 J Clin Aesthet Dermatol. 2022;15(8):E61–E66.
J Clin Aesthet Dermatol. 2022;15(8):E61–E66.
by Neal Bhatia, MD; Natasha Atanaskova Mesinkovska, MD, PhD; Nancy Samolitis, MD; Seaver Soon, MD; Tyler Steele, BA; and Kaitlyn M. Enright, MSc
Dr. Bhatia is with Therapeutics Clinical Research in San Diego, California. Dr. Mesinkovska is with the University of California Irvine’s Department of Dermatology in Irvine, California. Dr. Samolitis is with Facile Dermatology and Boutique in Los Angeles, California. Dr. Soon is with the Skin Clinic MD in San Diego, California. Mr. Steele is with La Roche-Posay, L’Oréal in New York, New York. Ms. Enright is with Klynical Consulting and Services in Montreal, Quebec.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors received honorarium fees from La Roche-Posay (L’Oréal, USA).
ABSTRACT: Objective. We sought to evaluate the impact of the coronavirus-19 (COVID-19) pandemic on sun-seeking and sun-safe behaviors.
Methods. We conducted an online, cross-sectional, population-based survey.
Results. In total, 1,001 respondents participated in the survey and reported being exposed to 12 or more hours of sunlight (i.e., direct and indirect ultraviolet light, and blue light) each day. Participants self-reported a net increase in all types of light exposure since the onset of the COVID-19 pandemic, especially to blue light (+38%). Notably, while the effects of direct sunlight were well known among survey respondents, they were less aware of the potential damaging impact of indirect sunlight and blue light.
Limitations. As the survey was only conducted among residents of the United States, results might not be generalizable to all geographical regions.
Conclusion. Social outreach strategies are required to improve sun-safe behaviors. Future behavioral interventions should encourage the implementation of broad-spectrum sun protection.
Keywords: Solar radiation, ultraviolet radiation, sun protective factor, sun protection
Due to the COVID-19 pandemic, sun seeking behaviors among the United States population may have shifted, altering the relative risk of photodamage caused by various sources (e.g., direct light, indirect light, and blue light). For example, as many people began working and studying remotely, their exposure to direct sunlight may have decreased, while their exposure to indirect sunlight (e.g., by working and studying near a window; reflected, or scattered by cloud cover and atmosphere; or reflectivity from ground surface) and blue light (e.g., from computers, phones, tablets) most likely increased.1 To better understand the impact of the pandemic on sun-seeking and sun-safe behaviors, a cross-sectional, population-based survey of residents in the United States was conducted.
Methods
In consultation with advisors, a cross-sectional, population-based survey was developed and deployed between July and August 2021. The survey targeted men and women between the ages of 15 and 74 years. The estimated time to complete the survey was 10 minutes. The survey questions are included in the supplemental material. Answers represented consumers’ self-reported behaviors as a yearly average.
The survey questions were designed to establish the population’s general knowledge of the risks of and protective measures against ultraviolet (UV) radiation, and in particular, the damaging effects from various light sources (i.e., direct and indirect UV radiation and blue light). Additionally, the survey evaluated the current state of sun-seeking behaviors since the COVID-19 pandemic as well as the current state of sun-safe behaviors since the COVID-19 pandemic, including sun protective factor (SPF) methods employed and SPF application patterns in different seasons, from different light sources, and on oneself versus one’s children.
Definitions. An important aim of the data collection process was to ensure a diverse sample was attained, with representative participants from regional, ethnic, gender, and generational subgroups accounted for between data collection waves. Generational subgroups were defined as the following:
- “Boomers”: Cohort born between the years 1946 to 1964
- “Generation (Gen) X”: Cohort born between the years 1965 to 1980
- “Millennials”: Cohort born between the years 1981 to 1996
- “Generation (Gen) Z”: Cohort born between the years 1997 to 2012
- Prior to initiating the study, respondents were provided with the following definitions:
- Direct sunlight: An uninterrupted path of light from the sun directly to the skin.
- Indirect sunlight: Sunlight that passes through a medium, whether that is through a window, a shade or shutter, a tree’s leaves, or surface reflection.
- Blue light: Blue light is part of the visible light spectrum (i.e., what the human eye can see). Sunlight is the most significant source of blue light. Electronic devices, including light emitting diode (LED) televisions, computer monitors, smart phones, and tablet screens, are also sources of blue light.
Sample size calculation and statistical analyses. Using a global population size of 7.9 billion, a confidence interval of 95 percent and a margin of error of 5 percent, 395 respondents were required to ensure a sufficient sample size. Data were analyzed using descriptive and inferential statistics.
