 by Iliana A. Rahimi, BSc; Igor Eberhard, PhD; and Erich Kasten, PhD
by Iliana A. Rahimi, BSc; Igor Eberhard, PhD; and Erich Kasten, PhD
Mrs. Rahimi and Professor Kasten are with the Medical School hamburg in Hamburg, Germany. Dr. Eberhard is with the Department of Social and Cultural Anthropology at the University of Vienna in Vienna, Austria.
Funding: No funding was provided for this article.
Disclosures: The authors have no conflicts of interest to relevant to the content of this article.
Abstract: Background: Tattoos have become increasing popular; however, medical complications and health risks can occur when getting a tattoo. Aim: The objective of this study is to determine whether people are properly informed about the medical risks and complications associated with tattoos and how the level of knowledge differs between those who have gotten tattooed and those who have not. Method: A cross-sectional online survey was performed. One-hundred participants had tattoos (32% male, 67% female) and 111 had no tattoos (53% male, 47% female); the average age was 26.9 years; level of education of both groups was comparable. There was a considerable (but not significant) difference between the two randomly selected samples with respect to sex and age, but both variables had no significant influence on the knowledge about medical risks, so no adjustment of the groups was carried out. The following variables were examined: demographics, characteristics of the tattoo, the intensity of the decision-making process that participants underwent before getting a tattoo, and the knowledge of medical risks and complications of tattoos. Results: More than 50 percent of the answers from both groups were incorrect (i.e., 55% of the answers from tattooed subjects were incorrect, and 58% of the non-tattooed group were incorrect). Neither sex (t-test, p=0.81) nor age (t-test, p=0.11) had any significant influence on the presence of knowledge. No significant correlations between sociodemographic variables and knowledge of medical risks of tattoos were found. No differences were found between characteristics of the tattoo and knowledge of medical risks apart from the size of the tattooed area (i.e., the larger the tattoo, the more information was sought by the person being tattooed). Differences were also found between educational levels and the knowledge of medical risks and complications of tattoos. Conclusions: Educating the public on the medical risks of tattoos might assist individuals in making more optimally informed decisions regarding whether to get a tattoo.
Keywords: Body modification, tattoo, body ink, health risks
J Clin Aesthet Dermatol. 2018;11(3):30–35
Tattoos are a form of permanent body modification or adornment that is created when an electrically driven needle inserts ink into the dermis. Tattooing is commonly practiced by people of nearly every race and country in the world. In the last three decades, tattoos have increased in popularity and are now seen on individuals from a broad range of social classes.1–3
Before government regulations were in place in many North American and European countries, tattoo ink was often manufactured by the tattoo artists themselves, and as a result, would often contain toxic substances. Many countries now regulate the composition of tattoo inks in an effort to increase safety and prevent harm to human health. Ink manufacturers are responsible for the safety of their products.5 In Germany, the composition of tattoo inks have only recently been regulated by law (2009–2010).4 Despite government regulations, however, health risks still exist due to tattooing.
