J Clin Aesthet Dermatol. 2023;16(9):33–37.
J Clin Aesthet Dermatol. 2023;16(9):33–37.
by Fathia M. Khattab, PhD; Mai A. Samir, MD; Shaimaa S. El Khouly, MSc; and Enayat M. Atwa, MD
All authors are with the Department of Dermatology, Venereology and Andrology, and Faculty of Medicine at Zagazig University in Zagazig, Egypt.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Polycaprolactone (PCL) threads are a novel treatment option for promoting collagen production and smoothing the skin.
Objective. This study aimed to compare the efficacy and safety of threads versus microneedling with autologous platelet-rich plasma (PRP) in the treatment of atrophic acne scars.
Methods. The study included 24 patients (12 females, 12 males) aged 20 to 37 years with atrophic acne scars. Each patient was treated in a split-face manner; a microneedling pen device was used to treat the right side with microneedling and PRP, whereas the left side was treated with threads. Four microneedling plus PRP sessions were used to treat the right side and a single session of threads was used on the left side. For scoring, a global scarring grading system was utilized. Patients were evaluated every three months following the conclusion of treatment. A six-month follow-up was conducted.
Results. Significant clinical improvement was observed in 95.8 percent of the patients on the threads-treated side of the face and in 83.3 percent of the patients on the microneedling plus PRP side. Patient satisfaction was significantly greater in the threads group than in the microneedling+PRP group (p<0.0001). The side effects were tolerable and transient.
Conclusion. Based on our results, we conclude that both threads insertion and microneedling with autologous PRP can yield satisfactory results with minor side effects (fine edema and erythema) that resolve rapidly.
Keywords. Microneedling, platelet-rich plasma, atrophic acne, threads
Acne scars result in physical changes, limit daily activities and self-esteem, and have secondary adverse effects such as depression and anxiety. An increasing number of individuals prefer therapy to overcome these adverse effects.1–4
Acne scars can be hypertrophic or atrophic. The atrophic scars are more prevalent and subdivided into ice picks, boxcars, and rolling scars.5–6 Atrophic scars are caused by dermal collagen disintegration.1
Despite the fact that numerous therapy methods are currently utilized, there has been some advancement with potentially negative side effects. There is no perfect treatment for acne scars. Therefore, modern therapy methods are continually under investigation.7,8
Chemical peeling, dermabrasion, ablative and non-ablative laser resurfacing, the insertion of fillers, and surgical procedures can be used to treat acne scars. Depending on the type and severity of the scar, a specific approach is required to achieve satisfactory results.9
Microneedling has emerged as a significant type of acne scar therapy. The underlying principle of microneedling with microneedles, which induces minor dermal damage, is collagen synthesis. The needles are so small that almost no tissue damage occurs.10
Autologous PRP contains a high number of platelet growth factors. Activation platforms release various growth factors and cytokines, enhancing skin regeneration and local action to increase the synthesis of proteins and collagen, endothelial migration, or angiogenesis. In addition, it is responsible for decreasing the scars in this collagen deposition.11
Thread lifting is a minimally invasive facial rejuvenation procedure. These methods can aid in the lifting of sagging skin. Absorbable threads are a novel method for supporting and extending facial and body tissues. Absorbable barbed sutures may provide a viable alternative to more aggressive surgical techniques. As a treatment for acne scars, absorbable threads that promote tissue regeneration via fibroblast activation have been proposed. 5
The current study aimed to assess the efficacy and the safety of threads versus microneedling with autologous PRP in the treatment of atrophic acne scars.
Methods
This comparative study was conducted between March 2021 and March 2022 at the Outpatient Clinics of the Dermatology, Venereology, Andrology Department, Faculty of Medicine, Zagazig University Hospitals. The study included 24 patients (12 females and 12 males) with atrophic acne scars aged 20 to 37 years. The duration of the scars ranged from 2 to 10 years. The Institutional Review Board (IRB) at Zagazig University approved the study.