Results
In total, 1,001 respondents participated in the survey, which reduced the actual margin of error from 5 to 3 percent. The achieved sample size was well above the general recommendation of what is considered a “good” sample size to use during a priori power calculations for predictive models of behavior (e.g., N>200).2 Clinical, scientific, and statistically significant findings are described below.
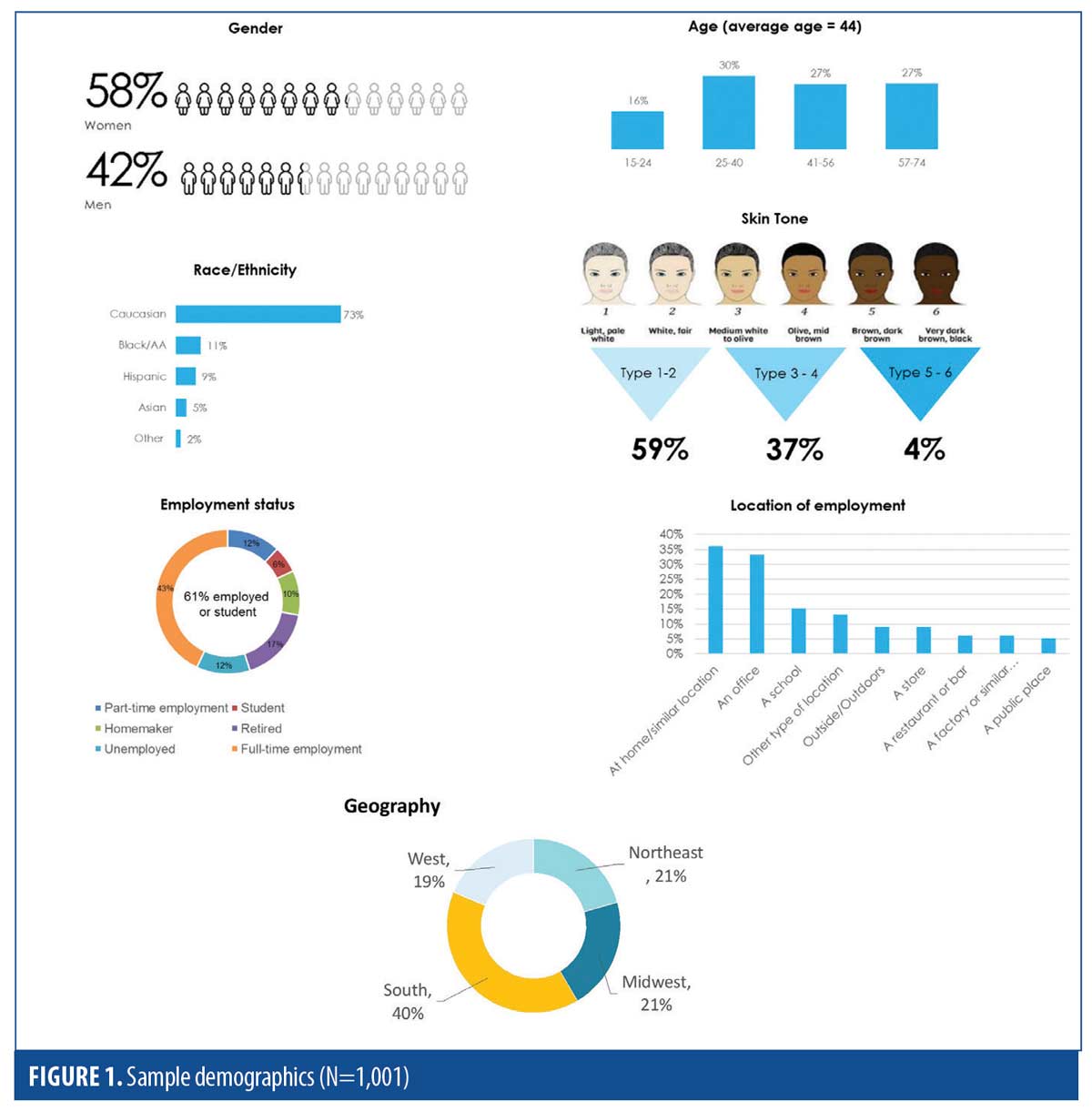
Sample demographics. A roughly equal number of men (48%) and women
(52%) participated in the survey. The majority of respondents were Caucasian (73%), although representatives from all Fitzpatrick Skin Types (I to VI) were included. The average age of the sample was 44 years. Of those working from home (32%), 82 percent were doing so due to the pandemic. Further demographic details of the sample are depicted in Figure 1.