Health Risks and Potential Side Effects of Tattoos
There are two levels of medical risk and complications that exist today due to tattoos: mild and advanced. Mild complaints are described as “any unusual condition, sensation or visible reaction in the tattooed skin that differs from normal skin of the same person.” These side effects are common, often ignored, and are usually treated at home.7 The application process of a tattoo damages the skin, causing blood clots to form around the broken blood vessels, creating a bruise. This damage to the skin makes taking care of the tattooed area of skin immediately after getting a tattoo imperative in order to prevent infections. The swelling of the skin around the tattoo protects the area from any further injury and helps it to heal. Advanced complaints are described as “more serious adverse reactions in tattoos, associated with objective symptoms and significant discomfort (i.e., events that would typically lead the patient to consult a physician).”7 Advanced side effects are less common and usually noninfectious. Reactions include aseptic inflammation, allergic reactions, and hypersensitivity to the tattoo ink, especially red ink, but also to chromium in green ink, cadmium in yellow ink, and cobalt in blue ink.8–15
The risk for adverse effects on health increases in individuals who obtain a tattoo in an unauthorized facility. For example, Galle et al6 found that among 597 tattooed adolescents, 23.4 percent reported complications more frequently if their tattoos were obtained in unauthorized facilities compared to those who obtained their tattoos in professional, regulated studios (35.3% vs. 15.9%, respectively). Unsterile equipment and needles can transmit infectious diseases, such as hepatitis or human immunodeficiency virus.19 This risk of infection lead the American Association of Blood Banks to require a one-year wait between obtaining a tattoo and donating blood. Additionally, tattoo ink can become contaminated with mycobacteria, which, once injected under the skin, can cause an infection that results in redness, swelling, itching, and raised pink, red, or purple blemishes in the area of the tattoo. Once the infection heals, the area might remain permanently scarred. In several states, modern tattoo studios are controlled by the health authorities and are highly sterile environments. More often than not, the problem is the lack of after-care by the customer.
Another risk factor of tattoos is the formation of granulomas around the tattoo ink; this can occur even years after obtaining the tattoo and can lead to significant allergic reactions. Inks might also contain metalliferous components (e.g., paraphenylenediamine), which can lead to pigmentary disorders, inflammations, and scarring.
Additionally, tattoos might lead to keloids, which are formations of fibrous scar tissue caused by excessive tissue repair in response to trauma or incision—in this case, due to the application of the tattoo ink.16 According to Brady et al,17 some tattoo-related skin problems can be treated with anti-inflammatory steroid drugs, while others might require surgery.
In 2011, in a study in The British Journal of Dermatology, investigators reported the discovery that nanoparticles are found in tattoo inks.20 Nanoparticles are ultramicroscopic, making them able to penetrate through skin layers into underlying blood vessels and then travel with the bloodstream. Evidence suggests that some of these nanoparticles might induce toxic effects in the brain and cause nerve damage. Some of these nanoparticles might also be carcinogenic. And according to the results of a study from the University of Bradford,20 nanoparticles from tattoo ink were found around blood vessels elsewhere in the body and could possibly enter organs and other tissues.20 Black ink is the color most often linked with high concentrations of such nanoparticles.
Some studies have found that red tattoo ink often contains azo-based hues. Azo dyes are organic compounds that are of great concern due to their potential toxicity and carcinogenic properties. Red ink appears to be connected to chronic and allergic skin reactions caused by tattoos.
There is much to learn regarding how specific pigments interact with the metabolism of the human body. For example, studies by the National Center for Toxicological Research21 report that yellow ink is broken down by enzymes and metabolized by the body. This pigment also breaks down in sunlight, often turning colorless. The chemically altered remnants of these pigments, however, remain in the skin layer, and it is still unknown if they are toxic or not.21 We do know that small amounts of ink particles always pass into the lymphatic system and accumulate in lymph nodes.22,23
Despite the heterogeneous and often unknown components of older tattoo inks, until now, no studies have shown a clear connection between tattoos and skin cancer.18 According to Doremus, however, tattoos can make it more difficult to diagnose skin cancer or can cause false identifications of cancer in lymph nodes.18
Over time, some individuals regret getting tattoos and wish to have them removed.24 In other cases, medical complications (e.g., allergic reactions, hypersensitivity to the tattoo ink, granuloma or keloid formations) require tattoo removal. Often, tattoo removal is more painful than tattooing and can leave scars.
