 J Clin Aesthet Dermatol. 2022;15(2):26–29.
J Clin Aesthet Dermatol. 2022;15(2):26–29.
by Anuj Bhatnagar, MD, DNB; Roma Rai, MD; Sanjay Kumar, MS ENT; Barnali Mitra, MD, DNB; Ajay Chopra, MD; Gautam Kumar Singh, MD; Debdeep mitra, MD, DNB; Chetan Patil, DNB; and Sunmeet Sandhu, MD, DNB
Drs. Bhatnagar, Kumar, B. Mitra, Patil, D. Mitra, and Sandhu are with Command Hospital Air Force Bangalore in Bangalore, India. Dr. Rai is with Command Hospital Air Force Pune in Pune, India. Dr. Chopra is with Command Hospital Western Command in Panchkula, India. Dr. Singh is with Base Hospital Delhi Cantt in New Delhi, India.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Introduction. Facial nerve palsy often leads to functional and physiological impairment in patients and they often suffer from social stigma. The use of polydiaxone (PDO) threads has long been used to treat facial furrows and age-related sagging in the face. The basic principle of the thread lift procedure is placing cogged threads in the subcutaneous plane along a planned trajectory. The efficacy and ease of this procedure compared to a traditional face lift has made PDO threads a popular option in the past three decades.
Methods. We treated 50 patients with a drooping face on one side following facial paralysis with thread lifting and botulinum injections to control contralateral hypertrophy and ipsilateral synkinesis. The Facial Grading System or the serial Sunnybrook Facial Grading System (SB scores) was used to assess at all the visits and serial photographs were recorded.
Results. Following the threading procedure, all 50 patients displayed improved facial symmetry. There was significant improvement in the baseline SB scores compared to the scores over following year, with all the scores having significant p value less than 0.05.
Conclusion. Based on our results, subdermal suspension with re-absorbable threads in conjunction with botulinum toxin constitutes an efficient and safe procedure for face lifting and rejuvenation of a drooping face as a result of long-lasting facial paralysis.
Keywords: Facial nerve palsy, botulinum toxin, polydiaxone thread
Facial nerve palsy often leads to functional and physiological impairment in patients and they often suffer from social stigma. This difficulty in expressing facial expressions often leads to a feeling of disappointment, dejection, and depression. One of the most common presentations of long standing facial nerve palsy is dropping of one side of face, which severely affects quality of life.1 This facial asymmetry and drooping of the mouth leads to the inability to smile, and facial expressions can be perceived to be in a constant state of displeasure. The functional impairment can also alter the patient’s eye movements, speech, and ability to chew food. Long-standing, severely injured facial nerve palsy leads to the degeneration of facial muscle fibers. The patient’s eyebrows can descend, nasolabial folds can flatten, wattles and jowls can appear, lips can lose volume, and the neck folds can sag. These changes are often accompanied with hemifacial synkinesis and contractures. The overall facial skin and soft tissues on the affected side becomes loose and saggy. The malar fat pad descends along the inferomedial direction. Overall, there is severe volume loss on the affected side of the face. With these changes, there is associated lengthening of the lower eyelid complex along with pseudoherniation of the orbital fat pad leading to tear trough deformity, flattening of the nasolabial folds, and a prominent nasojugal fold. The affected side appears to have undergone an accelerated aging process compared to the normal side.
The use of polydiaxone (PDO) threads has long been used to treat facial furrows and age-related sagging in the face. It has also been used to achieve a slimmer and slender face. Sulamanidze et al2 introduced the use of barbed sutures for lifting sagging and ptotic facial tissues. The efficacy and ease of this procedure compared to a traditional face lift has made PDO threads a popular option in the past three decades. The basic principle of thread lift procedure is placing of cogged threads in the subcutaneous plane along a planned trajectory. The inserted threads are then pulled to achieve the desired lift and the threads are thereafter secured and snipped close to the skin surface.3 The biggest advantage of this procedure is the ease of the procedure which can be performed under local anesthesia at the point of entry. The side effects can range from bruising to introduction of surface infection.
