 J Clin Aesthet Dermatol. 2023;16(2):19–23.
J Clin Aesthet Dermatol. 2023;16(2):19–23.
by Patrícia Froes Meyer, PhD; Rafaella Rêgo Maia, MSc;
Eneida de Morais Carreiro, MSc; Rodrigo Marcel Valentim da Silva, PhD;
Lorena Beatriz Ramos Bezerra, Sr; Stephany Luanna Queiroga Farias, Sr; and
Fábio dos Santos Borges, MSc
Drs. Meyer, Da Silva, and Mr. Maia are with the Federal University of Rio Grande do Norte in Natal, Brazil. Drs. Meyer and Carreiroa are with Rio Grande do Norte University Centre (UNIRN) in Natal, Brazil. Dr. Da Silva is additionally with Estácio de Sá University in Natal, Brazil. Drs. Bezerra and Farias are with Potiguar University in Natal, Brazil. Dr. Borges is with Estácio de Sá University in São Paulo, Brazil
ABSTRACT: Background. High-intensity stationary therapeutic ultrasound (HITU) technology is gaining popularity as an attractive modality for treating different conditions, but little is known about its application in aesthetics.
Objective. To analyze the effects of stationary unfocused ultrasound (HITU technology) in treating localized fat in women’s abdominal region.
Methods. The sample consisted of 43 women with localized abdominal adiposity, assessed pre and post-treatment by assessment protocols, adversity analysis questionnaires, ultrasound exams, and serum level exams. The volunteers were randomly divided into three subgroups: G-1, who used the device off, G-2 received therapy with the device once a week for two months (Parameters: Pulsed – 100Hz – 50% – 4.0 W/cm2 – 20 minutes) and the G-3 who used the device on twice a week for a month (Parameters: Pulsed – 100Hz – 50% – 3.2W/cm2 – 30 minutes). All groups received eight sessions in total.
Results. There was a significant reduction for G-3 in the plicometry of the lower right region (p=0.01) in the comparison between the final and initial moments. In the comparison among the three research groups, there was a significant reduction in plicometry in the lower right (p=0.03) and left (p=0.02) regions in G3. Via ultrasound, a reduction in the fat layers average was observed in all groups. In G-3, there were significant differences in the left infraumbilical region (p=0.02) and right (p=0.04). In the group comparison, the right infraumbilical region showed significant differences (p=0.04) for the G-3. No differences were found for weight, BMI, body fat percentage and supra, infra and umbilical perimetry (p>0.05). The adverse reactions reported were: Mild hyperaemia (75%) and sensation of shock (21%), there were also reports of improvement in fluid retention in 93.7 percent of the volunteers, and most were satisfied with the result. Conclusion: Both treatment protocols for the reduction of localized adiposity were effective compared to the placebo group, with a significant reduction in the use of ultrasound and plicometry in the concentration of fat in the lower abdominal region. Keywords: Ultrasound, HITU, localized fat
Ultrasound is one of the treatment methods most used for intervention in the mechanical properties of injured tissues, among other applications in aesthetics. The effects of ultrasound depend on its application parameters, the amount of energy it will reach a specific location, and the characteristics of ultrasound, i.e., the frequency, mode the wave will be generated, intensity, and its direct influence on the production of thermal and non-thermal effects.1
The increased tissue temperature observed in continuous ultrasound, causes an increase in local blood flow, membrane permeability, and the distensibility of collagen fibers, increasing the regeneration capacity of injured tissues and tissue elasticity. In the pulsed form, non-thermal or mechanical effects predominate—stable cavitation, acoustic microflow and radiation force.2
Ultrasonic vibrations cause tissue compressions and expansions at the same frequency emitted by the device. The mechanical effect is also called micro-massage and consists of the tissues’ mechanical reaction due to the ultrasonic wave pressure. The effect of unstable cavitation can occur under high intensities, suggesting that cavitation is the physical mechanism responsible for cellular changes. Changes in the membrane and consequent destruction of different types of cells submitted to ultrasound treatment are evidenced in the literature.3
The effectiveness of ultrasound has already been demonstrated in several studies, mainly associated with other therapies. Its application requires the operator to perform mechanical and repetitive movements so that the entire area is treated equally. However, this can lead to fatigue and consequent loss of therapy efficiency. The development of stationary ultrasound (High-Intensity Therapy Ultrasound – HITU technology) arose from the need to use technologies that guarantee the potentiation and practicality of treatments, allowing the optimization of time associated with efficient dosimetry thus providing a simultaneous treatment of large body areas.4,5,6
However, little is known about the effects of stationary ultrasound technology on localized adiposity. Moreover, it is necessary to demonstrate the behavior of serum levels after using these chosen parameters to guarantee their safety. Thus, the purpose of the present study was to analyze the effects of non-focused stationary ultrasound in the treatment of localized fat in the abdominal region of women.