A full history was obtained for each patient, including a history of previous medication, previous treatment of the scarring (e.g., laser, PRP, peeling, subcision, or other procedures), surgery, and history of drug intake (retinoids and anti-coagulants).
Exclusion criteria included patients with keloids or hypertrophic scars, active skin disease (other than mild acne, skin neoplasia, skin infection, and collagen), an active systemic or local skin disease could change wound healing, cases that underwent or were scheduled for treatment with injecting fillers or ablative or non-ablative laser resurfacing, medication with isotretinoin, or other oral retinoids within the past six months.
All subjects were evaluated using a qualitative global scarring grading system12 by two blinded physicians who evaluated photographs taken at baseline and every three months after the end of treatment.12 The physicians evaluated the improvement using a quartile grading scale (excellent improvement >75%, very good improvement [50%–74%], good improvement [25%–49%], and mild improvement [<25%]). To evaluate patient satisfaction, patients were asked to rate their satisfaction with their scars three months after the final session of threads, as well as treatment outcome (not satisfied [0%–24%], slightly satisfied [25%–49%], satisfied [50%–74%], or very satisfied [75%–100%]). Patient-perceived pain was also assessed using a visual analog scale: 1–3=mild, 4–6=moderate, and 7–10=severe.
All routine blood analyses were performed in the hospital laboratory, including a complete blood picture using automated Sysmex XN 2000 prior to PRP and platelet count following PRP, as well as the international normalized ratio (INR) (prothrombin time test).
Before treatment, all patients provided informed consent. Patients were asked about their concerns, objectives, and expectations regarding the treatment. The side effects of each technique, such as pain, edema, erythema, and hyperpigmentation, were illustrated for all participants.
Each patient was treated in a split-face manner; a microneedling pen (Dr. Pen ULTIMA-A6) device was used to treat the right side with microneedling and PRP with a one-month interval between each session for four sessions, while the left side was treated with threads in a single session. Patients were assessed three months after the last visit. The follow-up duration was six months.
Treatment of the right side of the face by microneedling and autologous PRP. The PRP was prepared using the double spin technique. In each patient, 10mL of blood was collected in sodium citrate-coated tubes. The tubes were then centrifuged at 1000rpm for 10 minutes. The supernatant plasma layer was collected in fresh tubes and centrifuged for 15 minutes at 3000rpm. The bottom part of the tube was collected (PRP).
Microneedling was performed perpendicularly, rolling was done five times each in the horizontal, vertical, and diagonal directions with the other hand. The treatment endpoint was identified as uniform pin-point bleeding that was easily controllable. A total of four passes with the microneedling pen were used during this session. In addition to microneedling, PRP was injected with subcutaneous blebs of PRP.
Gentle massaging was done before the procedure, followed by a topical antibiotic for approximately 45 to 60 minutes. After sterilization with alcohol, every patient received PRP by microneedling using a microneedling pen.
Topical and systemic antibiotics and anti-inflammatory medications were prescribed five days after treatment, along with instructions to patients to decrease exposure to the sun and apply sunscreen when going outdoors.
Treatment of the left side of the face by threads. In one session, monofilament polycaprolactone (PCL) threads were inserted on the left side of the face, while the right side received microneedling with PRP. After applying a topical anesthetic cream to the left side of the face for one hour, the area was cleaned with a 70% alcohol solution. Four monofilament threads were inserted in the dermal layer, two in a transverse line and two vertically, to form a mesh or net, similar to the cross-hatching technique.
Statistical analysis. Data collection and analysis were done utilizing the SPSS software (Version 23.0. Armonk, NY: IBM Corp). Quantitative data were expressed as mean SD & median (range), and quantitative information was presented as a pair of numbers and percentages. It was used to compare two sets of normally distributed data using the t-test of significance. Non-normally distributed variables were compared using the Mann-Whitney U test of significance. Chi-square and Fisher’s exact tests were used to compare percentages of categorical variables. The level of statistical significance was set at a p-value of ≤0.05.
