J Clin Aesthet Dermatol. 2019;12(10):24–28
 by Crystal Zheng, MD; Jeremy Quentzel, MD; and James C. M. Brust, MD
by Crystal Zheng, MD; Jeremy Quentzel, MD; and James C. M. Brust, MD
Dr. Zheng is with the Division of Infectious Diseases at Tulane University in New Orleans, Louisiana. Dr. Quentzel is with the Department of Medicine, Montefiore Medical Center & Albert Einstein College of Medicine in the Bronx, New York. Dr. Brust is with the Divisions of General Internal Medicine & Infectious Diseases, Montefiore Medical Center & Albert Einstein College of Medicine in the Bronx, New York.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Hundreds of thousands of Americans travel abroad each year for medical care, such as cosmetic silicone procedures. However, medical tourists risk encountering unqualified providers and receiving injectable or implantable cosmetic materials of questionable purity. We performed a retrospective chart review of patients treated at a multisite academic center in the Bronx, New York, between the years 2008 and 2017, and identified 12 patients who developed complications following silicone procedures performed in a foreign country, Puerto Rico, or the United States by an unlicensed provider. Procedures included silicone injections or implants in the breasts, buttocks, and face. Destination countries included the Dominican Republic, Guatemala, Venezuela, and Mexico. The patients in our study suffered significant morbidity, with complications including infection, implant rupture, and silicone migration. Laboratory and radiographic findings demonstrated nonspecific markers of inflammation. The management of silicone complications can be difficult and prolonged, and can place a large financial burden on the healthcare system as well as have significant and long-term negative consequences for the patient. Clinicians should be aware of the risks for adverse events, such as the ones described here following silicone injection and/or implant procedures, in patients who, whether for financial, cultural, or other reasons, chose to undergo cosmetic procedures in another country or by an unlicensed practictioner in the US. It is important that clinicians recognize the considerable and diverse morbidity of such patients and treat them with sensitivity and empathy to ensure optimal outcomes.
KEYWORDS: Cosmetic procedures, management, medical tourism, silicone granuloma, silicone injection
Medical tourism is a multibillion-dollar industry worldwide, and hundreds of thousands of Americans are estimated to travel abroad for medical care each year, seeking procedures such as cosmetic surgery, dentistry, and ophthalmologic procedures.1 While the advantages of medical tourism include potentially lower costs and a familiar cultural context, patients risk encountering unqualified providers and receiving medications or surgical materials of questionable purity.2 Certain cosmetic procedures, such as free silicone injections, are not approved by the United States (US) Food and Drug Administration (FDA) but are often available in other countries.3 Complications of procedures performed overseas typically manifest after the patient has returned home.4 Therefore, providers in the US must be familiar with the diagnosis and management of these adverse effects.
Silicone is widely used in cosmetic or reconstructive procedures in the form of an implant or a free injection. Reports of complications resulting from silicone procedures include local inflammation, granuloma formation, migration, embolization, and death.5 Complications in medical tourists following other types of procedures, such as abdominoplasty and liposuction, have been described; however, in our literature review, we found only five case reports of medical tourists with complications specifically from silicone procedures.6,7 These procedures were performed in the Dominican Republic,8-10 Thailand,11 and Venezuela,12 and led to complications such as pain, abscesses, and granuloma formation. The authors described diagnostic challenges, including the failure to obtain a travel history by clinicians, patient reluctance to disclose a history of medical tourism, and the nonspecific nature of the complications. Additionally, silicone injection by nonphysicians in the US poses similar risks of receiving impure materials by untrained practitioners, and have also resulted in complications.13
Montefiore Medical Center (MMC) is a multisite academic health center and the largest provider of healthcare in the Bronx, New York. MMC includes 11 hospitals and 250 ambulatory sites serving more than 500,000 patients, of whom 40 percent have Medicaid and 10 percent are uninsured.14,15 The Bronx has a large immigrant and socioeconomically disadvantaged population, where 56 percent of inhabitants are Hispanic, 34 percent are foreign-born, and 28 percent are living in poverty.16 This study describes cases of complications from silicone procedures among medical tourists encountered at MMC, highlighting the variety of clinical manifestations and the complicated medical course these patients can experience after returning to the US.