Methods
Research characterization. This experimental study compared “before and after” treatment results. The research was approved by the Research Ethics Committee (code: 5.231.138) and was conducted under the recommendations of the Consolidated Standards of Reporting Trials – CONSORT (CONSORT TRANSPARENT REPORTING OF TRIALS, 2010). All volunteers signed the free and informed consent form before the beginning of the study, and the treatment was carried out from August 2021 to November 2021.
Population, sample and criteria. The sample consisted of 48 volunteers who had localized adiposity. Inclusion criteria were women aged 25 to 50 years, who had a body mass index (BMI) between 18.5 and 29.99 (Normal to Overweight), and who had localized supraumbilical and infraumbilical fat with thicker than 30mm (identified via ultrasound imaging). The volunteers were evenly and randomly distributed into three subgroups, G-1, G-2, and G-3. During the treatment, five volunteers were discontinued, and the study ended with 43 participants (G-1 with 15 volunteers, G-2 with 14 volunteers, and G-3 with 14 volunteers).
Data collection instrument. All participants underwent evaluation of anthropometric and ultrasound measurements, performed pre-treatment and one week after the final session. An ultrasound device (Eco palm Wi-Fi, 10MHZ, China), a semi-professional camera (Canon, SX530 HS, Japan), a tape measure (Fibre Glass Tape, China), and an adipometer (Sanny, São Paulo, Brazil) were used, a bioimpedance balance (Omron, Japan) and an Ultraplace™ stationary unfocused ultrasound device with 64cm2 (infraumbilical) and 32cm2 (supraumbilical) transducers manufactured by Medical San™, (Rio Grande do Sul, Brazil).
The instruments for data collection throughout this research were the Physiotherapeutic Assessment Protocol in Localized Adiposity (PAFAL)7, an instrument used to obtain information such as identification, anamnesis, lifestyle habits, physical examination, with measurements and tests such as weight, height, BMI, skin folds, and waist circumference. The skinfolds of the infraumbilical region were measured three times, verified 2cm beside the umbilical scar, with a result based on the average values obtained in the measurements. The abdominal circumference measurement was performed in the infraumbilical region, verified 5cm below the umbilical scar. Bioimpedance was also performed, where body weight, BMI and fat percentage were monitored.
The photos were recorded in anterior and lateral orthostatism views (right and left). Subsequently, the volunteers underwent ultrasound examination, which was performed in the infraumbilical region, in a demarcated area of 10cm2, with the volunteer in the supine position. This method made it possible to evaluate the thickness of the fat layer in centimeters of the infraumbilical region before the beginning of the procedures and after the proposed treatment.
The volunteers underwent laboratory tests (lipid profile) before and up to three days after the last treatment session to analyze serum levels regarding triglycerides, total cholesterol, HDL-cholesterol, LDL and VLDL.
Upon completing the established protocol, the volunteers answered the Segot-chicq et al8 patient satisfaction analysis questionnaires and the Global Aesthetic Improvement Scale – GAIS, by Narins9, which is used to classify the treatment response, allowing a comparative assessment at different times after the therapeutic intervention.
Procedures. The G-1 group received a stationary ultrasound session with the device turned off and positioned in the target area for 20 minutes, while the G-2 group received a weekly session for two months, using the following modulation parameters: Pulsed, frequency of 100Hz, a duty cycle of 50 percent, and intensity of 4.0W/cm2, for 20 minutes; and finally, the G-3 received two weekly sessions for one month and using the modulation parameters: frequency of 100Hz, a duty cycle of 50 percent, and intensity of 3.2W/cm2, for 30 minutes).