Among the established methods for restoring facial symmetry post facial nerve palsy thread lift procedure appears the most convenient procedure. Invasive procedures like masseter or temporalis muscle transfer, cross-face nerve grafting and free muscle transfer; although may improve the facial symmetry but are associated with a lot of downtime and several complications. Among the elderly population with long standing facial nerve palsy, loose superficial muscular aponeurotic system (SMAS) layers in the face makes these surgeries contraindicated and less efficacious. Compared to a non-paralyzed face, where there is a possibility of gradual weakening and breaking of the threads due to repeated facial muscle movement, threads inserted in a face affected by paralysis last much longer due to limited muscle movement. Botulinum toxin can also be used on the contralateral normal side to ease out the muscle over activity which the patient inadvertently uses to compensate the paralyzed side.4 This study was designed to evaluate the efficacy and safety of PDO thread face lift technique in patients with facial palsy and facial asymmetry. Long term efficacy and the safety issues were also assessed in these patients.
Methods
Patients. From April 2018 to March 2019, we treated 50 patients with a drooping face on one side following facial paralysis using thread lifting (Aqulift COG Threads-I; Aakaar Medical Technologies, Mumbai, India) and botulinum toxin injections to control contralateral hypertrophy and ipsilateral synkinesis, if required. All patients were informed about the procedure and were enrolled under informed consent. There were 21 women and 29 men with an age range of 21 to 71 years. All patients had unresolved chronic facial paralysis for a minimum of two years. The symptoms included sagging upper eyelid, deviated mouth corner, deepened nasolabial fold induced by facial contracture, descended eyebrow, decreased facial volume, and marked jowls and wattles.
Photographic records were kept before and immediately after the procedure. All the patients after the procedure were reviewed every two months after the procedure for a total of 12 months for observation of clinical results and complications if any.
Procedure. Cogged and monofilaments PDO were used. These threads were designed for cosmetic purposes, including to lift facial skin that shows signs of aging, such as wrinkles and sagging, and to slim down the jawline. To prevent surgical site infection, a betadine scrub preparation was used, and local anesthesia was induced with 1:100,000 adrenaline in the SMAS layers of the involved side with a 26-gauge needle. The site for infiltration was in front of the tragus on the affected site. The needle was used to create a tunnel at the entry point so that the cannula could transit freely. Under local anesthesia, very few patients reported discomfort, anxiety, claustrophobia, pain, or dizziness. No additional sedation or anxiolytic was required in any patient and it was an outpatient procedure. About 4 to 6 cogged threads using a built-in cannula were inserted on the affected side based on the deviation of the face. The cogged threads used were three dimensional 360-degree with multi bi-direction cogs with an attached 21 G 90 mm round-edged needle which was used to minimize the damage of blood vessels.For the drooping of the forehead, eyebrow, eyelid, midface, and the corner of the mouth, 25 to 35 pieces of monofilament threads were used to elevate loose facial muscles under topical anesthesia.
Design is the most fundamental and crucial stage of thread lifting which determines the result of the procedures. Initially the skin is pulled in various directions on patients’ faces, and the key vectors are selected there from (Figure 1). To achieve a mutually satisfying result, sufficient communication is vital during the process.