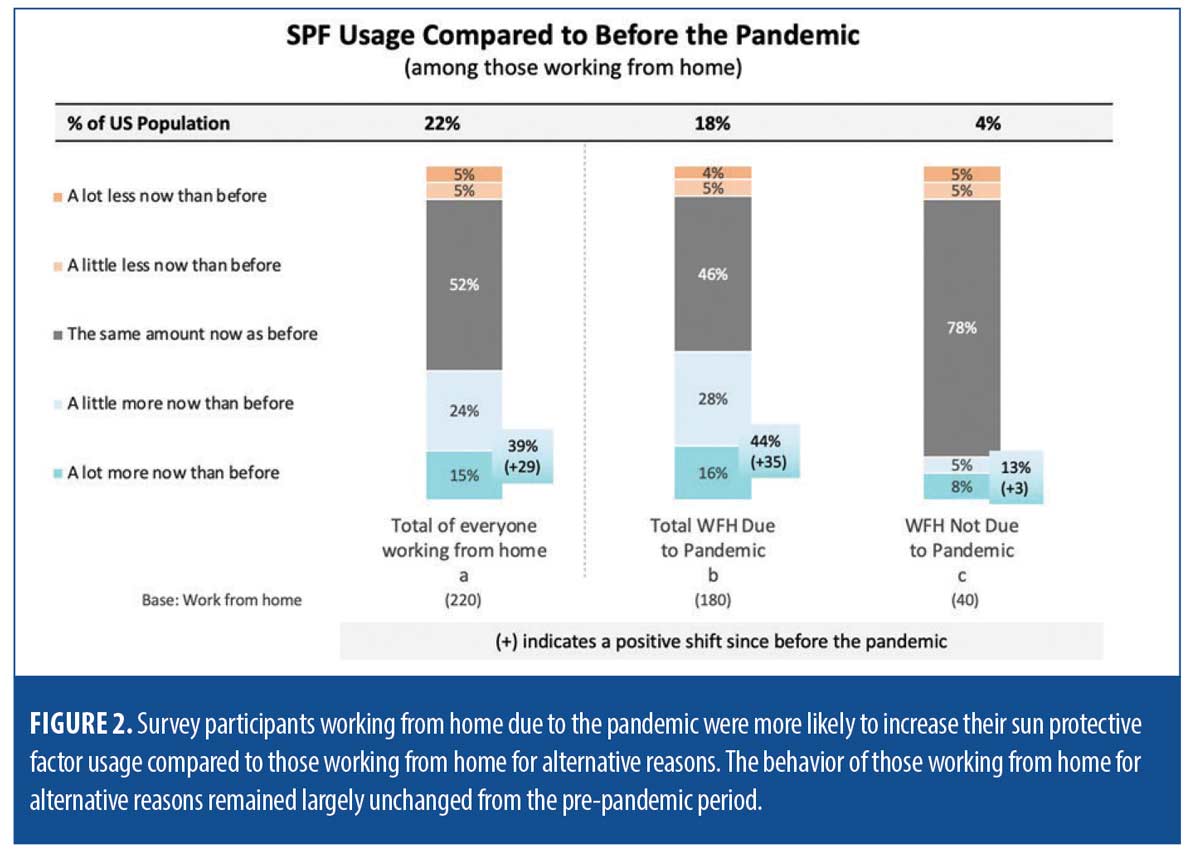
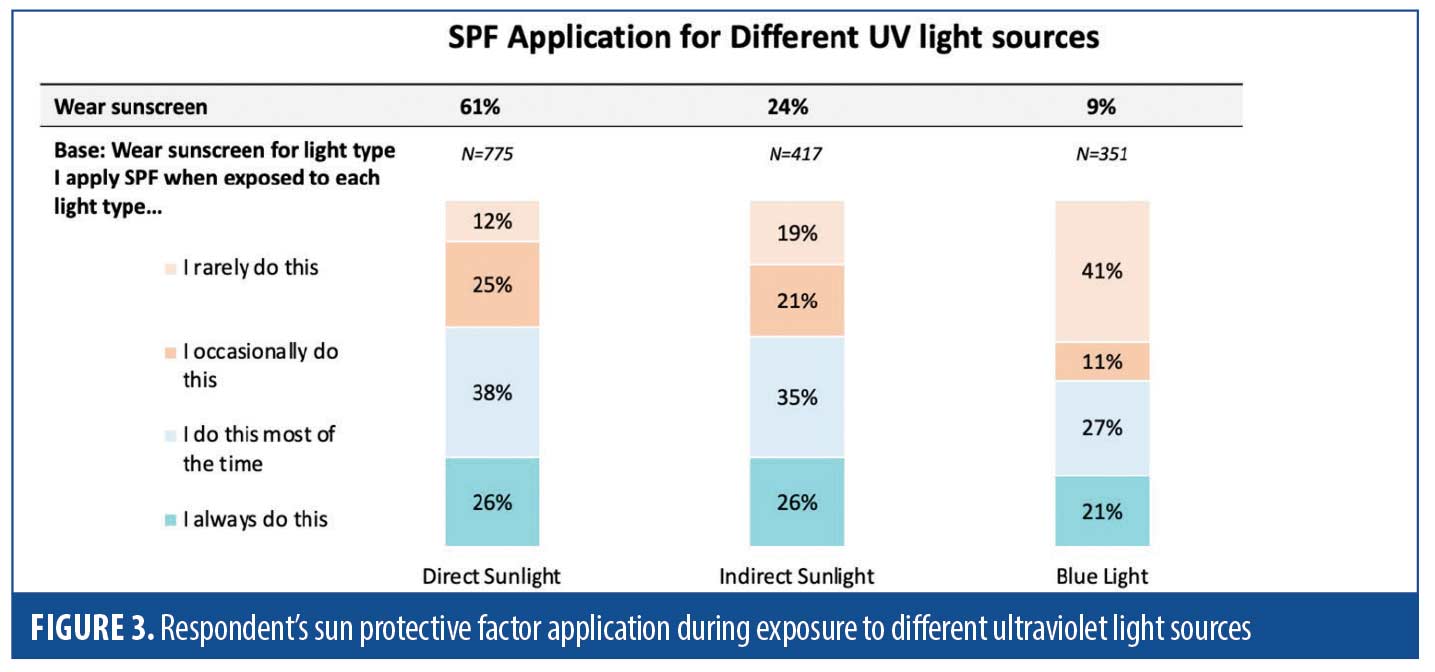
Light exposure. Participants self-reported a net increase in all types of light exposure since the onset of the COVID-19 pandemic, especially to blue light. This included a 12-percent increase in exposure to direct sunlight, a 15-percent increase in exposure to indirect sunlight, and a 38-percent increase in exposure to blue light exposure (Figure 2). Figure 3 displays respondent’s SPF application patterns when exposed to different UV light sources. Participants also reported that following the onset of the pandemic, they were exposed to greater than12 hours of sunlight (i.e., direct, indirect, and blue light) each day, including an average of 3.1 hours of direct sunlight, 4.4 hours of indirect sunlight, and 5.0 hours of blue light.
Direct sunlight. On average, participants self-reported an average of 3.1 hours of direct sunlight per day. Significant subgroup correlations were apparent. For example, African Americans spent significantly more time exposed to direct sunlight than all other ethnicities (e.g., an average of 3.8 hours versus 3.1 hours). In addition, men and participants over the age of 40 years reported being exposed to direct sunlight for a greater amount of time (3.3 and 3.5 hours, respectively). While the majority of respondents were very familiar with direct sunlight, just 4 in 10 were concerned with it.
Indirect sunlight. Participants who worked from home reported sitting either directly next to a window or within a room with a window in 91 percent of cases, versus 74 percent of those who worked in an office outside the home. In both groups, the average amount of time spent next to or near a window (i.e., being exposed to indirect sunlight) was 6.1 hours per day. However, when asked how many hours a day they thought was spent exposed to indirect sunlight, the average response was only 4.4 hours a day. There were no significant differences between subgroups (i.e., age, ethnicity, gender) and the average amount of time spent exposed to indirect sunlight (p>0.05). Regardless of season, respondents were less likely to apply SPF to protect themselves against indirect light than direct light.
Blue light. Participants were exposed to an average of five hours of blue light per day. A significant subgroup skew was observed for “Gen Z”, who spent an average of 5.9 hours a day exposed to blue light. This represented a significantly increased duration compared to all other generational groups (p<0.05). The impact of blue light was a greater concern to respondents than indirect sunlight and created nearly as much concern as direct sunlight.