The volunteers were instructed to carry out their tasks normally, without interrupting their daily activities. In the end, volunteers were reassessed by PAFAL, and the proposed questionnaires were applied.
Data analysis. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) software version 24.0 for Windows, following the principles of intention-to-treat analysis. In the descriptive analysis, the mean was used to measure central tendency, the standard deviation as a measure of dispersion, and the distribution of absolute and relative frequency in qualitative variables. The Levene test was applied for variance homogeneity analysis. The W. Mauchly test of sphericity was applied, and, when violated, a technical correction of the Greenhouse-Geisser test was used. The Tukey post hoc was applied for an F of F test. A significance level of 5 percent (p<0.05) was adopted, and a mixed model ANOVA was used for multiple comparisons.
Results
The analysis of body weight, BMI, and percentage of body fat showed no significant changes after the final assessment. Similarly, there was no significant difference in supraumbilical, infraumbilical, and umbilical perimetry (p>0.05).
For the intragroup analysis of the plicometry data, there was a significant reduction for G-3 in the lower right region (p=0.01) in the comparison between the final and initial moments. Furthermore, in the comparison between groups, there was a significant reduction in the lower right (p=0.03) and left plicometry (p=0.02). As a result, it was observed that there was a significant reduction in the concentration of fat in the lower region, more pronounced in the group two applications in the week.
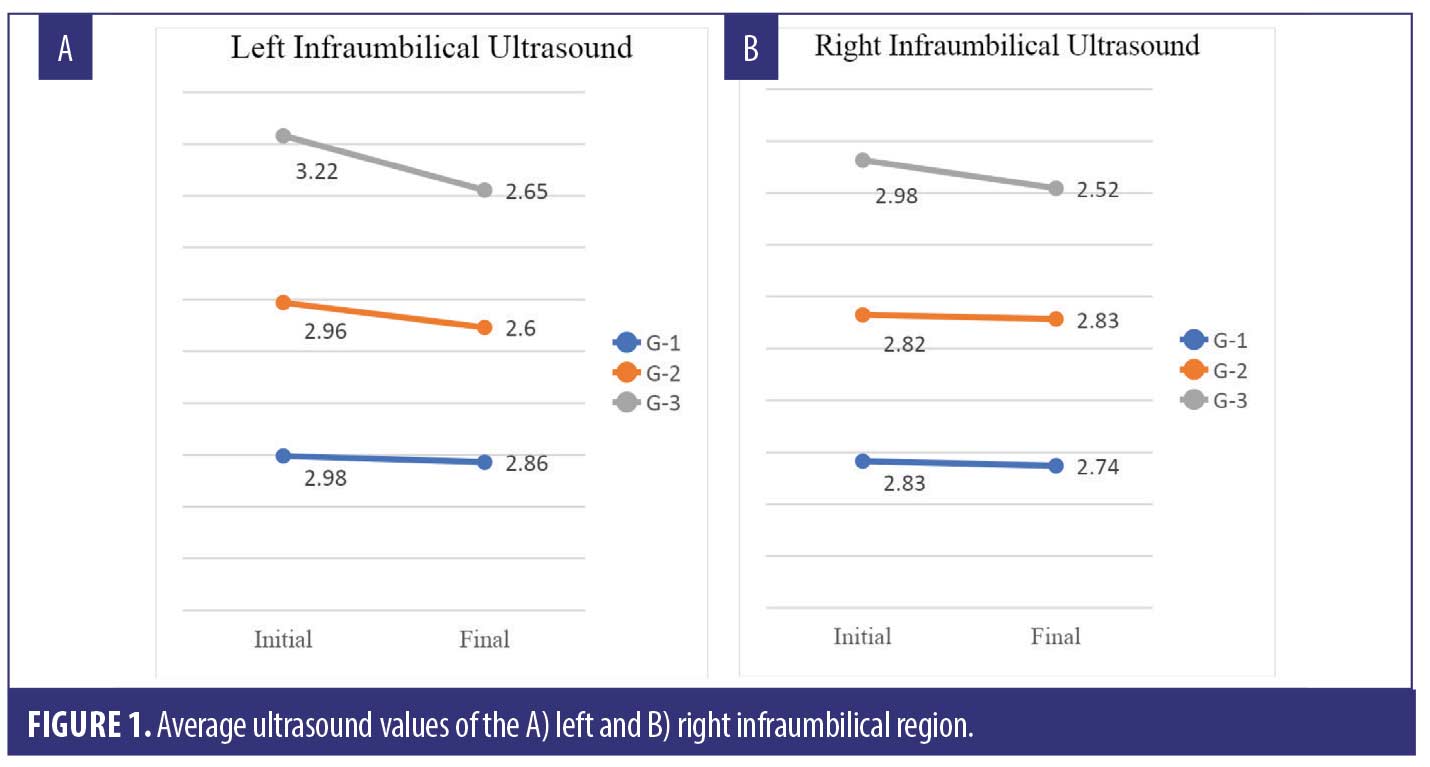
Concerning the ultrasound values, a reduction in the averages of the fat layers was observed in all groups, more expressively in G-3 (Figure 1). In the intragroup analysis, there was no significant difference in the measurements of the supraumbilical region (p<0.05), however, for the G-3 group, significant differences were obtained in the left (p=0.02) and right infraumbilical region (p=0. 04). In the group comparison, the right infraumbilical region showed significant differences (p=0.04) for the G-3.
