 J Clin Aesthet Dermatol. 2023;16(6):55–58.
J Clin Aesthet Dermatol. 2023;16(6):55–58.
by Aislyn Oulee, MD; Grace S. Ahn, MD; Sogol S. Javadi, BS; and Jashin J. Wu, MD
Dr. Oulee is with the University of California Riverside School of Medicine in Riverside, California. Dr. Ahn is with the University of California San Diego School of Medicine in La Jolla, California. Ms. Javadi is with the David Geffen School of Medicine at the University of California in Los Angeles, California. Dr. Wu is with the Department of Dermatology at the University of Miami Miller School of Medicine in Miami, Florida.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Phototherapy has gained popularity in the recent decades for the treatment of various immune-mediated dermatological conditions since it is more-cost effective and less toxic compared to systemic therapies. This systematic review aims to inform dermatology providers of the risks and benefits of phototherapy, especially in patients at risk for malignancies. Ionizing energy from phototherapy results in DNA photolesions, namely of cyclobutane pyrimidine dimers (CPDs) and 6-4 photoproducts (6-4PPs). Without adequate repair, these mutations increase the risk for carcinogenesis. Additionally, phototherapy can also indirectly cause DNA damage through the formation of reactive oxygen species (ROS), which damage of several structural and functional proteins and DNA. When choosing a phototherapy modality, it also important to take into consideration the side effect profiles associated with each modality. For instance, a 10-fold higher dose of NB-UVB is required to produce a similar amount of CPDs compared with BB-UVB. Patients who undergo UVA with psoralen (PUVA) can be susceptible to developing skin malignancies up to 25 years after receiving their last treatment. It would behoove providers to consider optimal radiation dosage given each patients’ level of skin pigmentation and potential for photoadaptation. Additionally, there are measures have been proposed to minimize deleterious skin changes, such as a 42-degree Celsius heat treatment using a 308nm excimer laser prior to UVB phototherapy and low frequency, low intensity electromagnetic fields along with UVB. However, as performing routine skin exams, remain paramount in the prevention of phototherapy-induced neoplasia. Keywords. DNA damage, UV radiation, phototherapy, carcinogenesis, PUVA, NB-UVB, BB-UVB
Phototherapy is a type of treatment that primarily utilizes ultraviolet radiation (UVR) that has been used for over a century to treat various dermatological diseases.1 Current phototherapy modalities include broadband UVB (290-320 nm), narrowband UVB (311-313 nm), 308 nm excimer laser, UVA-1 (340-400 nm), and UVA with psoralen (PUVA).2 Phototherapy has become increasingly popular, with a 5 percent annual increase in the overall volume of phototherapy services billed to Medicare from 2000 to 2015.3 Some of the most common dermatological conditions that have been effectively treated by phototherapy include immune-mediated skin diseases such as psoriasis, atopic dermatitis, and vitiligo.4,5 Although these conditions have different etiologies and clinical manifestations, immune system dysregulation plays a key role in the development of all these conditions.6–8 Phototherapy is also effective in treating rare diseases such as mycosis fungoides and scleroderma.4 Topical and systemic treatments are also available for the treatment of include immune-mediated dermatological conditions, however; both treatment modalities possess significant limitations. Systemic immunomodulators for the treatment of psoriasis are expensive, with annual costs ranging from $1,197 to $27,577.8 Systemic therapies have also been associated with severe systemic toxicity, such as hepatotoxicity, nephrotoxicity, and severe infection.9,10 Topical therapies are only indicated for individuals with localized disease, rendering them less effective than the existing systemic therapies.11 A powerful treatment option is phototherapy, which is associated with less systemic side effects and lower annual costs than immunomodulators and is more effective than topical treatments.9 Phototherapy exerts its therapeutic effects on autoimmune and autoinflammatory diseases by inducing apoptosis of proinflammatory cells and activating immunoregulatory mechanisms.12 Common side effects associated with phototherapy include sunburn, erythema, and edema.13 Chronic side effects include lentigines, photoaging, and skin cancer.4 Herein, we present a systematic review of recent literature summarizing the known consequences of phototherapy, which include DNA damage and induction of malignancies, to better understand this increasingly popular treatment modality.