Methods
We retrospectively reviewed the electronic medical records from MMC’s three major hospitals and its ambulatory practices in the Bronx to identify all adult patients who presented for treatment between the years 2008 to 2017 and had the term silicone in their pathology reports. Individual charts were reviewed to identify patients who had undergone cosmetic procedures in a foreign country or in Puerto Rico or in the US by an unlicensed provider. Demographic, clinical, laboratory, and imaging data were recorded. The study was approved by the institutional review board of the Albert Einstein College of Medicine, which waived the requirement for informed consent due to data being previously collected during the course of routine medical care and because the study did not pose additional risks to the identified patients.
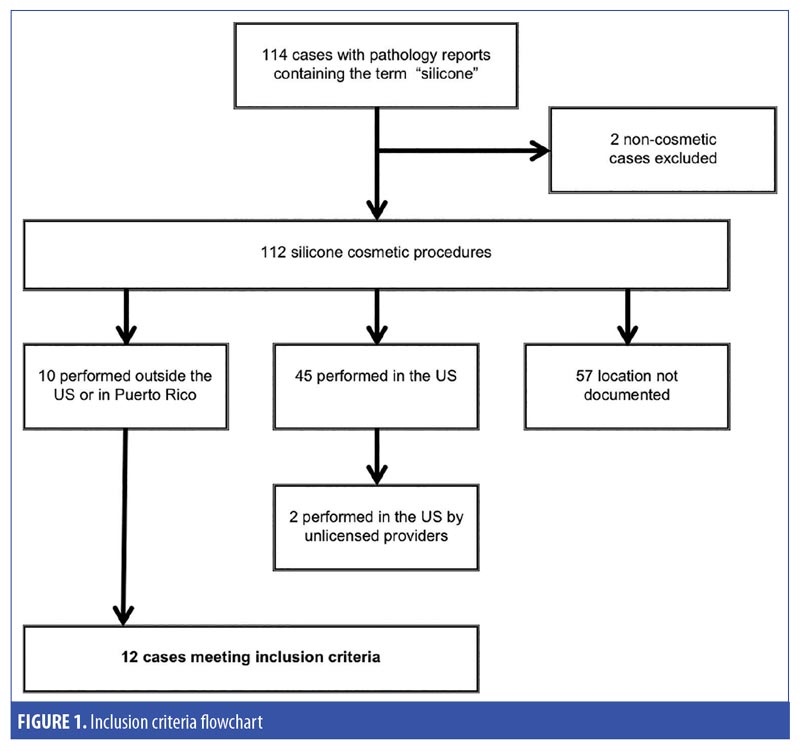
Results
We identified 114 cases with pathology reports that included the term silicone. Two cases involved silicone used in orthopedic and corneal surgeries and were excluded. There were 45 cases of silicone cosmetic procedures performed in the US, including two by unlicensed providers, and 10 cases performed in a foreign country or Puerto Rico. For the remaining 57 cases, the location of the procedure was not documented. Twelve cases met inclusion criteria and are described below (Figure 1).
Demographics. Ten of the study patients were female and two were male-to-female transgender. The median age was 45 years (range: 24–69 years), and all patients were Hispanic. Nine patients had Medicaid or dual Medicaid/Medicare, one had Medicare only, one had private insurance, and one was uninsured. The 12 cases are summarized in Table 1.
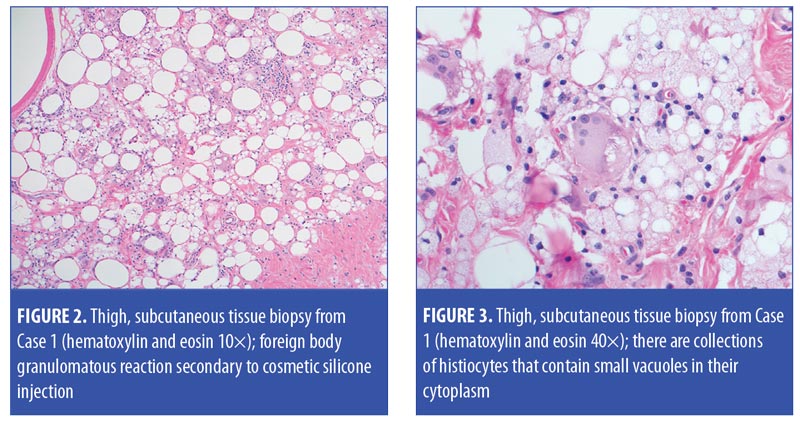
Case descriptions. Case 1. A 47-year-old woman presented with pain in her right thigh. She had visited the emergency room 1 to 2 times a year for the past 10 years due to recurrent right thigh pain and had been treated multiple times for cellulitis and superficial thrombophlebitis. Upon exam, the right thigh was erythematous, tender, warm, and indurated. Laboratory testing was notable for a C-reactive protein (CRP) level of 3.6mg/dL (reference range: 0.0–0.8mg/dL). The erythrocyte sedimentation rate (ESR) was 50mm/h (reference range: 0–20mm/h) and a magnetic resonance imaging (MRI) scan showed edema. Upon further questioning,the patient revealed that the pain began after receiving gluteal free silicone injections by a nonphysician provider in the Dominican Republic more than 10 years prior to presentation. A biopsy of the subcutaneous tissue revealed granulomas in reaction to silicone (Figures 2 and 3). She was followed up by rheumatology as an outpatient but did not receive any treatment.