The lipid profile values before and after the sessions generally showed a reduction in the control group and an increase in the group treated once a week, except for HDL, which showed the opposite behavior. G-3 showed an increase in some variables and a reduction in triglycerides and VLDL cholesterol levels. However, none of the results exceeded the risk reference values of the lipid profile exams.
The photographs taken prior to the intervention were taken eight sessions after the beginning of the protocol. Figures 2 to 4 show the physical changes in the institutions of each group, making it possible to observe the reduction of abdominal fat, mainly in the infraumbilical region in groups G-2 and G-3.


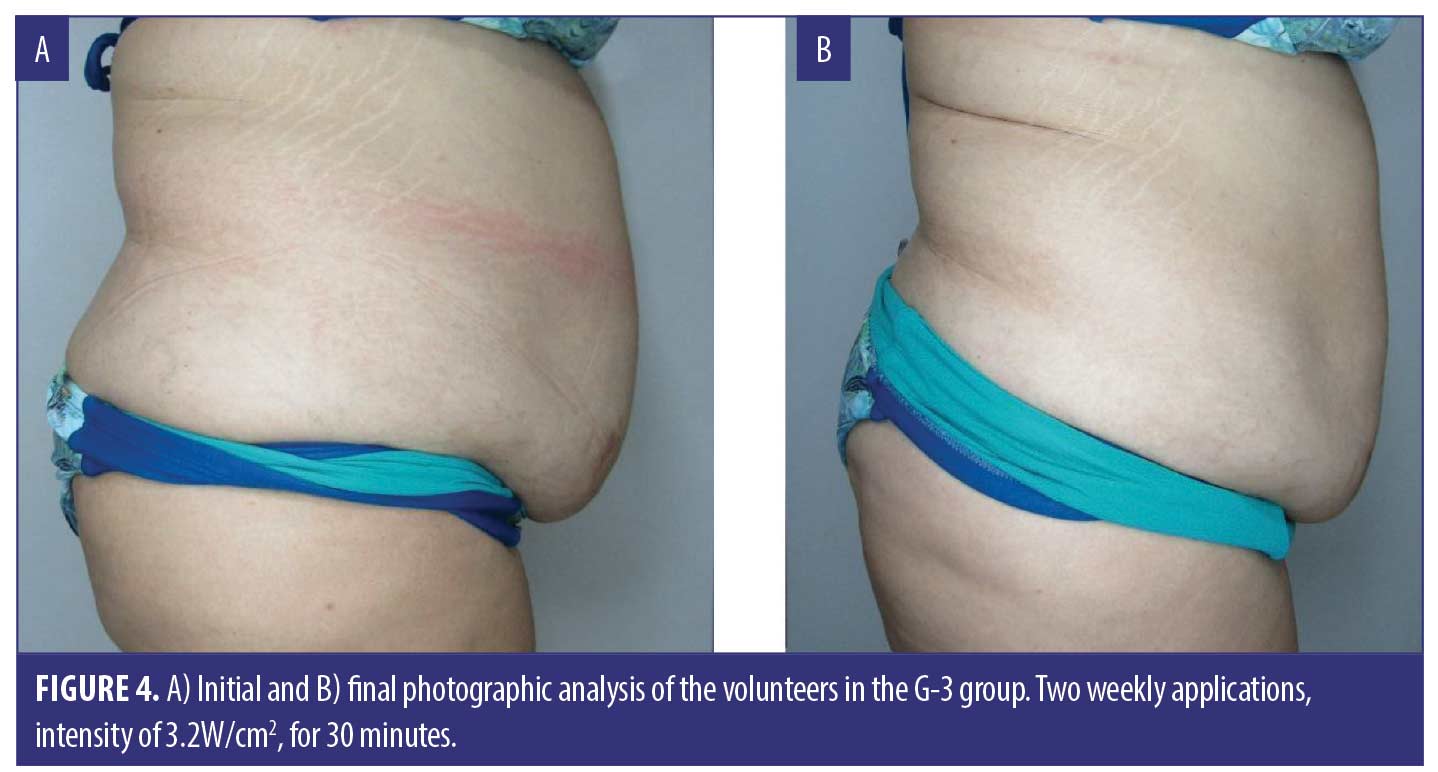
At the end of the treatment sessions, a questionnaire was applied to assess adverse reactions. The reactions reported by the volunteers were mild hyperaemia, which was present in 75 percent of the volunteers, and a sensation of shock in 21 percent. The other reactions, such as burning, numbness, tingling, hematoma, hypersensitivity, blistering, presence of skin tags or sensation of shock, were not observed by the volunteers during the treatment. Other analyzed variables showed that 93.7 percent of the volunteers reported an improvement in liquid retention, 86 percent reported that the clothes were loose, and most volunteers (62.5%) reported being very satisfied with the results.
Discussion
The term “therapeutic ultrasound” encompasses many existing and potential clinical applications. Although HIFU (High-Intensity Focused Ultrasound) is perhaps the resource receiving the most clinical attention, many collimated, non-focusing high-intensity ultrasound equipment is also being considered.10 High-intensity stationary ultrasound (HITU) technology is gaining popularity as an attractive modality for treating uterus, liver, prostate tumors, etc.11 However, literature on its application for aesthetic purposes is scarce, and this study is a pioneer in this area.