Today, pulsed lasers are used to remove tattoos; the laser energy passes through the epidermis and is absorbed especially by dark tattoo pigments. Laser treatment does not remove the tattoo ink out of the body; rather, the relatively large pigments of the ink are broken down into much smaller particles, which are transported through the body and stored in the lymph nodes or other tissues.25 The ink does not ever really leave the body, though possibly a portion is excreted via the liver.23
Toward the end of the 19th century, the basic commodities of tattoo inks were red chalk, coal, gypsum, saffron, black clay, ox gall, carbon black, and kermes. Red ink contained vermilion, ferric oxide, and red drawing ink.26 Toward the end of the 20th century, the ink contained primarily water, alcohol, glycerin, and coloring pigments. Today, modern ink is usually free of alcohol. Modern tattoo inks might contain shellac, preservatives, aromatic amines, azo dyes, hydrochloride, food coloring, ammonia, and nickel.13, 20, 21, 27 This is a problem for those people who have allergies to one or more of these substances. Tattoo dyes are very photosensitive: light colors fade over the years. To avoid this, in the summertime, a sun blocker should be applied on the tattooed area.26
From a biological view, tattoo colors promote cell stress and weaken mitochondria.27 A study by Regensburger et al in the year 201027 analyzed black tattoo dye and discovered that it contains benzopyrene, phenol concentrations, and polycyclic aromatic hydrocarbons (PAH). Tattoo dyes with PAHs reduce the mitochondrial activity of skin cells (i.e., these cells have a more limited degree of health).27
Methods
Study design. The objective of this study is to determine whether people are properly informed about the medical risks and complications associated with tattoos and how this level of knowledge differs between those who have gotten tattoos and those who have not.
We hypothesized that people with tattoos attempt to become better informed regarding the risks of tattoos before making the decision to get a tattoo than those who remain non-tattooed. A secondary hypothesis was that individuals who have obtained several tattoos or large tattoos have better knowledge about medical risks compared to those with none or only one tattoo.
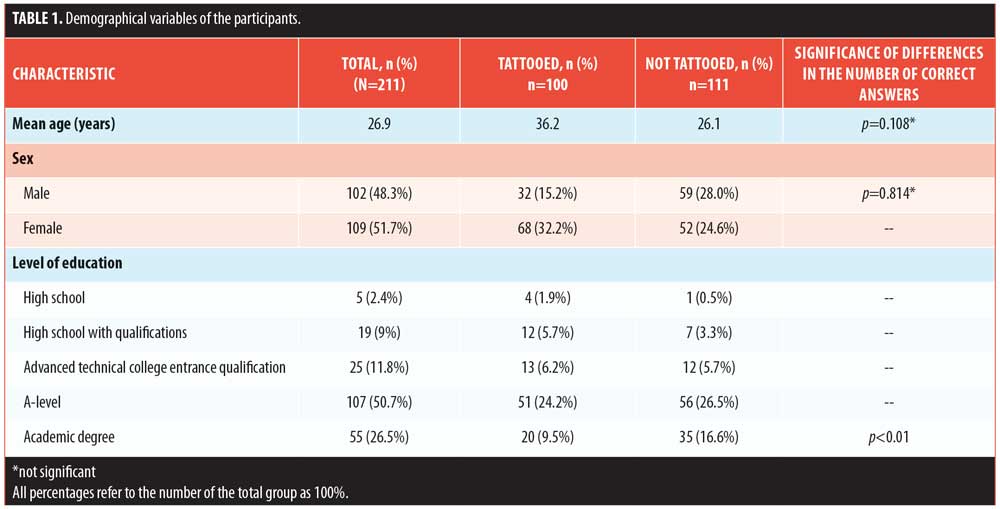
We conducted a cross-sectional online survey involving 211 participants. All participants were German individuals older than 18 years of age who either had tattoos (n=100) or did not have tattoos (n=111). In addition to questions about the medical risks of tattoos, the following variables were examined: sociodemographic characteristics (Table 1), a description of the tattoo(s), and the intensity of the decision-making process that participants underwent before getting a tattoo.