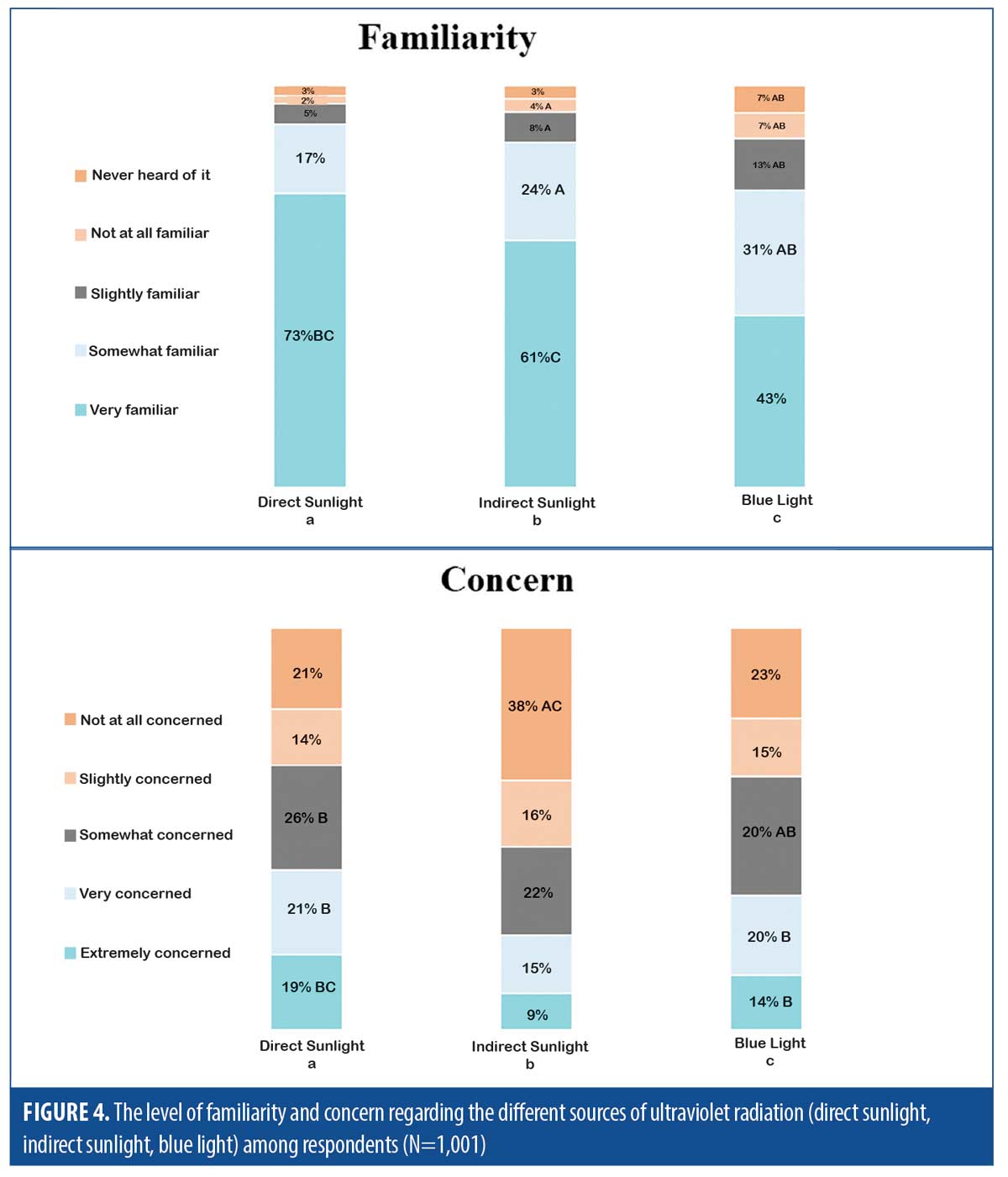
Familiarity and concern. Consumers were familiar with the different light sources, but there were significant subgroup skews observed. For example, 81 percent of “Boomers” reported being “very familiar” with risks associated with direct sunlight, which was significantly higher than other generations (p<0.05); 50 percent of “Gen Z” reported being “very familiar” with the risks associated with indirect sunlight, which was significantly lower than other generations (p<0.05); and 34 percent of “Boomers” reported being “very familiar” with the risks associated with blue light, which was significantly lower than other generations (p<0.05).