Methods
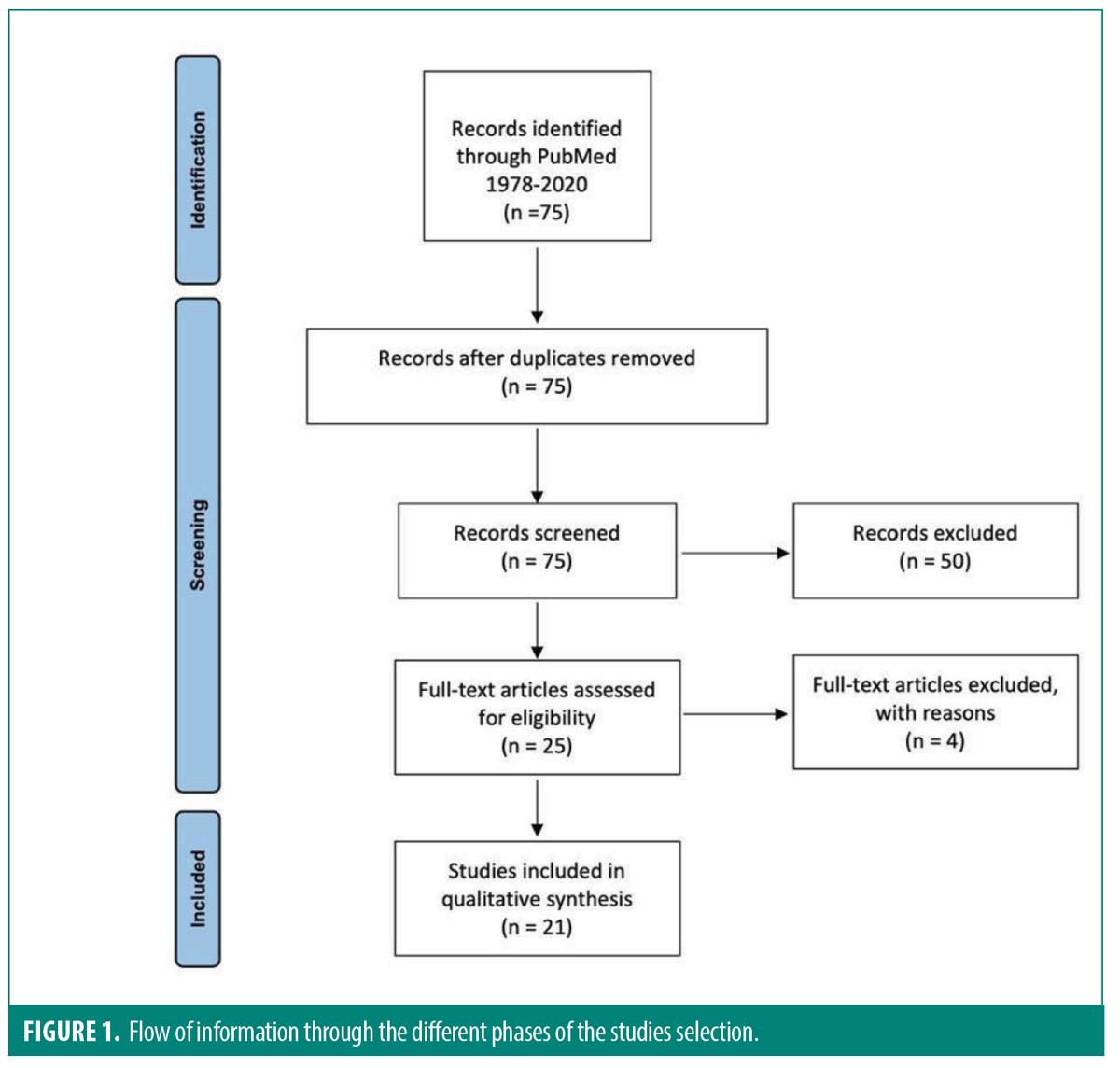
This systematic review was conducted according to PRISMA guidelines. A literature search was conducted using the bibliographical databases PubMed/MEDLINE in August 2021 using the following search terms: “(Phototherapy[Title/Abstract]) and (DNA damage[Title/Abstract])” according to PRISMA reporting guidelines for systematic reviews. All available studies prior to August were considered for inclusion. Given the focus of this article, the inclusion criteria were: (1) relevant studies discussing DNA/cellular damage in adults undergoing/who underwent phototherapy and (2) articles describing the mechanisms of DNA damage/skin cancer caused by phototherapy/UVR. Exclusion criteria included studies written in languages other than English with no translation available, articles not pertaining to both phototherapy and DNA damage, and articles discussing the effects of UVR in neonatal hyperbilirubinemia. Only studies including dermatological conditions as indications for phototherapy were included in this review since phototherapy is often administered for longer time periods and at higher frequencies/doses for the treatment of chronic dermatological disease compared to the treatment of neonatal hyperbilirubinemia, which is a transient condition occurring many newborns. Additionally, the main goal of this review is to bolster dermatologists’ ability to weigh the risks and benefits of phototherapy in patients who are more at risk for malignancy and/or increased comorbidities.