Results
Patients were categorized (12 females and 12 males), with ages ranging from 20 to 37 with a mean of 26.6±4.9 years. 33.3 percent of patients were students and specialists, while 16.7 percent were housewives and workers. Nine of the 24 patients had significant sun exposure (37.5%), five had other skin diseases (20.8%), 17 had a family history of acne scar (70.8%), and five were smokers (20.8%); the predominant skin type was Type III. Scars ranged in age from 2 to 10, with a mean of 4±2.6 years. Among the studied patients, eight (33.3%) had experienced an acne flare within the past month. All patients had rolling scars that might be associated with another scar type, primarily boxcar scar, and 19 patients (79.2%) had previously received treatment for acne scars, mainly with topical treatment, followed by isotretinoin (Table 1).
Three months after the last session of microneedling+PRP, there was a statistically significant improvement in the acne grading scale. The disparity between the two sides was insignificant. Regarding Grade IV showed an improvement to Grade III and Grade II (on both sides (p=0.0001) (Table 2).
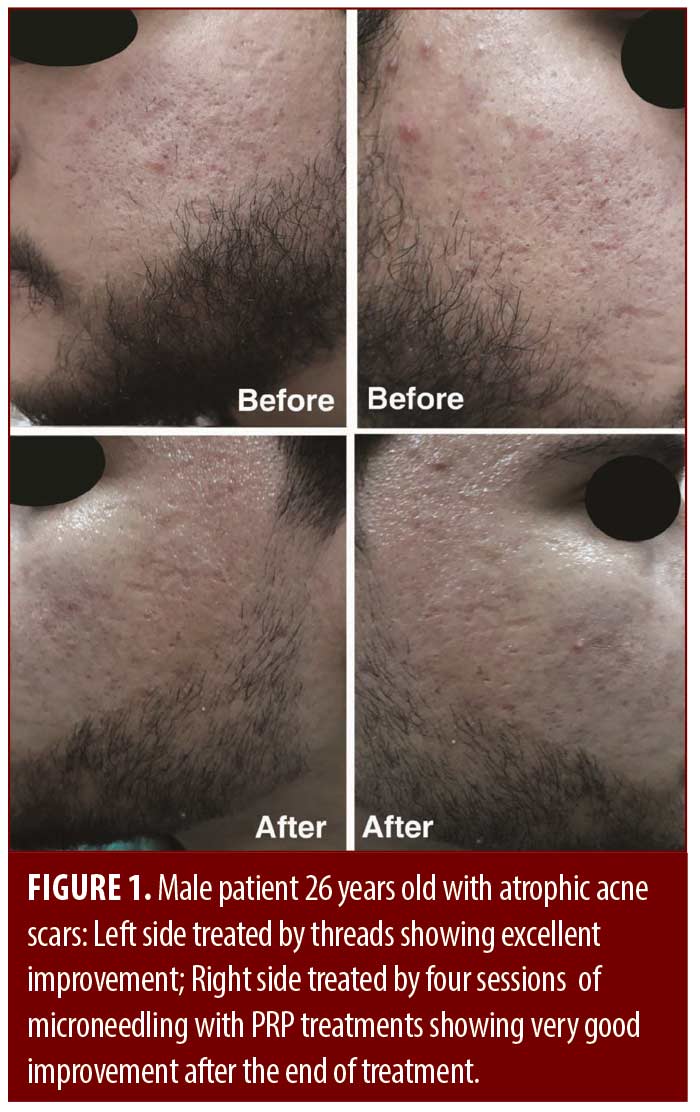
The physician’s assessment showed excellent improvement in acne scarring in 83.3 percent of the side of the threads and 58.3 percent in the microneedling+PRP side (p<0.0001) (Table 3). Regarding patient satisfaction, both groups reported high levels of satisfaction (p<0.0001) (Table 3). Mild edema, pain, and ecchymosis were observed, with no significant differences between groups (p=0.21) (Table 3). Concerning the type of scars and scars severity, the results were higher with rolling and moderate types of acne scars but with no significant difference. Photo documentation is presented in Figures 1 and 2.