Case 2. A 55-year-old woman presented with breast pain and swelling, having had silicone breast implants inserted in Guatemala four years previously. On exam, her left breast had an area of tender fluctuance with overlying erythema. Computed tomograpy revealed implant capsule rupture, an adjacent fluid collection, lymphadenopathy, pleural nodules, and a lung granuloma consistent with silicone embolization. She underwent surgical removal of the left breast implant. The abscess culture was positive for methicillin-sensitive Staphylococcus aureus, and she was treated with cephalexin.
Case 3. A 47-year-old woman presented with deformities of both breasts, having received free silicone injections in Puerto Rico more than 10 years prior to presentation. On exam, she was noted to have laterally displaced breasts with diffuse, palpable, fibrotic tissue. A mammogram showed breast tissue completely obscured by silicone and granulomas. She underwent excision of silicone fibrosis and autologous fat grafting. Pathology revealed fat necrosis, fibrosis, and a foreign-body giant-cell reaction. Postoperatively, she underwent an additional revision of breast reconstruction and was able to achieve significant cosmetic improvement.
Case 4. A 44-year-old woman presented with complaints of a lump in her left breast. Three years prior to presentation, she had received silicone implants in Venezuela. Mammography and ultrasound showed a 1.3cm mass. Biopsy revealed fat necrosis and foreign-body giant-cell reaction. She underwent yearly surveillance ultrasounds, which did not show any significant evolution.
Case 5. A 28-year-old woman presented following placement of silicone implants in the Dominican Republic the year before. She reported hardening of her left breast over the previous six months, and, two weeks before presentation, reported feeling a mass in her breast, with pain, erythema, and leakage of fluid. On exam, there was a large area of fluctuance and a fluid wave in the upper pole of the left breast. Ultrasound showed capsule rupture, diffuse edema, hyperemia, and a small fluid collection surrounding the implant. Her laboratory data were notable for an ESR of 125mm/h, ferritin level of 1,450mg/mL (reference range: 10.0–150mg/mL), and CRP level of 7.6mg/dL. The patient underwent drainage of the fluid collection, which was culture-negative and determined to be a seroma. She then underwent bilateral implant removal, during which time, the left implant capsule was found to be ruptured. Pathologic examination of the left capsule showed fibroconnective tissue with granulation and moderate chronic inflammation.
Case 6. A 69-year-old woman presented with red patches on her legs that had been present since she underwent cosmetic injections into her thighs 25 years previously in the Dominican Republic. Exam revealed pink-violaceous, atrophic, crinkling patches on her bilateral hips and thighs. A shave biopsy demonstrated silicone granulomas. Due to the large area of distribution and her lack of pain or other symptoms, her skin lesions were monitored clinically and she did not undergo any therapy.
Case 7. A 47-year-old woman presented with facial scarring. She had received silicone injections into her bilateral cheeks 20 years ago in the Dominican Republic to improve what she believed to be a thin facial appearance. Twelve years after the procedure, she developed acute facial swelling and underwent excision of the injected material, which resulted in severe facial scarring. On physical exam, she had firm and fibrous scarring in the cheeks and perinasal region, with deep troughs. The scarring restricted the motion of her lips and interfered with smiling and speaking. For cosmetic improvement, she underwent tissue expander implantation, cervicofacial flap, and skin grafting. Skin biopsy showed a granulomatous reaction to silicone.