Questionnaire. An online questionnaire was created on the research website
www.soscisurvey.de during the winter of 2015–2016. Participants received instructions on how to fill out the questionnaire; one point was given for every correct answer. Demographical information was obtained from the participants, including age (range: 18–60+ years), sex, level of education (high school, high school with qualifications, advanced technical college entrance qualification, A-level, academic degree), number of tattoos, and the date of first tattoo. Thirteen yes/no questions and three closed format questions assessed knowledge of the medical risks and complications of tattoos. For testing the reliability of the answers, deliberately, four “nonsense” questions were included to which the correct answer was “no” (e.g., “Do the colors of a tattoo change due to exposure to polyester-containing clothes?”). The participants were asked to answer the questions as precisely as they could. The characteristics of the individuals’ tattoos were evaluated by the following variables: the number of tattoos (1–3, 4–6, 7–9, or 10 or more); the location (categorized by 14 locations on the body: hand, forearm, upper arm, thigh, lower leg, foot, shoulder, neck, chest, stomach, groin, back, bottom and face); the size (determined by the number(s) of a palms needed to cover the tattoo); and the number of colors (categorized by 11 different colors, specifically black, blue, brown, green, gray, pink, purple, red, ultraviolet ink, white, and yellow). The intensity of the decision-making process was measured by asking the participants how well informed they were before getting a tattoo (e.g., via the internet, magazines, friends/relatives, tattoo studio, or another source) or how well they were educated by their tattoo artist (e.h., via conversation, informed consent, or another source). The questionnaire was fully anonymous in order to respect the privacy of the respondents and to encourage participants to answer truthfully. If the participants were interested in learning more about the medical risks and complications of tattoos, they could send an e-mail after completing the survey.
Data analysis. The SPSS statistical software (IBM Corp., Armonk, New York, USA) was used for all statistical analyses. A two-tailed p-value of 0.05 was designated as the threshold for significance.
Results
Two-hundred and eleven participants filled out the questionnaire: 102 men (48.3%) and 109 women (51.7%) participated in this research. According to the results of this questionnaire, the level of education of both groups (tattooed vs. non-tattooed) was comparable; all participants had a high level of education (e.g., graduated from high school or achieved a bachelors degree). There was a considerable (but not significant) difference between the two randomly selected samples with respect to sex and age, but both variables had no significant influence on the knowledge about medical risks, so no adjustment of the groups was carried out. There was a significant difference between the informed levels with regard to knowledge of medical risks of tattoos (p<0.01). The results of the knowledge of participants about medical risks are displayed in Table 2.
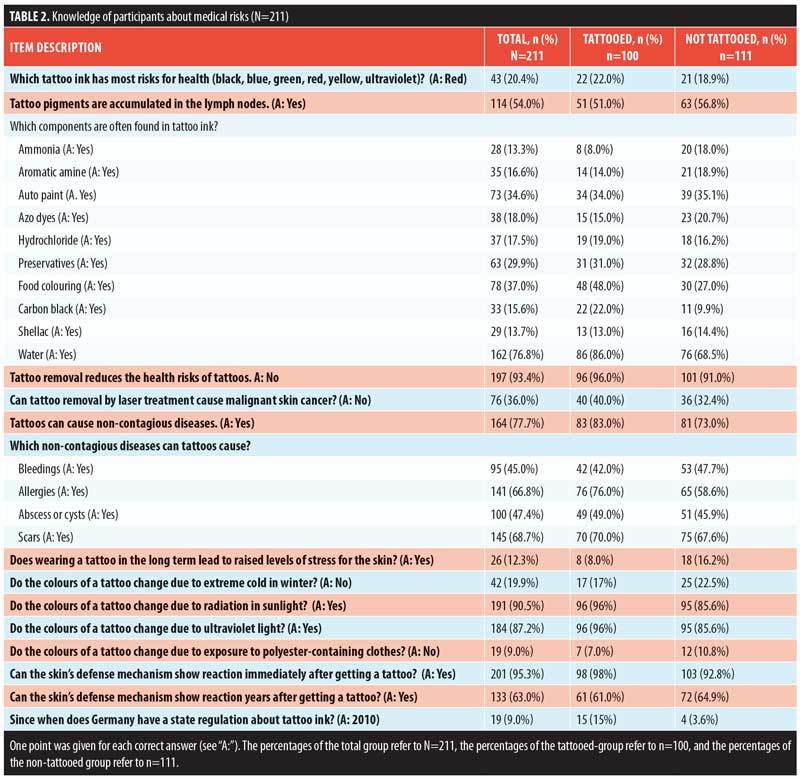
Table 2 also shows a comparison between the tattooed and the non-tattooed group concerning the correct answers of the questions. For example, out of the 211 participants, only 43 (20%) had the correct view that red ink has most risks for the health, while 168 (80%) thought yellow, green, blue, black, or ultraviolet dyes were the most dangerous. One-hundred fourteen participants (54%) were aware that tattoo dyes are accumulated in the lymph nodes. Most of the participants of both groups did not know the components of tattoo inks.