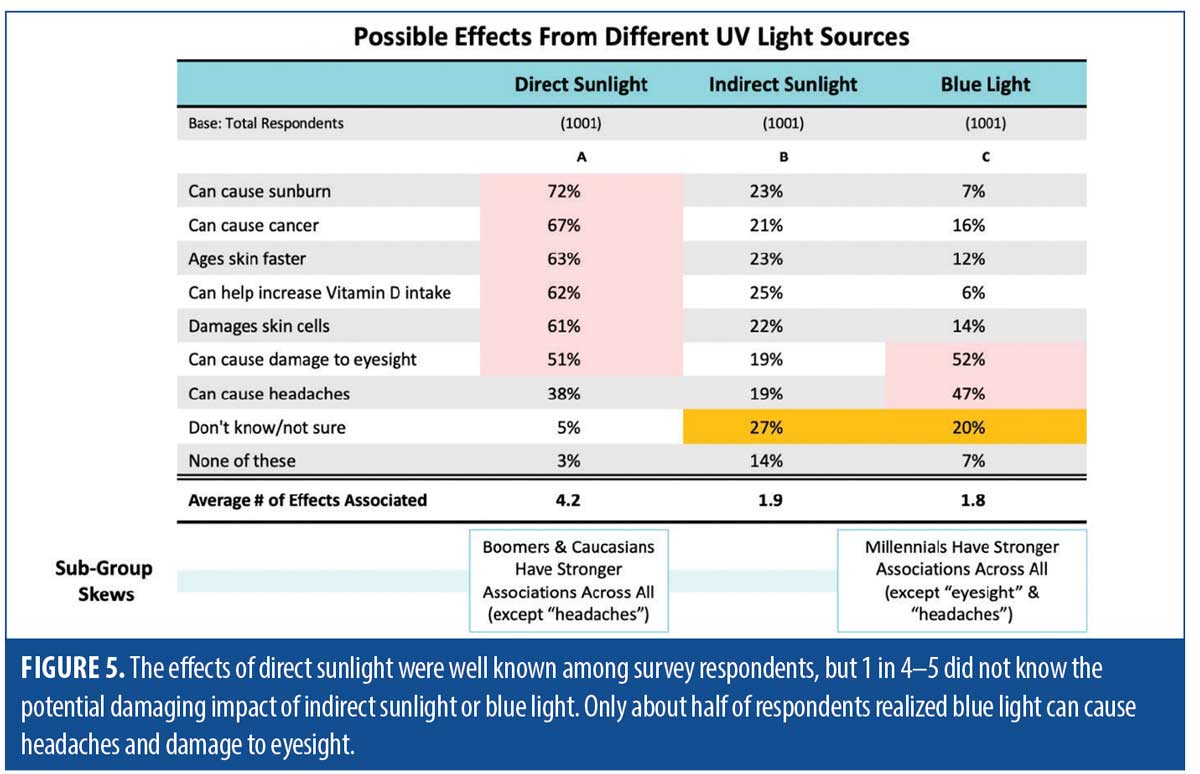
Consumers’ concern was found not to be as strong as their familiarity (Figure 4). For example, 54 percent of the sample reported being “slightly/not at all” concerned with indirect light, 38 percent of the sample reported being “slightly/not at all” concerned with blue light, and 35 percent of the sample reported being “slightly/not at all concerned” with direct light (Table 1). The low level of concern could be because 1 in 5 to 1 in 4 respondents did not know the potential damaging impact of indirect or blue light, and approximately half of the sample realized that blue light could result in headaches and damage to eyesight (Figure 5). “Millennials” were 24 percent, 16 percent, and 24 percent more concerned than other generations regarding direct, indirect, and blue light sources, respectively (significant difference at the 90 percent confidence level).
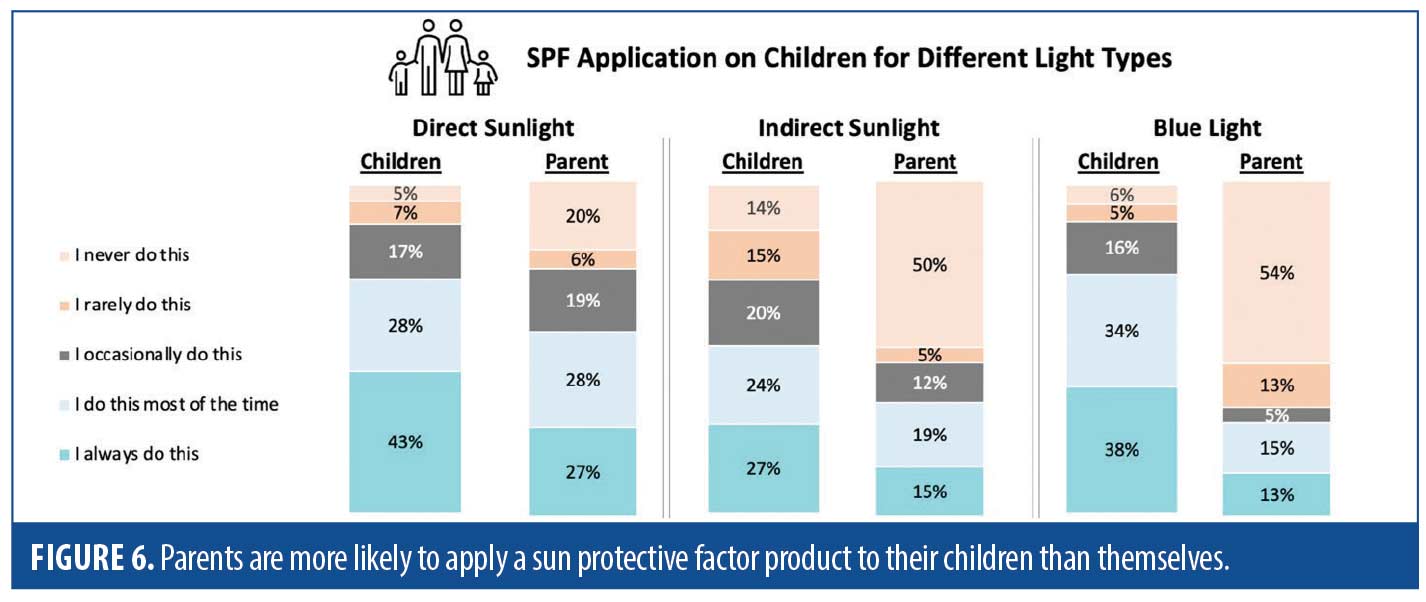
Parent-child correlations. Parents were particularly concerned with keeping their children sun safe (Figure 6). Parents were more likely to apply SPF to their children than themselves, regardless of the light source. Parents had strong beliefs about their young child’s sun-protective behaviors. However, this did not translate into their own sun safe behaviors. Often, parents reported a high awareness of the need to keep their child sun safe and would implement multiple methods to ensure their safety. Despite this finding, parents did not show improved sun safety behaviors compared to other adults in their demographic group (p>0.05). This supports that a lack of concern, rather than knowledge, contributes to the risky sun behaviors among parents.