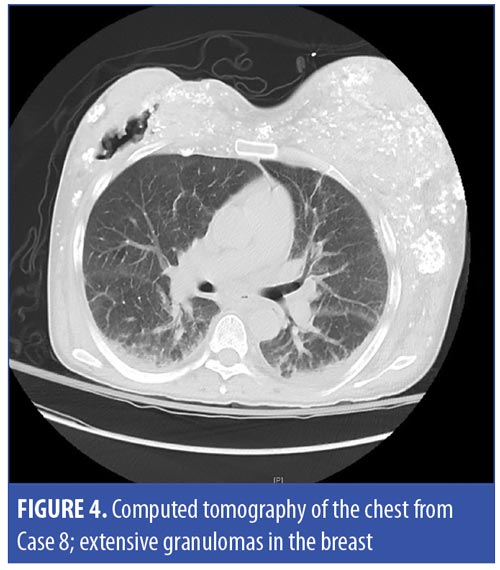
Case 8. A 36-year-old, male-to-female transgender patient with chronic, nonhealing ulcers presented with drainage from a buttock ulcer. Ulcers on her buttocks, hips, thighs, and breasts had been present since receiving free silicone injections eight years earlier in Mexico. She visited the MMC wound care and general surgery clinics regularly and underwent debridement and silicone removal every two weeks. A biopsy of a left hip ulcer taken during her initial debridement revealed necrotic, dense, collagenized tissue, silicone, calcifications, and focal aggregates of bacteria. She also had hypercalcemia secondary to granulomatous disease, which was complicated by nephrolithiasis requiring lithotripsy and ureteral stents, recurrent urinary tract infections, and chronic renal failure. On exam, she had diffuse, palpable, irregular subcutaneous masses and large, deep ulcers on the breasts and buttocks with a foul-smelling discharge. She was hospitalized and administered intravenous antibiotics, and debridement was performed, including a biopsy of a buttock ulcer, which showed granulation tissue. Deep wound culture grew Morganella morganii and Enterococcus faecalis. She had several hospitalizations over the next five years for wound infections, hypercalcemia, acute renal failure, urinary tract infections, and septic shock. Laboratory studies were notable for a CRP level of 8.5mg/dL and ESR of 135mm/h. Subsequent wound cultures grew Pseudomonas aeruginosa and methicillin-resistant Staphylococcus aureus (MRSA).Computed tomography (CT) scans of the chest (Figure 4), abdomen, pelvis, and thighs demonstrated calcified granulomas, soft tissue infiltration, ulcerations, and calcified lymph nodes, likely representing lymphatic drainage of silicone. A gallium scan showed increased tracer uptake in the breasts and buttocks. A bone-marrow biopsy revealed silicone and small granulomas, reflecting embolization of the injected silicone. She ultimately required nephrectomy of her right kidney. Her hypercalcemia improved with chronic prednisone. Multiple providers documented that she appeared guarded, tearful, and embarrassed during encounters. She was referred to outpatient plastic surgery but did not show up to appointments. During an inpatient consultation, she refused to allow the plastic surgery service to examine her, and was eventually lost to follow-up.
Case 9. A 46-year-old male-to-female transgender patient who had received silicone breast implants in Mexico 20 years earlier presented with pain and hardening of her breasts. On exam, both breasts were firm and contracted. She underwent capsulectomy and implant exchange, while pathologic examination showed patchy histiocytic aggregates containing silicone. She had no further complications.
Case 10. A 40-year-old male-to-female transgender patient with a history of human immunodeficiency virus (HIV) infection and cluster of differentiation four-count of 450 cells/uL presented with breast deformities. Twenty-five years earlier, she had received free silicone injections in the Dominican Republic, which was followed by placement of silicone breast implants 10 years later. She developed infection, extrusion, and migration of free silicone into the abdomen, and had the free silicone and implants surgically removed at a US hospital three years prior to seeking treatment at MMC for persistent cosmetic defects. She presented with asymmetric and deformed breasts with loss of the left nipple and copious, palpable, subcutaneous nodules. She underwent debridement of free silicone and subcutaneous nodules, with biopsy showing scarring, extensive fat necrosis with calcification, and abundant histiocytes and chronic inflammation. She subsequently underwent breast implant insertion, reconstruction with bilateral latissimus dorsi flaps, and nipple-areola reconstruction. Pathology showed scar formation, chronic inflammation, and a lymph node with focal noncaseating granulomas and foreign-body giant-cell reaction. After multiple reconstructive surgeries, the patient still had residual silicone that was difficult to excise, and she remained dissatisfied with the cosmetic result.