Results
A total of 75 non-duplicated article citations were reviewed; 21 articles (Figure 1) met the inclusion/exclusion criteria. Although phototherapy has been an effective tool in treating a variety of dermatological conditions, it can cause DNA damage and has been linked to increased risk of carcinogenesis. Upon UVR penetration into the skin, its ionizing energy is absorbed by different molecules, DNA being one of them.14 The absorption of this energy by DNA leads to the formation of photolesions, which mainly consist of cyclobutane pyrimidine dimers (CPDs) and 6-4 photoproducts (6-4PPs).15 These mutations can lead to errors in DNA replication which can then lead to the initiation of skin carcinogenesis if not repaired.16,17 CPDs are exclusively seen with UVR-induced DNA damage and their accumulation results in immunosuppression and skin-tumorigenic gene mutations.18 The immune system is responsible for the destruction of UV-induced skin malignancies and therefore immunosuppression can predispose individuals to development of malignancies.14 CPDs are mainly repaired through nucleotide excision repair but some dimers escape repair even in healthy individuals.14,19 6-4PPs trigger the activation of the ataxia telangiectasia and Rad3-related (ATR) pathway which helps ensure the survival of DNA-damaged cells.6 The ATR pathway has been linked to UV tumorigenesis due to accumulation of mutations. Its inhibition is associated with the suppression of UV-induced tumor development.20 Another mechanism by which UVR can lead to carcinogenesis is through mutations to the p53 tumor suppressor gene.13 The p53 tumor suppressor gene, also known as the guardian of the genome, blocks DNA replication if DNA is damaged.21 Therefore, UVR predisposes individuals to malignancy not only by directly creating DNA mutations but also by inhibiting a major genome defense mechanism.