All in all, the tattooed group achieved 1,217 correct answers (45.1%; 12.2 points per participant), while the non-tattooed participants obtained 1,256 points (41.9%; 11.3 points per participant). A test for independent samples showed no significance (p=0.343).
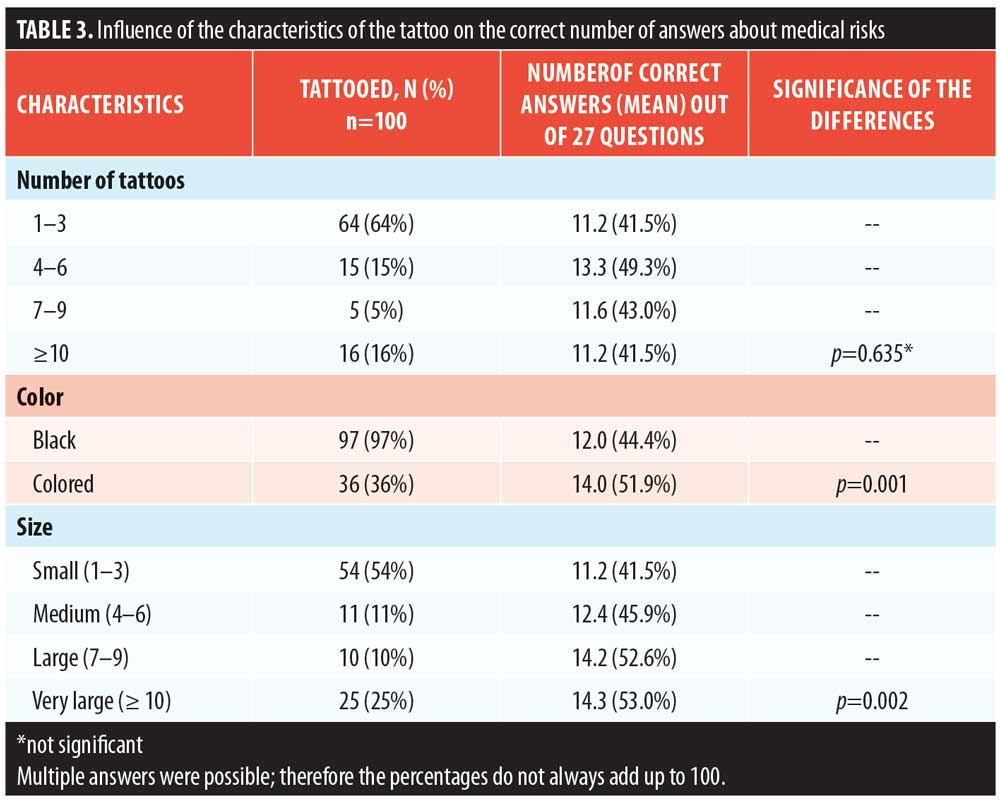
The influence that tattoo characteristics of the participants had on their levels of knowledge about risks and complications is shown in Table 3. No differences were found between the number and color(s) of the tattoo and knowledge of medical risks, apart from the size of the tattooed area (i.e., the larger the tattoo, the more information was sought).
