatol Res. 2012;304(2):87–113.
- Lebwohl M. The role of salicylic acid in the treatment of psoriasis. Int J Dermatol. 1999;38(1):16–24.
- Hagemann I, Proksch E. Topical treatment by urea reduces epidermal hyperproliferation and induces differentiation in psoriasis. Acta Derm Venereol. 1996;76(5):353–356.
- Pan M, Heinecke G, Bernardo S, Tsui C, Levitt J. Urea: a comprehensive review of the clinical literature. Dermatol Online J. 2013;19(11):20392.
- Del Rosso JQ. Repair and maintenance of the epidermal barrier in patients diagnosed with atopic dermatitis. J Clin Aesthet Dermatol. 2011;4(6):45–55.
- Del Rosso JQ, Zeichner J, Alexis A, et al. Understanding the epidermal barrier in healthy and compromised skin: clinically relevant information for the dermatology practitioner. J Clin Aesthet Dermaol. 2016;9(4 Suppl 1):S2–S8.
- Jacobi A, Mayer A, Augustin M. Keratolytics and emollients and their role in the therapy of psoriasis: a systematic review. Dermatol Ther. 2015;5(1):1–18.