For some authors12,13 in high-intensity therapeutic ultrasound, which can also be characterized as high-intensity focused ultrasound (HIFU), the high-power beams are generated from sources outside the body. They are designed to allow rapid heating of a target tissue volume, leaving tissue in the ultrasound propagation path relatively unaffected. Therefore, acoustic field characterization is essential for accurately predicting ultrasound-induced biological effects on tissue.
Initially, when treating with this technology (stationary focused ultrasound), it is necessary to observe the specifics of the transducer. Transducers designed to be used in external applications, mainly in abdominal organs, are located relatively far from the treatment area. The ultrasound must generally pass through an intermediate medium that must be protected before reaching the target area. For this, most external treatments are performed at a frequency close to 1 MHz, so the acoustic intensity provided by external transducers can reach a certain amount of W/cm2 at the point to be treated.14,15 Given these characteristics, these research parameters were chosen to reach the subcutaneous tissue without causing adverse effects on the volunteers.
The use of high-power stationary ultrasound (HPPTUS) was first described in 1983. In the technique used, the ultrasound power was first increased to the threshold pain level (e.g., 1.5 w/cm) and then reduced to half the intensity. Then, during the next 2 to 3 minutes, the intensity was increased again with frequent questions about the patient’s sensations (only up to the original pain threshold level).16
In treatments with stationary ultrasound applications, the temperature reached in the tissue depends on the properties of the tissue to be treated and on the ultrasonic parameters, a critical parameter to maintain patient safety. The study by Cortela et al17 used bovine muscle tissue samples to analyze the effects of stationary ultrasound (HITU) application. After applying four cycles, the authors believed that temperature had a cumulative effect on the structures and proteins that make up the tissue, showing a relationship with the denaturation of proteins, which occurs in the range of 40 to 50°C.