Discussion
The main objective of this study was to investigate the extent of knowledge on medical risks associated with tattooing between tattooed individuals versus non-tattooed individuals. Two-hundred eleven participants over the age of 18 who were either tattooed (n=100) or non-tattooed (n=111) completed the study questionnaire. All participants had at least a high school level education. As described in the Methods section, 1 point was given for every correct answer, for a maximum of 27 points for each participant.
More than 50 percent of the answers in both groups were wrong (there were only 45.1% correct answers in the tattooed group and 41.9% correct answers in the non-tattooed group). This rather weak knowledge surprised us, especially due to the high level of education for the participants (i.e., all had at least finished high school). For example, only 51 percent (n=108) of the tattooed group and 57 percent (n=120) of the non-tattooed group were aware that tattoo pigments are accumulated in the lymph nodes, while 61.0 percent (n=129)(tattooed) and 64.1 percent (n=135) (non-tattooed) correctly knew that allergic reactions to tattoo ink can emerge years after obtaining a tattoo. In contrast, 96 percent (n=203) (tattooed) and 91 percent (n=192) (non-tattooed) knew that tattoo removal does not reduce the health risks of tattoos and 96 percent (n=203) (tattooed) and 85.6 percent (n=181) (non-tattooed) knew that sunlight leads to changes in the color of a tattoo. The majority of ignorance was found with respect to the components of tattoo ink; here, on average, the number of incorrect answers was between 74 percent (n=156) (non-tattooed) and 72 percent (n=152) (tattooed group).
In independent samples statistical tests, we found no significant differences between the mean results of the tattooed and the non-tattooed groups with regard to the medical risks and complications of tattoos. An examination of the demographical variables of the participants showed no significant differences in the knowledge of medical risks between the sexes and across different ages, but significance was found between the knowledge of medical risks and complications of tattoos and different levels of education. This result is in contrast to the findings of Cegolon et al,28 who compared the health awareness of 4,277 adolescents aged 14 to 22 years. They reported that boys had less knowledge of infectious diseases related to body art, were less aware of the hygienic norms to be observed after piercings or tattoos, were less likely to turn to a certified artist, and, when complications occurred, went to a professional health care provider less often.28
No significant differences were found among the tattooed group in regards to the number of the tattoos the participants had, suggesting that tattoo-related characteristics have no influence on the knowledge of the medical risks and complications of tattoos. However, in contrast to the pure number of tattoos, the size of the tattoo seemed to have a more significant impact on the level of knowledge regarding medical risks. As expected, participants with large tattoos sought information regarding the health risks of tattoos more often than did those with small tattoos or those with no tattoos, and thus had more knowledge about medical risks and complications compared to their counterparts. Therefore, the size of the tattoo and the number of details (e.g., shadowing, variety of colors) should be taken into consideration. This could be the main reason why participants who had larger tattoos also scored better on the questionnaire.
In recent years, researchers have conducted a significant number of studies on the medical risks and complications associated with tattoos.29 However, the results of these studies apparently have not reached the general population. Interestingly, the tattooed group did not have a higher level of knowledge versus the non-tattooed group. These findings demonstrate the importance of providing the public with more information on tattoos, including potential risks. An optimized understanding of medical risks associated with tattooing might influence individuals to more carefully consider the pros and cons of getting a tattoo before making a decision.