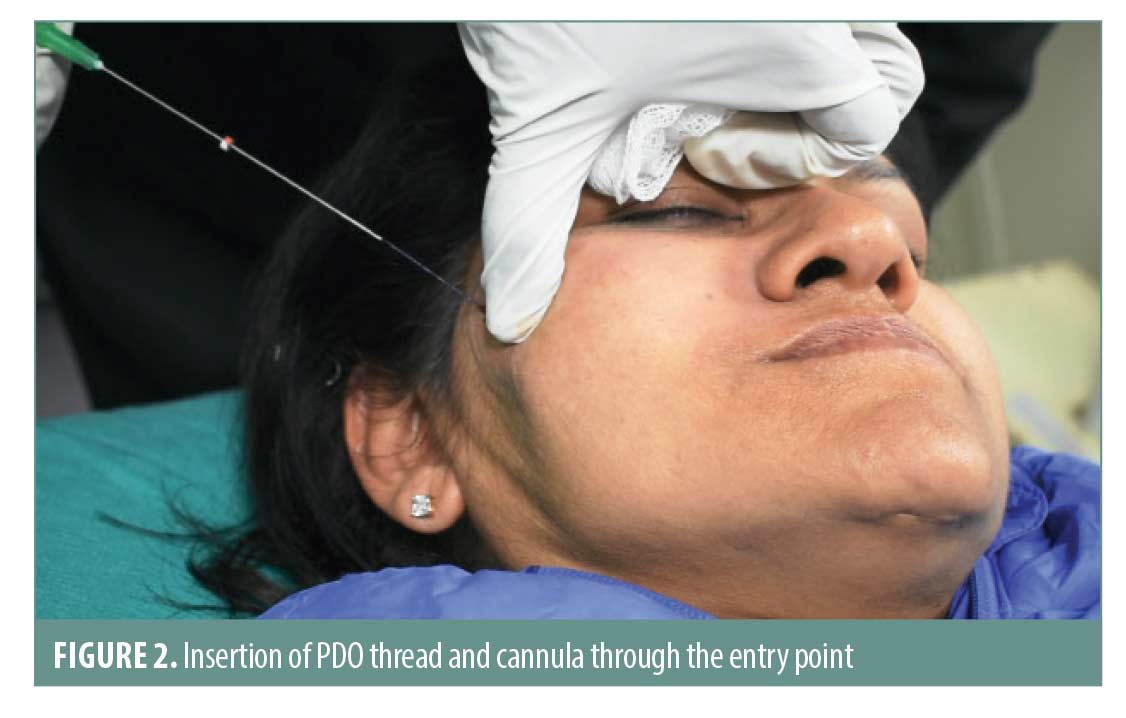
A tumescent anesthesia mixture of 1mL of lignocaine and adrenaline is mixed with 9mL of normal saline and this mixture is infiltrated at the entry point. The entry point is then tunneled using an 18-gauge needle for easy maneuvering of the PDO thread and cannula. After, the cannula is guided in the desired direction, (Figure 2) the cogged thread is anchored in the subcutaneous plane and the cannula is withdrawn, leaving the thread in situ. The tread is placed in the subcutaneous plane and anchored to the adjacent lose areolar tissue using the barbed cogs.
The loose ends are tied in a knot and the ends are snipped with a scissors and the knot is buried inside the entry point (Figure 3). Hence no thread is visible outside and the desired pull or traction has been created. For the drooping of the forehead, eyebrow, eyelid, midface, and the corner of the mouth, 25 to 35 pieces of mono-threads were used to elevate loose facial muscles. Mono threads are plain threads made up of bioabsorbable material (PDO). To manage the sagging upper eyelid, 6 to 8 pieces of thread (30mm) were inserted beneath the eyebrow to tuck the distal cog on the frontalis muscle. To treat laxity of the midface, 8 to 10 pieces of thread (60mm) were inserted on the medial side of the face towards the lateral side to grasp the temporalis muscles at the end of the thread cog. To manage the deviated mouth corner, 12 to 16 pieces of thread (60mm) were inserted at the nasolabial fold, mouth corner, and cheek. This was an average estimate and the number and distribution including choice of thread varied from patient to patient. The contralateral side of the face was injected with botulinum toxin A to decrease facial muscle hypertrophy that usually results from chronic action against the weak antagonism of the weakened muscles and to reduce contralateral muscle strength. The purpose of this treatment is to improve the maintenance of the effect of the inserted thread on the involved side. The average number of injections on the contralateral side was 15.8 ± 6.3, with 1.5–2 units per point. All facial expression muscles or muscle groups on both sides of the face were dynamically examined. An ice pack was applied for vasoconstriction, and topical anesthesia was given prior to injection. Botulinum toxin was injected using a tuberculin syringe with a 27-gauge needle.

Patients were evaluated at baseline and after three, six, nine, and 12 months by the treating physician in person and were not blinded. The Facial Grading System (FGS) is also known as the Sunnybrook Facial Grading System was used to assess at all the visits and serial photographs were recorded. The before and after values were compared using the paired t-test.