Potential for behavioral modification. Despite some of the unsatisfactory sun safe behaviors reported by the respondents, there was significant potential for behavioral modifications. For example, 54 percent of participants agreed that they would use SPF if they knew UV light could penetrate through glass and windows; 52 percent of participants agreed that they would use SPF if they knew they could be at risk of harmful UV light exposure when indoors in a room with windows; and 57 percent of participants agreed that if they knew using products that contained SPF could help prevent the negative effects on skin caused by indirect light exposure, that they would use them.
Discussion
A comprehensive understanding of people’s health-behavior decisions is vital to determining which interventions might be most useful. In our study, we conducted a survey aimed at collecting and comparing data related to UV exposure risk, knowledge, concern, and protective behaviors, and explore how these data could potentially inform a social intervention or educational materials to improve sun-safe behaviors. These results can provide guidance to dermatologists and other healthcare practitioners who seek to discuss photoprotection with their patients.3
The top insights provided by the survey results include:
- The lack of consumer awareness regarding the negative effects of indirect light and blue light.
- The apparent apathy of “Gen Z” regarding sun safe behaviors and light sources.
- The limited use and concern with implementing SPF into standard of care, especially during colder months.
- The finding that “children come first” when it comes to applying SPF.
- Parents do not protect themselves as much as their children.
- The lack of consumer knowledge regarding effective SPF and protection against different light sources.
- The finding that consumers are open to education.
To improve sun-safe behaviors among the general population, the authors provide the following guidance to educators and healthcare professionals:
- Working and studying from home is “the new normal” for an unprecedented number of patients, therefore physicians need to counsel and educate their patients on occupational sun safety.
- It may be beneficial for physicians to incorporate questions about where patients work and their proximity to different light sources during procedural consults and routine skin check ups.
- Physicians should remind patients that the majority of sun damage comes from daily, incremental light exposure, and is often incurred during the younger years. The results from our survey suggest that younger generations lack this knowledge. This may increase patients’ understanding of the importance of daily photoprotection, which the current data demonstrate is lacking outside of the older “Boomer” generation.
- Clinicians and members of the general population need to consider the risks associated with all UV light sources, and not simply the more commonly discussed UVA/UVB rays. This is a topic that should be implemented into educational curriculums. Industry and lobbying groups could develop podcasts, web series, and host “lunch and learns” in an effort to better educate clinicians and support staff. Educating support staff may be more effective than educating dermatologists, who often spend less time with patients. Additionally, educational websites could be developed. Consumers could be directed to such websites through the use of QR codes, which could provide a coupon or free sample after watching a short educational video. Dermatologists should become aware of the relevance for protecting against blue light in patients with melasma and those with darker skin types.
Physicians have a responsibility to educate their patients about the risks of UV light and potential sun-safe behaviors. Healthcare practitioners should implement educational methods that promote increasing the personal choice and responsibility of patients in their decision to practice sun-safe behaviors. After a skin treatment, clinics could provide patients with samples of sunscreen, along with a short educational consult. This may promote continued SPF use and give consumers the opportunity to “try before they buy”. Educational campaigns need to address cultural beliefs (e.g., being in the sun and having a tan are a part of Australian identity and culture).4 The industry needs to develop more effective social media campaigns, particularly for targeting “Gen Z”. Based on the findings from a randomized controlled trial,5 educational materials should include UV imagery, as this was found to be most effective at increasing sun safe behaviors.
The way in which consumers employ sun protection methods (when, what [i.e., ability to differentiate between products with appropriate filters], how often, how much)needs to restructure in a way that will promote implementing sunscreen into standard, everyday skincare regimens, not only for anti-aging purposes, but for supporting skin health (e.g., transepidermal water loss, hydration, excessive melanin production, elasticity, fine lines and wrinkles, sun damage, skin cancer), as well.