Although no studies were found that directly employ stationary ultrasound technology (HITU) to reduce localized fat, several scientific shreds of evidence already used the HIFU model, high-intensity focused ultrasound, to reduce subcutaneous fat.18,19,20
In this study, stationary ultrasound provided a significant difference in the reduction of localized adiposity in the means found in plicometry and ultrasound. Compared to the control, the parameters used in the treated groups proved efficient. These findings corroborate the studies by Fatemi21, who reported that 282 patients who underwent a single treatment with HIFU in the abdomen and flanks had a mean reduction of 4.7cm in waist circumference after three months. In addition, Teitelbaum et al22 reported a mean reduction of approximately 2cm in the circumference of the abdomen, thighs, or flanks and approximately 2.9mm in subcutaneous fat thickness in 137 healthy subjects within two weeks, which was sustained 12 weeks after a single HIFU treatment.
Another important point is the evaluation of biochemical markers. The study by Guth et al18 showed that the use of HIFU did not promote clinically significant changes in the findings of the lipid panel or liver, pancreatic and renal functions. Similar to what we see in this study, after the application of stationary ultrasound, where the lipid profile performed did not show above the risk reference values.
The Global Aesthetic Improvement Scale (GAIS) is commonly applied after aesthetic procedures. Its use as a tool to assess HIFU effectiveness has shown self-reported patient satisfaction from 47 to 86 percent, 23 similar to this study’s findings, and among 62.5 percent of the volunteers were satisfied with the results. However, although subjective scales are essential to assess the success of cosmetic procedures, the scores obtained cannot constitute a highly satisfactory objective proof of efficacy since the placebo groups also tend to report positive results. Hence, patients’ expectations play an important role in evaluating treatment outcomes.24
In the available studies, there are some reports of adverse effects, mainly pain, swelling, and ecchymosis, which usually disappear in 1 to 2 weeks and, for most patients, a limited downtime is required after treatment.25 In the present study, only mild hyperaemia and a shock sensation were reported, and the volunteers did not need to interrupt their daily activities. We also emphasize that there were reports of improvement in fluid retention, requiring further studies to assess this condition. Several other studies on the effectiveness of HIFU treatment in reducing fat have suggested that positive results can be safely achieved without any significant effect on blood lipid or inflammatory markers and adverse local effects such as burning or scarring.18,26,27
Conclusion
A significant reduction in the analysis of ultrasound and plicometry in the concentration of fat in the lower region was shown, and these results were more pronounced in the group that received two applications a week. Considering this, it is clear that both treatment protocols for reducing localized adiposity were effective, with a higher dose once a week and a lower dose twice a week. However, further studies using other assessment methods and a larger sample size are needed to determine the effects of this therapy.
References
- Duck FA, Baker AC, Starritt HC, editors. Ultrasound in medicine. CRC Press. 2020 Jul 14.
- Barnes D. Ultrafrequência. Porto Alegre: Essência do Saber Ed. 2019; p.119–123
- Meyer PF. Efeitos da ultracavitação no tecido adiposo de coelhos. Fisioterapia Brasil. 2012;13(2):106–111.
- Shaw A, Martin E, Haller J, et al. Equipment, measurement and dose—a survey for therapeutic ultrasound. Journal of Therapeutic Ultrasound. 2016 Dec;4(1):1–9.
- Hotta TA. Nonsurgical body contouring with focused ultrasound. Plastic Surgical Nursing. 2010 Apr 1;30(2):77–82.
- Elhelf IS, Albahar H, Shah U, et al. High intensity focused ultrasound: the fundamentals, clinical applications and research trends. Diagnostic and interventional imaging. 2018 Jun 1;99(6):349–359.
- Mendonça AG, Rodrigues RD, Corradi DP, et al. Protocolo de avaliação fisioterapêutica em adiposidade localizada. Fisioter Bras. 2008 Jan:26–31.
- Segot-Chicq E, Compan-Zaouati D, Wolkenstein P, Consoli S, et al. Development and validation of a questionnaire to evaluate how a cosmetic product for oily skin is able to improve well-being in women. Journal of the European Academy of Dermatology and Venereology. 2007 Oct;21(9):1181–1186.
- Narins RS, Brandt F, Leyden J, et al. A randomised, double-blind, multicenter comparison of the efficacy and tolerability of Restylane versus Zyplast for the correction of nasolabial folds. Dermatologic surgery. 2003 Jun;29(6):588–595.