Discussion
Our clinical study recruited 24 patients with atrophic acne scars. All patients completed the study. The left side of the faces of all study participants was treated with threads in a single session. The right side of the faces of all study participants was treated with microneedling and autologous PRP (4 sessions, one month apart), with a six-month follow-up.
Twenty-four patients (12 female, 12 male) participated in the study. Regarding scarring grades for the right side of the face in all patients, there were three patients (29.2%) with Goodman and Baron Grade II, 12 patients (50.0%) with Grade III, and nine patients (37.5%) with Grade IV. On the left side of the faces of all patients, two patients (8.4%) had Grade II, ten patients (41.6%) had Grade III, and 12 patients (50.0%) had Grade IV scarring. All patients with rolling scars may also have other types of scars, primarily boxcar scars. The age of scars ranged from 2 to 10, with a mean of 4±2.6 years. The predominant skin type of the patients, according to the Fitzpatrick scale, was Type III. Before treatment, there was no significant difference between the acne scars on both sides, with p>0.05. Compared to the microneedling with PRP treatment side, the improvement of atrophic acne scars for the threads treatment side was significantly greater (p=0.0001), but there was no significant difference compared to the microneedling with PRP treatment side (p=0.0001). Overall improvement of 95.8 percent of threads was improved compared to 83.3 percent of patients after the microneedling pen device with PRP.
To our knowledge, this is the first study comparing these two modalities to manage atrophic acne scars.
Regarding satisfaction, the study by Nassar et al,14 demonstrated that the satisfaction of cases was higher in the combined groups compared to the subcision alone (p<0.0001). In the hyaluronic acid group, 100 percent of patients were satisfied or very satisfied, compared to 70 percent in the monofilament threads group. There were no statistically significant differences in patients’ satisfaction regarding treatment modalities for both sides p>0. 05.
Elrefaei et al15 found that eight (53.3%) patients were very satisfied, six (40%) were satisfied, and one (6.7%) was slightly satisfied with poly-L-lactic acid (PLLA) threads for the treatment of acne scarring. In contrast, our patients were extremely satisfied with threads (83.3%). Cobo et al13 illustrated that patient dissatisfaction with PLLA threads was greater than with subcision.
Patel et al10 conducted a study on 34 patients comparing the efficacy of microneedling, alone and with PRP, for atrophic acne scarring. On the right and left sides of the face, Goodman and Baron’s baseline mean dropped from 2.72±0.45 to 2.2± 0.4 and 2.37 ±0.5, respectively. The mean physician satisfaction score was two. Findings showed a score of 16±0.79 on the right side and 1.91±0.8 on the left side of the face. The results are comparable to our results on the right side, with a combination of microneedling and PRP.
Amer et al16 investigated the efficacy of microneedling alone and in conjunction with PRP or HA in the treatment of atrophic acne scars. They reported that 41 patients (aged 20 to 40) demonstrated a improvement following both therapies. Following therapy, improvement was 82.9 percent on the left side (HA) and 85.4 percent on the right side (PRP), with no statistically significant differences between groups (P>0.05). Their recorded efficacy or combination of microneedling with autologous PRP is consistent with our study results. In accordance with the current study, Tirmizi et al1 performed a study on 50 patients to assess microneedling treatment for atrophic post-acne scars. A total of three sessions divided into four weekly intervals were conducted. After three sessions, the acne grade was significantly decreased from III to II. Cases with Grade II increased after three months compared with before treatment (p=0.009), and cases with Grade III decreased (p=0.045). A increased proportion of patients with moderate acne scars, as compared to severe, were in Grade II (77.3% vs. 22.7%; p<0.001).
After threads and microneedling with autologous PRP treatment, there is a significantly higher value of improvement of atrophy acne scar for threads treated side compared to baseline (p=0.0001). However, there was no statistically significant difference between the microneedling and PRP treatment groups (p=0.0001). This difference in patient satisfaction and clinical improvement may be due to the patient’s high expectations that multiple microneedling sessions with PRP are superior to a single-thread insertion session.