In this study, only 45.1 percent of the answers of the tattooed group and 41.9 percent of the answers of the non-tattooed group were correct. These results support the findings of Galle et al,30 who found that, among high school students, 79.4 percent knew about infectious risks and 46 percent knew about non-infectious risks. In our study, 77.7 percent of the participants knew that tattoos can cause noncontagious diseases. The respective numbers in the Galle et al study30 among university students were 87.2 percent and 59.1 percent. Only 3.5 percent of students in high school and 15 percent of university undergraduates acknowledged the risk of viral disease transmission; two percent and three percent knew about allergic risks, respectively. With a finding of 66.8 percent, this knowledge was much higher in our study. Seventy-three percent of the high school students and 33.5 percent of the university students in Galle et al’s study30 had body art done at unauthorized facilities. Approximately seven percent of both high school students and college students reported complications from their purchased body art. In another study by Galle et al,6 researchers found that 84.4 percent of freshman students reported that they knew the risks of infection associated with body art practices, but only 4.1 percent of them correctly identified the infectious diseases. Additionally, 59.2 percent of the sample declared that non-infectious diseases can occur after a tattoo or piercing, but only 5.4 percent of them correctly identified allergies, cysts, bleeding, and scars as the possible non-infectious diseases. In the study by Quaranta et al,31 78.3 percent of the participants believed it was risky to undergo piercing/tattoo practices, while 60.3 percent indicated acquired immunodeficiency syndrome (AIDS) as a possible infection, 38.2 percent identified hepatitis C, 34.3 percent identified tetanus, and 33.7 percent identified hepatitis B in the sample. Notably, 28.1 percent of freshmen were not aware that there are also non-infectious complications associated with tattoos; with a rate of 22.3 percent, we found nearly the same amount in our results.
Conclusion
In summary, the results of this research show that a substantial portion of the respondents had very little knowledge of the health risks and complications associated with tattoos. Practically no differences were found between tattooed and non-tattooed people regarding the knowledge of these risks. No difference was found between men and women with regard to their knowledge of complications; stratification by demographic variables such as age or the decision-making process were not significant. Significance was only found when the size of the tattoos and educational level were considered. These findings might help in the effective planning of health promotion strategies for those who are considering tattoos.
References
- DeMello M. “Not just for bikers anymore”: Popular representations of American tattooing. J Pop Cult. 1995; 29(3):37–52.
- Stirn A. Motivation von tätowierten und gepiercten für die körpermodifikationen. Ergebnisse einer ersten deutschen fragebogenerhebung. Z Klin Psychol Psychiatr Psychother. 2004; 52(1):43–58.
- Trampisch HJ, Brandau K. Tattoos und piercings in Deutschland: eine querschnittstudie. Available at: http://aktuell.ruhr-uni-bochum.de/mam/content/tattoo-studie.pdf. Accessed March 3, 2016.
- BGBI (Federal Law Gazette). Regulation on Inks Used in Tattoos Including Certain Comparable Substances and Mixtures Made Up of Individual Substances. 2008; 2215.
- Bundesinstitut für Risikobewertung (BfR): Fragen und Antworten zu Tätowiermitteln (FAQ des BfR vom 01. Juni 2013). Available at: http://www.bfr.bund.de/de/fragen_und_antworten_zu_taetowiermitteln-187854.html#topic_187857. Accessed December 11, 2015.
- Galle F, Quaranta A, Napoli C, et al. Body art practices and health risks: young adults’ knowledge in two regions of southern Italy. Ann Ag. 2012; 24(6):535–542.
- Serup J. Allergies and tattooing. Available at: http://www.bfr.bund.de/cm/343/allergies-and-tattoing.pdf. Accessed October 2, 2016.
- De Cuyper C, Cotapos ML. Dermatologic Complications with Body Art: Tattoos, Piercings and Permanent Make-Up. Berlin, Germany: Springer-Verlag GmbH; 2010.
- Engel E, König B. Tattoo pigments in skin: determination and quantitative extraction of red tattoo pigments. Available at: http://d-nb.info/989763633/34. Accessed October 11, 2015.
- Glassy C, Glassy M, Aldasoiuqi A. Tattooing: medical uses and problems. Cleve Clin J Med. 2012;79(11):761–770.
- Grimm S, Cronin A. Health risks associated with tattoos and body piercing. J Clin Outcomes Manag. 2014; 21(7):315–316.