Case 11. A 24-year-old woman presented with discoloration in her buttocks. Four years prior, she had received free silicone injections to the buttocks from an unlicensed provider in her home in New York. On exam, she had induration and discoloration spanning the buttocks, perineum, and medial thigh. Biopsy of the perineum showed vacuoles surrounded by foam-laden histiocytes consistent with silicone migration. She was referred to dermatology, plastic surgery, and cognitive behavioral therapy, but never came to the appointments and was lost to follow-up. She had also undergone silicone breast implants in Colombia, South America, but had no complications from this procedure.
Case 12. A 44-year-old woman presented with burning, swelling, and itching of the lips. She had undergone free silicone injections to the lips, cheeks, hips, and buttocks 10 years previously in a nonmedical facility in New York. She subsequently suffered complications from the migration of silicone to the labia majora and underwent multiple surgical resections to remove the silicone from the buttocks and perineum. On exam, she had erythema, swelling, and tenderness over her cheeks, lips, labia majora, mons pubis, and buttocks and underwent excision of silicone from these areas. Pathology showed infiltrating foamy macrophages, fat necrosis, and chronic inflammation. She returned two years later with firmness, pain, and deformity in the buttocks. Due to the extent of silicone infiltration, the plastic surgeon advised her that it would not be possible to remove all the silicone and she would likely have recurrent complications.
Discussion
Generalists and specialists should familiarize themselves with complications from silicone procedures among medical tourists. The patients in this series suffered significant morbidity, with symptoms lasting decades, as well as multiple hospitalizations and significant cosmetic deformities. Most of these patients were relatively young and healthy, with few exisiting comorbidities. All of the patients in this case series were Hispanic, and those who had traveled abroad underwent procedures in Latin America, possibly due to the region’s cultural familiarity or geographic proximity to the US. Compared to MMC’s overall patient population, a disproportionate number of these patients had Medicaid, suggesting that cost might be a primary motivator for medical tourism. Although not strictly considered medical tourists, we included patients who underwent procedures performed by unlicensed providers in the US due to the similar risks for complications (Cases 11 and 12). Providers should ask about such procedures, even if there is no history of international travel. In over half of the patients who suffered complications from silicone procedures, the country of procedure was not documented in their patient files, and, we suspect, this information was likely never requested from the patients. Clinicians should be sensitive when inquiring about medical tourism due to potential embarrassment and reluctance to discuss by the patients, which was seen in Case 8.
For clinicians, diagnosing and treating silicone procedure complications in the medical tourist patient can be challenging for many reasons. Not only can a single patient have silicone injection or implants in multiple parts of the his or her body (e.g., face, breasts, buttocks), but the complications can manifest in multiple areas of the body other than the original procedure sites, due to migration (as seen in Cases 10, 11, and 12) or embolization (as seen in Cases 2 and 8). Additionally, complications can present years after the initial procedure, and the association might not be immediately apparent to providers or patients. A range of presentations directly related to previous silicone procedures are possible, including infection, inflammation, scarring, chronic ulcers, implant rupture/contracture, and hypercalcemic granulomatous disease. Laboratory and radiographic studies might show signs of inflammation, such as elevated CRP and ferritin levels and ESR, as seen in Cases 1, 5, and 8, and edema or lymphadenopathy, as seen in Cases 1, 2, and 8. However, findings are often nonspecific and can mimic other, more common conditions. If complications from silicone injection or implants are suspected, biopsy should be obtained and might show reactions to silicone, including inflammation, granuloma, fibrosis, or necrosis.
Once diagnosed, the management of silicone complications is generally difficult. The patient might require multiple excisional and reconstructive surgeries, and the silicone might not be completely excisable if infiltration is extensive, as seen in Cases 10 and 12. Cosmetic deformities might not result from the initial procedure, but from subsequent excisional procedures, as seen in Cases 7 and 10. Some patients are never able to achieve satisfactory cosmetic results, despite multiple corrective surgeries. Recurrent complications requiring multiple hospitalizations and prolonged therapy, such as intravenous antibiotics, are also possible, as seen in Case 8. This high degree of healthcare utilization can add a significant burden on the healthcare system, in general, and on a patient’s morbidity and quality of life, in particular.