Results
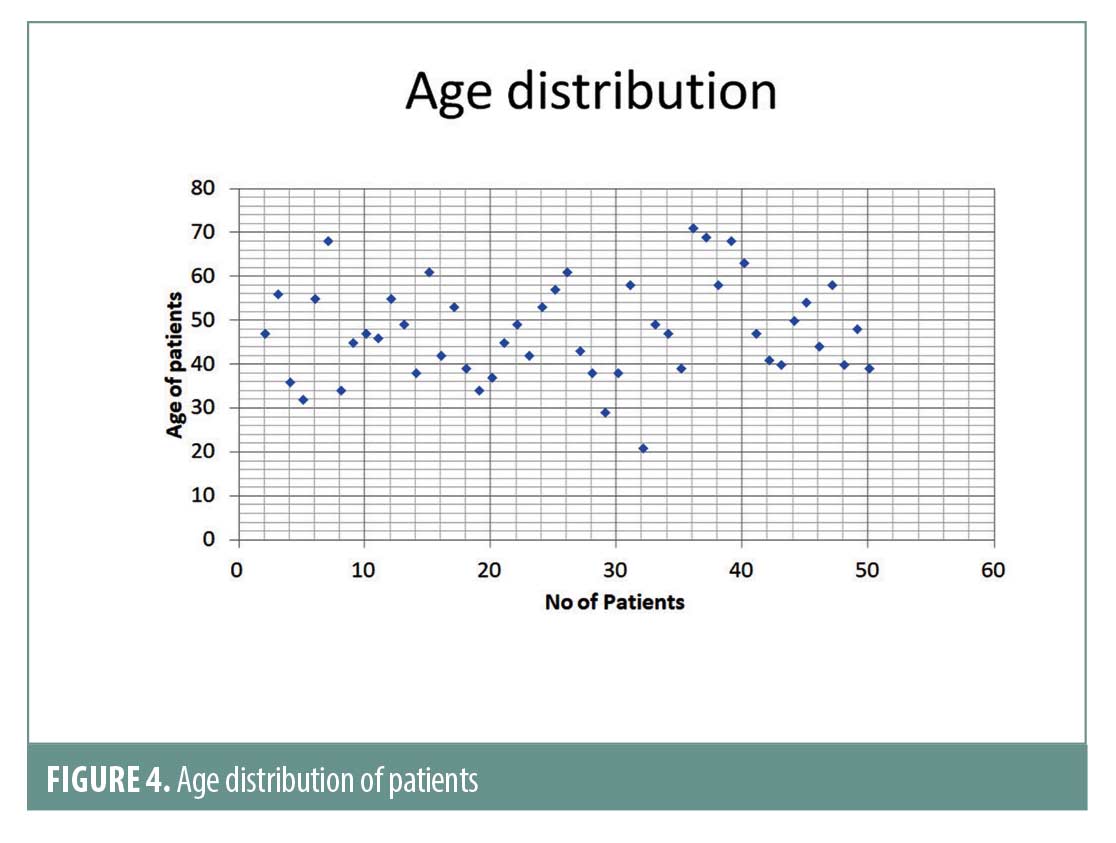
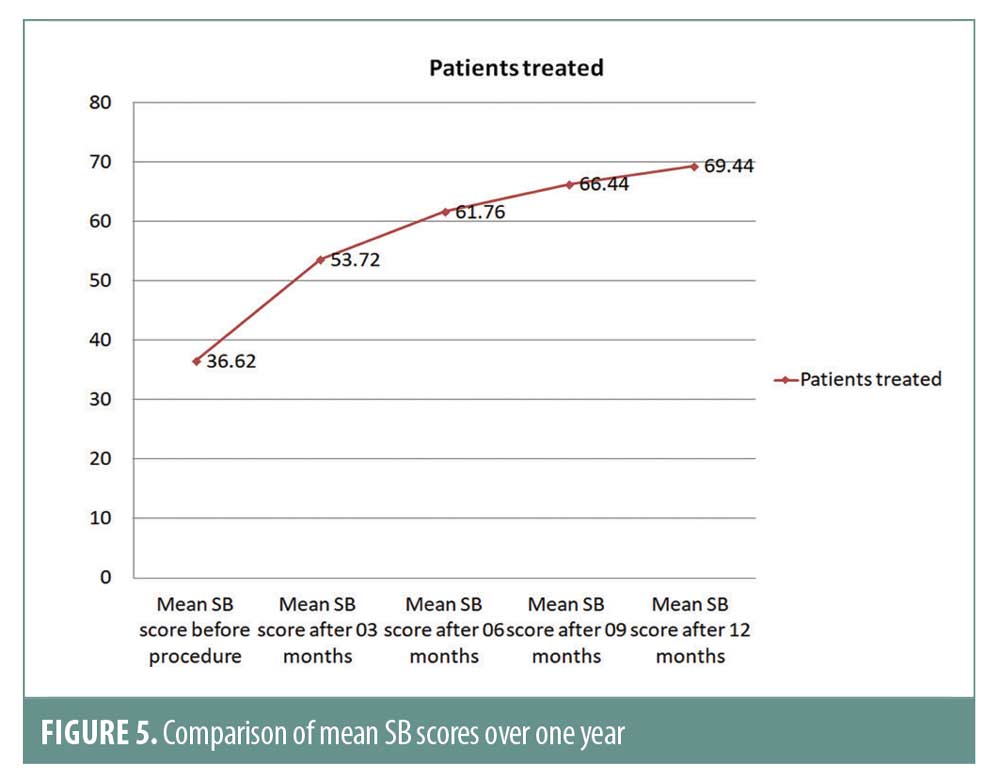
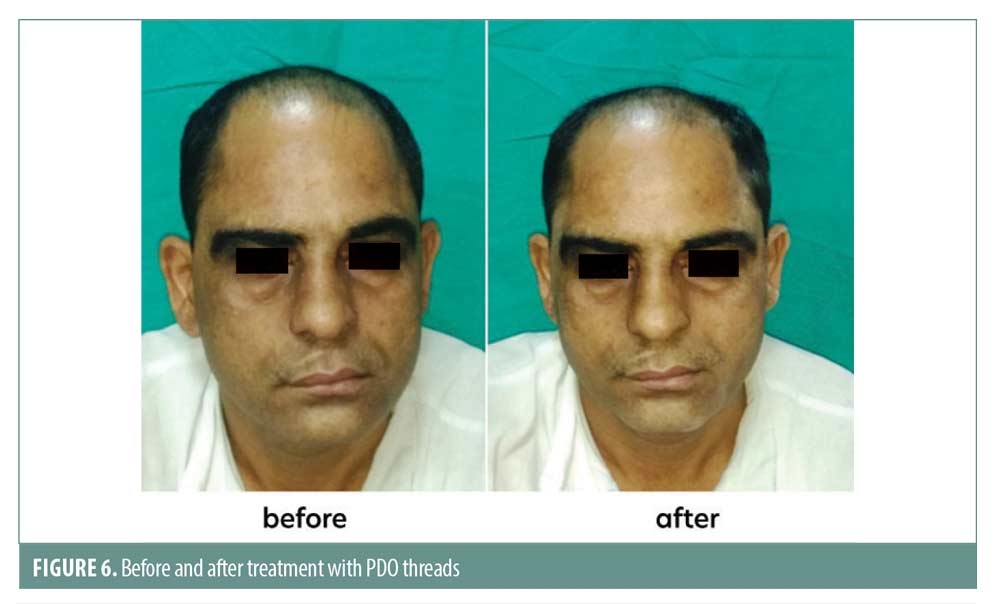
Fifty patients underwent the procedure. The etiology of facial palsy is summarized in Table 1. Following the threading procedure, all 50 patients displayed improved facial symmetry. The patients were able to improve their facial expressions using actions involving their mouth. The mean age of the 50 patients was 47.56 years with a standard deviation of +/- 10.9 years as shown in Figure 4. The Facial Grading System or the serial Sunnybrook Facial Grading System (SB scores) was used to assess at all the visits and serial photographs were recorded. The functionalities that were assessed included the facial symmetry including nasolabial folds, slurring of speech, drooling of saliva and deviation of angle of mouth. The comparison of the facial grading system scores are shown in Table 2 and Figure 5. Before and after images are shown in Figure 6 and 7. All the scores compared to baseline have significant p-value less than 0.05.