Phototherapy dosimetry is toxicity-limited, and each phototherapy modality is associated with a different degree of carcinogenic side effects. Narrowband UVB (NB-UVB) has been shown to be more effective in the treatment of psoriasis than broadband UVB (BB-UVB) and less cytotoxic and genotoxic than both UVC and BB-UVB per absorbed dose.22,23 A study examining the effects of UVB in organ-cultured human and mouse skin revealed that a 10-fold higher dose of NB-UVB is required to produce a similar amount of CPDs compared with BB-UVB. However, this higher dose of NB-UVB is also associated with a 1.5 to 3 times increased production of 8-oxo-7,8-dihydro-2′-deoxyguanosine (8-oxodGuo), a marker of oxidative DNA damage, compared to BB-UVB.24 Additionally, irradiation of cultured lymphoblasts and keratinocytes with NB-UVB produced very little DNA damage whereas the same dose of BB-UVB resulted in severe damage. Both UVB sources exhibited dose-dependent DNA damage.25 In contrast, an earlier study revealed significant higher CPD formation and ratio of malignant skin tumors in mice following NB-UVB compared to BB-UVB at the same minimal erythema dose (MED).26 However, it is important to note that NB-UVB requires a lower MED for the treatment of psoriasis compared to BB-UVB.24
Another phototherapy source is UVA, which is relatively ineffective in the treatment of dermatological conditions unless when combined with light-sensitizing medication such as psoralens, also known as PUVA.22 PUVA and NB-UVB are equally effective in the treatment of psoriasis, however; NB-UVB phototherapy is more commonly used because it has a lower carcinogenic potential than PUVA.27 Although UVB is responsible for most CPDs, UVA causes indirect DNA damage through the formation of reactive oxygen species (ROS). Increased levels of ROS result in the damage of several structural and functional proteins and DNA, and reduce the efficacy of DNA repair enzymes.28 ROS have also been shown to play a key role in the development of skin cancer including malignant melanoma.22 The detrimental effects of PUVA are long-lasting and patients who have received PUVA therapy are susceptible to developing skin malignancies up to 25 years after receiving their final treatment.13
Some studies have proposed measurements that can be employed to diminish phototherapy- associated DNA damage, and thus minimize the risk phototherapy-induced neoplasia. For instance, a 42-degree Celsius treatment using a 308nm excimer laser prior to UVB phototherapy been shown to reduce the rate of UVB-induced DNA damage and apoptosis of human melanocytes in vitro.29 Another study demonstrated that using low frequency, low intensity electromagnetic fields can divert the deleterious effects of UVB on an animal model of cutaneous T lymphocytes.30 These findings help provide insight for the development of even safer phototherapy protocols.
Discussion
Given the costs and benefits of every treatment option, dermatologists must be able to uniquely tailor treatments on a case-by-case basis to optimize quality of life for patients with chronic dermatologic conditions such as psoriasis, atopic dermatitis, vitiligo and others. With the chronicity and refractory nature of dermatologic conditions that respond well to phototherapy comes a desperation for alternative therapies from prior trials of other first-line treatments. The topical and systemic medications often prescribed prior to phototherapy are often associated with an onslaught of various risks and side effects including but not limited to atrophy, dyspigmentation, acneiform reactions, renal injury, acute liver injury, neutropenia, and immune system dysregulation.31 Avoiding these side effects can serve as one of many incentives for opting into phototherapy instead of topical and systemic agents. The comorbidities associated with autoimmune/autoinflammatory conditions render patients vulnerable to rare, but severe complications associated with immunomodulatory agents and other systemic and topical medications. Additionally, unlike immunomodulatory agents, which are associated with rising costs, phototherapy serves as a much more cost-effective treatment option.
Although phototherapy has become an increasingly attractive option for both providers and patients, there are still considerable disadvantages that must be incorporated into the shared decision-making when crafting a treatment regimen. As described in this review, the increased risk of DNA damage and possible resultant malignancies must be seriously considered before initiating phototherapy. Dermatologists must also consider the time burden of phototherapy, as patients must be able to commit to months of tri-weekly treatments to optimize results. Overall, phototherapy acts a powerful yet nuanced tool that dermatologists must carefully consider depending on each patient’s treatment history, comorbidities, socioeconomic status, and clinical priorities.
To uniquely tailor a phototherapy treatment regimen, several considerations must be incorporated. One factor involves the pigmentation level of the patient, as lighter skin tones are more susceptible to genetic injury.32 The dose-dependent nature of phototherapy-induced DNA damage and malignancy induction is another consideration to keep in mind when prescribing phototherapy. Though increasing the radiation dose increases the efficacy of results and shortens the timeline needed to achieve results, it also prolongs DNA repair paving the way for cancer-associated mutations to exponentially multiply and trigger tumor growth.33,34 One last consideration is the phenomenon of photoadaptation, in which some individuals experience no increase in DNA damage following consecutive doses of phototherapy. The adaptive mechanisms seen in photoadaptation are likely genetically predetermined and include DNA repair, tanning, and thickening of the epidermis.15 Individuals who exhibit photoadaptation develop an increase in MED, reflecting an improved ability to repair DNA damage.35,36 Therefore, it is possible that photoadapters are less susceptible to UVR-induced carcinogenesis following phototherapy.