- Houghton S, Durks K, Carrol A. Children’s and adolescent’s awareness of the physical and mental health risks associated with tattooing: a focus group study. Adolescence. 1995;30(120):971–988.
- Bundesamtes für Risikobewertung. “Nickel in Tätowiermitteln kann Allergien auslösen“ Stellungnahme Nr. 012/2013 des BfR () vom 25. October 2012. Available at: http://www.bfr.bund.de/cm/343/nickel-in-taetowiermitteln-kann-allergien-ausloesen.pdf. Accessed October 11, 2015.
- Kaur RR, Kirby W, Mailbach H. Cutaneous allergic reactions to tattoo ink. J Cosmet Dermatol. 2009;8(4):295–300.
- Lemeric W. Tattoo ink allergies are found to be from red ink, study says. 2015. Available at: http://www.ibtimes.com.au/tattoo-ink-allergies-are-found-be-red-ink-study-says-1450227. Accessed October 11, 2015.
- Sperry K. Tattoos and tattooing. Part II: Gross pathology, histopathology, medical complications, and applications. Am J Forensic Med Pathol. 1992;13(1):7–17.
- Brady BG, Gold H, Leger WA, Leger MC. Self-reported adverse tattoo reactions: a New York City Central Park study. Contact Dermatitis. 2015; 73(2):91–99.
- Doremus AR. Can tattoos cause skin cancer?. Clin J Oncol Nurs. 2009; 13(2):231–232.
- United States Food and Drug Administration. Tattoos & permanent makeup; fact sheet. Available at: https://www.fda.gov/Cosmetics/ProductsIngredients/Products/ucm108530.htm. Accessed May 1, 2016.
- Høgsberg T, Loeschner K, Löf D, Serup J. Tattoo inks in general usage contain nanoparticles. Br J Dermatol. 2011;165(6):1210–1218.
- Öko-Test. Tattoofarben. Available at: http://www.zentrum-der-gesundheit.de/pdf/tattoo-gesundheitsrisiko-ia-17.pdf. Accessed January 10, 2016.
- Soran A, Menekse E, Kanbour-Shakir A, et al. The importance of tattoo pigment in sentinel lymph nodes. Breast Dis. 2017 Jul 6. [Epub ahead of print].
- Sepehri M, Sejersen T, Qvortrup K, et al. Tattoo pigments are observed in the Kupffer cells of the liver indicating blood-borne distribution of tattoo ink. Dermatology. 2017;233(1):86–93.
- Burris K, Kim K. Tattoo removal. Clin Dermatol. 2007;25(4):388–392.
- United States Food and Drug Administration. Tattoo removal: options and results. Available at: https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm336842.htm. Accessed May 1, 2016.
- Feige M. Das Tattoo- und Piercing-Lexikon: Kult und Kultur der Körperkunst. Berlin, Germany: Lexikon-Imprint-Verlag; 2000.
- Regensburger J, Lehner K, Maisch T, et al. Tattoo inks contain polycyclic aromatic hydrocarbons that additionally generate deleterious singlet oxygen. Exp Dermatol. 2010;19(8):e275–e281.
- Cegolon L, Miatto E, Bortoletto M, et al. Body piercing and tattoo: awareness of health related risks among 4,277 Italian secondary school adolescents. BMC Public Health. 2010;10: 73.
- Høgsberg T, Hutton Carlsen K, Serup J. High prevalence of minor symptoms in tattoos among a young population tattooed with carbon black and organic pigments. J Eur Acad Dermatol Venereol. 2013;27(7):846–852.
- Galle F, Mancusi C, DiOnofrio V, et al. Awareness of health risks related to body art practices among youth in Naples, Italy: a descriptive convenience sample study. BMC Public Health. 2011;11: 625.
- Quaranta A, Napoli C, Fasano F, et al. Body piercing and tattoos: a survey on young adults’ knowledge of the risks and practices in body art. BMC Public Health. 2011;11:774.