- Shaw A, ter Haar G, Haller J, et al. Towards a dosimetric framework for therapeutic ultrasound. International Journal of Hyperthermia. 2015 Feb 17;31(2):182-192.
- Xing G, Wilkens V, Yang P. Review of field characterisation techniques for high intensity therapeutic ultrasound. Metrologia. 2021 Feb 23;58(2):022001.
- Beissner K. Some basic relations for ultrasonic fields from circular transducers with a central hole. The Journal of the Acoustical Society of America. 2012 Jan;131(1):620-7.
- Okada N, Shiiba M, Takeuchi S. Developing of tough hydrophone for high intensity acoustic field at low frequency. In2016 IEEE International Ultrasonics Symposium (IUS) 2016 Sep 18 (pp. 1-4).
- Fleury G, Berriet R, Chupin L, Guey JL, Le Baron O, Mainfroy B, Martinez T. High intensity therapeutic ultrasound transducer performance and characterisation. In2010 IEEE International Ultrasonics Symposium 2010 Oct 11 (pp. 876-885).
- Aubry JF. High-intensity therapeutic ultrasound: metrological requirements versus clinical usage. Metrologia. 2012 Aug 10;49(5):S259.
- Simons DG, Travell JG. Apropos of All Muscles. In: Simons DG, Travell JG, Simons LS, editors. Travell & Simons’ Myofascial Pain and Dysfunction: The Trigger Point Manual. 2nd ed. Baltimore: Williams & Wilkins; 1999. p 94-17.
- Cortela G, Negreira C, Pereira WC. Effect of Continuous Application of Heating-Cooling Cycles on Ultrasonic Attenuation of Muscle Tissue. In: Mediterranean Conference on Medical and Biological Engineering and Computing 2019 Sep 26 (pp. 1307-1314). Springer, Cham.
- Guth F, Bitencourt S, Bedinot C, Sinigaglia G, Tassinary JA. Immediate effect and safety of HIFU single treatment for male subcutaneous fat reduction. Journal of Cosmetic Dermatology. 2018 Jun;17(3):385-9.
- Atiyeh BS, Chahine F. Evidence-based efficacy of high-intensity focused ultrasound (HIFU) in aesthetic body contouring. Aesthetic Plastic Surgery. 2021 Apr;45(2):570-8.
- Karkhi A, Kisyova R. High intensity focused ultrasound (HIFU) technology for body contouring. Journal of Aesthetic Nursing. 2019 Mar 1;8(Sup1):34-7.
- Fatemi A. High-intensity focused ultrasound effectively reduces adipose tissue. InSeminars in cutaneous medicine and surgery 2009;8(4):257-262.
- Teitelbaum SA, Burns JL, Kubota J, Matsuda H, Otto MJ, Shirakabe Y, Suzuki Y, Brown SA. Noninvasive body contouring by focused ultrasound: safety and efficacy of the Contour I device in a multicenter, controlled, clinical study. Plastic and reconstructive surgery. 2007 Sep 1;120(3):779-89.
- Alizadeh Z, Halabchi F, Mazaheri R, Abolhasani M, Tabesh M. Review of the mechanisms and effects of noninvasive body contouring devices on cellulite and subcutaneous fat. International journal of endocrinology and metabolism. 2016 Oct;14(4).
- Klassen AF, Cano SJ, Alderman A, East C, Badia L, Baker SB, Robson S, Pusic AL. Self-report scales to measure expectations and appearance-related psychosocial distress in patients seeking cosmetic treatments. Aesthetic surgery journal. 2016 Oct 1;36(9):1068-78.
- Nassab R. The evidence behind noninvasive body contouring devices. Aesthetic Surgery Journal. 2015 Mar 1;35(3):279-93.
- Fatemi A, Kane MA. High-intensity focused ultrasound effectively reduces waist circumference by ablating adipose tissue from the abdomen and flanks: a retrospective case series. Aesthetic plastic surgery. 2010 Oct;34(5):577-82.
- Shek SYN, Yeung CK, Chan JCY, Chan HHL. Efficacy of high-intensity focused ultrasonography for noninvasive body sculpting in Chinese patients. Laser Surg Med. 2014; 46(4):263–269.