Our review aims to outline the risks associated with phototherapy and the considerations that must be made for each individual patient who is considering undergoing phototherapy.
Following phototherapy treatment, minimizing the likelihood of developing the cutaneous malignancies through performing routine skin exams in patients who are undergoing, or have undergone, phototherapy remains paramount. Acknowledging the increased risk of phototherapy-induced malignancies plays a crucial role in mitigating the often understated consequences of phototherapy intervention.
References
- Møller KI, Kongshoj B, Philipsen PA, et al. How Finsen’s light cured lupus vulgaris. Photodermatology, Photoimmunology & Photomedicine. 2005;21(3):118–124.
- Situm M, Bulat V, Majcen K, et al. Benefits of controlled ultraviolet radiation in the treatment of dermatological diseases. Coll Antropol. Dec 2014;38(4):1249–1253.
- Tan SY, Buzney E, Mostaghimi A. Trends in phototherapy utilization among Medicare beneficiaries in the United States, 2000 to 2015. J Am Acad Dermatol. Oct 2018;79(4):672–679.
- Vangipuram R, Feldman SR. Ultraviolet phototherapy for cutaneous diseases: a concise review. Oral Dis. May 2016;22(4):253–259.
- Oulee A, Javadi S, Martin A, et al. Phototherapy Trends in Dermatology 2015-2018. Journal of Dermatological Treatment. 2022 Aug;33(5):2545–2546.
- Hung K-F, Sidorova JM, Nghiem P, et al. The 6-4 photoproduct is the trigger of UV-induced replication blockage and ATR activation. Proceedings of the National Academy of Sciences. 2020;117(23):12806–12816.
- Roesner LM, Werfel T. Autoimmunity (or Not) in Atopic Dermatitis. Front Immunol. 2019;10:2128–2128.
- Reeves WH. Autoimmune mechanisms in psoriasis. Semin Dermatol. Sep 1991;10(3):217–224.
- Beyer V, Wolverton SE. Recent Trends in Systemic Psoriasis Treatment Costs. Archives of Dermatology. 2010;146(1):46–54.
- Bascones-Martinez A, Mattila R, Gomez-Font R, et al. Immunomodulatory drugs: oral and systemic adverse effects. Med Oral Patol Oral Cir Bucal. 2014;19(1):e24–e31.
- Liem WH, McCullough JL, Weinstein GD. Effectiveness of topical therapy for psoriasis: results of a national survey. Cutis. May 1995;55(5):306–310.
- Krutmann J, Morita A, Chung JH. Sun exposure: what molecular photodermatology tells us about its good and bad sides. J Invest Dermatol. Mar 2012;132(3 Pt 2):976–984.
- Narayanan DL, Saladi RN, Fox JL. Ultraviolet radiation and skin cancer. Int J Dermatol. Sep 2010;49(9):978–986.
- Maverakis E, Miyamura Y, Bowen MP, et al. Light, including ultraviolet. J Autoimmun. May 2010;34(3):J247–257.
- Bataille V, Bykov VJ, Sasieni P, et al. Photoadaptation to ultraviolet (UV) radiation in vivo: photoproducts in epidermal cells following UVB therapy for psoriasis. Br J Dermatol. Sep 2000;143(3):477–483.
- Thompson KG, Kim N. Distinguishing Myth from Fact: Photocarcinogenesis and Phototherapy. Dermatol Clin. Jan 2020;38(1):25–35.
- Addison R, Weatherhead SC, Pawitri A, et al. Therapeutic wavelengths of ultraviolet B radiation activate apoptotic, circadian rhythm, redox signalling and key canonical pathways in psoriatic epidermis. Redox Biology. 2021 May;41:101924.
- Vieyra-Garcia PA and Wolf P. From Early Immunomodulatory Triggers to Immunosuppressive Outcome: Therapeutic Implications of the Complex Interplay Between the Wavebands of Sunlight and the Skin. Front Med (Lausanne). 2018;5:232.
- Mitchell D, Paniker L, Sanchez G, et al. Molecular response of nasal mucosa to therapeutic exposure to broad-band ultraviolet radiation. J Cell Mol Med. Jan 2010;14(1-2):313–22.