Discussion
Facial palsy involves the paralysis of muscles of facial expression supplied by facial nerve. Unilateral palsy leads to impaired facial movements and lack of facial expressions. Unilateral facial palsy in middle aged individuals if further exacerbated by the aging process which leads to herniation of fat pad and sagging of the skin and musculature. Facial paralysis causes progressive soft tissue laxity and loss of subcutaneous volume leading to ptosis of eyebrows, prominence of the orbital rim, flattening of the nasolabial folds and jowl formation similar to the aging process. Unilateral and asymmetrical palsy leads to gross disfigurement of the face. Surgical facelift is an option to correct this asymmetry however it is invasive and has many complications along with a long downtime.5 The use of long lasting absorbable barbed threads has evolved as a viable options for sagging face.6-8 The spines of the cogged PDO threads appear to act as a hook to anchor the thread and cause a tissue reaction promoting neocollagenosis.9 The plugs open like an umbrella lifting up the sagging skin. The immediate effect is lifting of sagging skin due to the effect of the barbed threads. The barbs also act as hooks preventing further sagging or sliding of the supporting tissues. This non-surgical outpatient procedure also has the advantage that over the next year the process of neocollagenosis continues and the overall support structure improves. The PDO threads are supposed to dissolve in about 180 days. This procedure can also be combined with other minimally invasive procedures in the same sitting such as botulinum toxin injection or hyaluronic acid filler on the contra lateral side. The addition of botulinum toxin injection improved the outcome as it led to weakening the overused muscles on the contra lateral side. The contra lateral non-paralyzed side, which acts against the weak antagonism of the contralateral muscles, usually develops facial muscular hypertrophy over time along with facial rhytides, furrows and deviation of angle of mouth.10 Botulinum toxin injection can achieve a balance by partially paralyzing voluntary hypertrophic, non-paralyzed muscles while maintaining facial expression. Each individual patient should be considered on a case-by-case basis because of the marked variation in clinical presentation and duration with diverse histories along with variation in facial muscle strength and anatomy and multiple etiologies of facial paralysis. Although the effects of botulinum toxin may last about six months and the effect of threads may last about 12 to 18 months, the procedures can certainly be repeated.
Conclusion
It appears that subdermal suspension with the re-absorbable thread, in conjunction with botulinum toxin to optimize facial rejuvenation of the contralateral side, constitutes an efficient and safe procedure for face lifting and rejuvenation of a drooping face as a result of long-lasting facial paralysis. We recommend this procedure for patients who do not wish to undergo any invasive treatment after a major surgery due to the fear of additional surgery based on previous experiences. The PDO thread lift is a safe and effective method for patients with long standing facial nerve palsy to attain some degree of facial symmetry.
References
- Bradbury ET, Simons W, Sanders R. Psychological and social factors in reconstructive surgery for hemi-facial palsy. J Plast Reconstr Aesthet Surg. 2006;59:272–278
- Sulamanidze MA, Fournier PF, Paikidze TG, Sulamanidze G. Removal of facial soft tissue ptosis with special threads. Dermatol Surg. 2004;28(5):367–371.
- Abraham RF, DeFatta RJ, Williams EF. Thread-lift for facial rejuvenation: assessment of long-term results. Arch Facial Plast Surg. 2009;11(3): 178–183.
- Choi KH, Rho SH, Lee JM, Jeon JH, Park SY, Kim J. Botulinum toxin injection of both sides of the face to treat post-paralytic facial synkinesis. J Plast Reconstr Aesthet Surg. 2013;66(8): 1058–1063.
- Chaffoo RA. Complications in facelift surgery: Avoidance and management. Facial Plast Surg Clin North Am. 2013;21:551–558.
- Lycka B, Bazan C, Poletti E, Treen B. The emerging technique of the antiptosis subderma suspensionthread. Dermatol Surg. 2004;30: 41–44
- Isse NG, Fodor PB (2005) Elevating the midface with barbed polypropylenes utures. Aesthet Surg J. 2005;25:301–303
- Lee S, Isse N. Barbed polypropylene sutures for mid face elevation. Arch Facial Plast Surg. 2005;7:55–61
- Wu WTL (2004) Barbed sutures in facial rejuvenation. Aesthet Surg J 24:582–587
- Cooper L, Lui M, Nduka C. Botulinum toxin treatment for facial palsy: A systematic review. J Plast Reconstr Aesthet Surg. 2017;70(6):833–841