Limitations. This study had limitations. Data were limited to the available documentation in the electronic medical records; thus, it is possible we missed cases if the country of procedure was not recorded. Additionally, because only cases with a biopsy report—and, by extension, a complication—were queried, no conclusion regarding the prevalence of complications among medical tourists can be made.
Conclusion
This retrospective chart study is, to our knowledge, the largest case series analysis of complications attributable to cosmetic silicone procedures among patients considered medical tourists. It is our aim that this information will assist clinicians in properly identifying, diagnosing, and treating complications, such as the ones described here following silicone injection and/or implant procedures, in patients who, whether for financial, cultural, or other reasons, chose to undergo cosmetic procedures in another country or by an unlicensed practictioner in the US. It is important that clinicians recognize the considerable and diverse morbidity such patients can experience, as well as understand the importance of treating this unique patient population with sensitivity and empathy to ensure optimal outcomes.
References
- Horowitz MD, Rosensweig JA, Jones CA. Medical tourism: globalization of the healthcare marketplace. MedGenMed. 2007;9(4):33.
- Nguyen D, Gaines J. Medical tourism. Available at: https://wwwnc.cdc.gov/travel/yellowbook/2018/the-pre-travel-consultation/medical-tourism. Accessed May 9, 2018.
- United States Food and Drug Administration. FDA warns against the use of injectable silicone for body contouring and enhancement: FDA safety communication. Available at: https://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm584824.htm. Accessed November 4, 2017.
- Adabi K, Stern CS, Weichman KE, et al. Population health implications of medical tourism. Plast Reconstr Surg. 2017;140(1):66–74.
- Ryu AJ, Glazebrook KN, Samreen N, et al. Spectrum of chronic complications related to silicone leakage and migration. Am J Med. 2018;131(11):
1383–1386. - Cusumano LR, Tran V, Tlamsa A, et al. Rapidly growing Mycobacterium infections after cosmetic surgery in medical tourists: the Bronx experience and a review of the literature. Int J Infect Dis. 2017;63:1–6.
- Cai SS, Chopra K, Lifchez SD. Management of Mycobacterium abscessus infection after medical tourism in cosmetic surgery and a review of literature. Ann Plast Surg. 2016;77(6):678–682.
- Pasternack FR, Fox LP, Engler DE. Silicone granulomas treated with etanercept. Arch Dermatol. 2005;141(1):13–15.
- Paul S, Goyal A, Duncan LM, Smith GP. Granulomatous reaction to liquid injectable silicone for gluteal enhancement: review of management options and success of doxycycline. Dermatol Ther. 2015;28(2):98–101.
- Singh M, Solomon IH, Calderwood MS, Talbot SG. Silicone-induced granuloma after buttock augmentation. Plast Reconstr Surg Glob Open. 2016;4(2):e624.
- Plaza T, Lautenschlager S. Penis swelling due to foreign body reaction after injection of silicone. J Dtsch Dermatol Ges. 2010;8(9):689–691.
- Nasseri E. Gluteal augmentation with liquid silicone of unknown purity causes granulomas in an adult female: case report and review of the literature. J Cutan Med Surg. 2016;20(1):72–79.
- Ellis LZ, Cohen JL, High W. Granulomatous reaction to silicone injection. J Clin Aesthet Dermatol. 2012;5(7):44–47.
- Safyer S. Montefiore Medicine’s 2018–2019 state budget testimony on health policy and Medicaid. Available at: www.montefiore.org/documents/news/2018-2019-State-Budget-Testimony-on-Health-Policy-and-Medicaid-Dr-Steven-Safyer.pdf. Accessed June 29, 2018.
- Chase D. Montefiore Medical Center: integrated care delivery for vulnerable populations. Available at: https://www.commonwealthfund.org/publications/case-study/2010/oct/montefiore-medical-center-integrated-care-delivery-vulnerable. Accessed June 29, 2018.
- United States Census Bureau. QuickFacts Bronx County (Bronx Borough), New York. Available at: https://www.census.gov/quickfacts/fact/table/bronxcountybronxboroughnewyork/PST045217. Accessed June 29, 2018.