- Kawasumi M, Lemos B, Bradner JE, et al. Protection from UV-induced skin carcinogenesis by genetic inhibition of the ataxia telangiectasia and Rad3-related (ATR) kinase. Proceedings of the National Academy of Sciences. 2011;108(33):13716–13721.
- Lane DP. Cancer. p53, guardian of the genome. Nature. Jul 2 1992;358(6381):15–16.
- Buglewicz DJ, Mussallem JT, Haskins AH, et al. Cytotoxicity and Mutagenicity of Narrowband UVB to Mammalian Cells. Genes (Basel). Jun 11 2020;11(6).
- Lee CH, Wu SB, Hong CH, et al. Molecular Mechanisms of UV-Induced Apoptosis and Its Effects on Skin Residential Cells: The Implication in UV-Based Phototherapy. Int J Mol Sci. Mar 20 2013;14(3):6414–6435.
- Budiyanto A, Ueda M, Ueda T, et al. Formation of cyclobutane pyrimidine dimers and 8-oxo-7,8-dihydro-2′-deoxyguanosine in mouse and organ-cultured human skin by irradiation with broadband or with narrowband UVB. Photochem Photobiol. Oct 2002;76(4):397–400.
- Tzung TY, Rünger TM. Assessment of DNA damage induced by broadband and narrowband UVB in cultured lymphoblasts and keratinocytes using the comet assay. Photochem Photobiol. Jun 1998;67(6):647–650.
- Kunisada M, Kumimoto H, Ishizaki K, et al. Narrow-band UVB induces more carcinogenic skin tumors than broad-band UVB through the formation of cyclobutane pyrimidine dimer. J Invest Dermatol. Dec 2007;127(12):2865–2871.
- Orimo H, Tokura Y, Hino R, et al. Formation of 8-hydroxy-2′-deoxyguanosine in the DNA of cultured human keratinocytes by clinically used doses of narrowband and broadband ultraviolet B and psoralen plus ultraviolet A. Cancer Sci. Feb 2006;97(2):99–105.
- Lawrence KP, Douki T, Sarkany RPE, et al. The UV/Visible Radiation Boundary Region (385–405 nm) Damages Skin Cells and Induces “dark” Cyclobutane Pyrimidine Dimers in Human Skin in vivo. Scientific Reports. 2018/08/24 2018;8(1):12722.
- Hu W, Mi N, Xu Y, et al. 42 °C heat stress pretreatment protects human melanocytes against 308-nm laser-induced DNA damage in vitro. Lasers Med Sci. Oct 2020;35(8):1801-1809.
- Nindl G, Hughes EF, Johnson MT, et al. Effect of ultraviolet B radiation and 100 Hz electromagnetic fields on proliferation and DNA synthesis of Jurkat cells. Bioelectromagnetics. Sep 2002;23(6):455–463.
- Valejo Coelho MM and Apetato M. The dark side of the light: Phototherapy adverse effects. Clin Dermatol. Sep-Oct 2016;34(5):556–562.
- Kelly DA, Young AR, McGregor JM, et al. Sensitivity to sunburn is associated with susceptibility to ultraviolet radiation-induced suppression of cutaneous cell-mediated immunity. J Exp Med. Feb 7 2000;191(3):561–566.
- De Gruijl FR, Van Der Meer JB, Van Der Leun JC. Dose-time dependency of tumor formation by chronic UV exposure. Photochem Photobiol. Jan 1983;37(1):53–62.
- Mbene AB, Houreld NN, Abrahamse H. DNA damage after phototherapy in wounded fibroblast cells irradiated with 16 J/cm(2). J Photochem Photobiol B. Feb 9 2009;94(2):131–137.
- Hamzavi I. Photoadaptation: a path toward rational phototherapy protocols. J Invest Dermatol. Oct 2006;126(10):2156–2158.
- Hexsel CL, Mahmoud BH, Mitchell D, et al. A clinical trial and molecular study of photoadaptation in vitiligo. Br J Dermatol. Mar 2009;160(3):534–539.