Patient satisfaction and scar improvement remain the primary objectives when treating acne scars. In the current study, the patients were satisfied with the immediate improvement in the appearance of the scarring. difference between physician-reported outcomes and patient-reported outcomes as patient annoyed with increased number of sessions and multiples procedures. Regarding side effects, treatments were well tolerated and revealed stable results at the follow-up.
With respect to the safety assessment of therapeutic techniques in the present study, there was an agreement with previous studies that reported by previous studies1,10,14,15 that there were no remarkable side effects observed in our study among the patients, such as persistent post-inflammatory hyperpigmentation, persistent erythema, herpes labialis flare-up, scarring, or keloid formation. In all cases, only temporary mild edema and erythema were evaluated and resolved within 2 to 5 days of treatment. There was no statistical difference between the two treatment modalities regarding adverse effects (p>0.05).
Conclusion
Threads insertion and combined microneedling with autologous PRP can provide satisfactory results for patients, with minimal side effects that resolve rapidly.
References
- Tirmizi SS, Iqbal T, Mansoor M, et al. Role of Microneedling in Atrophic Post-Acne Scars: An Experience from a Tertiary Care Hospital. Cureus. Published online January 8, 2021.
- Fife D. Practical evaluation and management of atrophic acne scars: Tips for the general dermatologist. J Clin Aesthetic Dermatol. 2011;4(8):50–57.
- Kim J. Topographic computer analysis for acne scar treatment on face accompanying biopsy study after dermal injection of hydrotoxin mixture. J Cosmet Dermatol. 2021;20:75–83.
- Huang IH, Huang YC. Comment on “Platelet-rich plasma and its utility in the treatment of acne scars: A systematic review.” J Am Acad Dermatol. 2020;82(1):e29–e32.
- Jameson JL, Kasper DL, Longo DL, et al. Https://T.Me/MBS_MedicalBooksStore.; 2018.
- Carlavan I, Bertino B, Rivier M, et al. Atrophic scar formation in patients with acne involves long-acting immune responses with plasma cells and alteration of sebaceous glands. Br J Dermatol. 2018;179(4).
- Gulanikar A, Vidholkar R. Efficacy of platelet-rich plasma in acne scars. Clin Dermatol Rev. 2019;3(2):109.
- Sitohang IBS, Sirait SAP, Suryanegara J. Microneedling in the treatment of atrophic scars: A systematic review of randomised controlled trials. Int Wound J. Published online February 3, 2021:iwj.13559.
- Kolcheva PS, Talybova AM, Stenko AG. Innovative methods in treatment of patients with atrophic post-acne scars. Med Alph. 2020;(6):47–51.
- Patel Y, Parmar B, Umrigar DD. A Comparative Study of Microneedling Alone Versus Along with Platelet-Rich Plasma in Acne Scars. Int J Sci Res. Published online 2020:63–64.
- Porwal S, Chahar YS, Singh PK. A comparative study of combined dermaroller and platelet-rich plasma versus dermaroller alone in acne scars and assessment of quality of life before and after treatment. Indian J Dermatol. 2018;63(5):403–408.
- Goodman GJ, Baron JA. Postacne scarring–a quantitative global scarring grading system. J Cosmet Dermatol. 2006;5(1):48–52.
- Cobo R. Use of polydioxanone threads as an alternative in nonsurgical procedures in facial rejuvenation. Facial Plast Surg. 2020;36(4):447–452.
- Nassar A, Elkashishi K, Artima AY, et al. Updated treatment of Atrophic Acne Scars. Zagazig Univ Med J. 2021;0(0):0-0.
- Elrefaei NMH, Mohamed W, El Attar YA, et al. Comparative study between the efficacy of subcision versus subcision with poly-L-lactic acid threads in facial atrophic scar treatment. Published online 2021.
- Amer A, Elhariry S, Al-Balat W. Combined autologous platelet-rich plasma with microneedling versus microneedling with non-cross-linked hyaluronic acid in the treatment of atrophic acne scars: Split-face study. Dermatol Ther. 2021;34(1).