A concept to be developed is that there are no “cheat days” when it comes to sun protection. Consistent with previous investigations, attitude and concern, group norm and familiarity, and personal choice (e.g., parental responsibility) emerged as significant predictors of people’s intentions which, in turn, significantly predicted sun-safe behaviors. However, compared to previous research, the level of direct sunlight has decreased since the pandemic and the level of indirect light and blue light exposure has increased.5-11 As many industries and institutions have indicated their willingness to maintain the home office and virtual learning modality, these patterns likely reflect the “new normal”.12,13 Unfortunately, the general consumer’s knowledge of indirect and blue light is limited, and often, they do not consider using products containing SPF when in the presence of blue light.14
According to our survey results, parents generally had knowledge of the broad sun safety recommendations; however, the specific details of the recommendations were not always known. Parents reported adopting a range of sun-protective measures for their child, which depended on the time of year. A range of advantages (e.g., reducing the risk of skin cancer, developing good habits early and parental peace of mind), disadvantages (e.g., false sense of safety and preventing vitamin D absorption), barriers (e.g., child refusal) and facilitators (e.g., routine and accessibility) to performing sun safe practices were identified. Normative pressures and expectations also affected parents’ motivation to be sun safe for their child. These findings have important implications for policy development and suggest that, although parents may be informed about sun safe behaviors for their child, this knowledge is not necessarily a prerequisite for effective action. Given that parents adopt different behaviors across the year, which is contrary to recommendations, educational campaigns that often focus on imparting accurate information may not produce desirable behavior. Despite a fairly thorough knowledge regarding the relationship between skin cancer and sun exposure, parents’ behavior was unsatisfactory. This also supports that knowledge is not sufficient to produce a positive behavior, as determinants of these two aspects are different.
The finding that participants were exposed to greater than12 hours of UV radiation and or blue light per day is significant. In effect, participants are continuously exposed to one or more light sources during regular waking hours. Healthcare professionals should be considered as key figures for future multicomponent intervention strategies in the field of photoprotection. Future interventions targeting cultural beliefs will be more effective, as the health messages can be tailored to the specific group and behavior. These identified beliefs can be used to inform interventions to improve sun safe behaviors.9 Computer-based educational resources may also be effective at increasing knowledge and changing behaviors.15,16
Educational materials should also target specific subgroups of the population. For example, African Americans were exposed to the highest levels of direct sunlight, yet this cohort had the most infrequent use of SPF. Moreover, despite participants with higher skin phototypes (Fitzpatrick skin types IV to VI) have an increased susceptibility to the damaging effects of blue light, the general population’s knowledge of this fact was extremely limited.17,18 Another area of improvement concerns the inconsistent use of SPF throughout the seasons. Given the known damaging effects of indirect light and blue light, educators should promote the continued use of SPF, even in colder months.
Limitations. Health decision making is a complicated process involving influences from many sources, and motivational factors often vary between individuals. Therefore, theory-based research, such as the current evaluation, may fail to predict future actions with complete accuracy. The interpretation of the current survey results should be considered within the limitations of cross-sectional studies, which are observational and descriptive in nature and may not be causal or relational. Lastly, although this survey collected data on consumers’ average behavior throughout the year, irradiances vary widely in a country like Canada.
Conclusion
The effects of direct sunlight were well known, but survey respondents were less aware of the potential damaging impact of indirect sunlight or blue light. Moreover, sun-seeking and sun-safe behaviors, level of concern regarding UV exposure, and knowledge of risk vary significantly among major subgroups of the general population (e.g., generations, ethnicities). Evidence supports that social media campaigns may provide an effective outreach strategy for improving sun-safe behaviors, particularly among the “Gen Z” cohort. Future behavioral interventions should encourage the implementation of broad-spectrum sun protection, including protection against solar radiation that can damage the cutaneous layers and negatively affect skin heath (i.e., direct light, indirect light, and blue light). Lastly, committed support from healthcare practitioners, cancer foundations and employers may encourage the widespread implementation of sun-safety education programs.
References
- Bourdas DI, Zacharakis ED. Evolution of changes in physical activity over lockdown time: Physical activity datasets of four independent adult sample groups corresponding to each of the last four of the six COVID-19 lockdown weeks in Greece. Data Brief. 2020 Oct;32:106301. Epub 2020 Sep 11.
- Weston R, Gore PA Jr. A Brief Guide to Structural Equation Modeling. The Counseling Psychologist. 2006; 34(5), 719–751.
- Hedges T, Scriven A. Sun safety: what are the health messages? J R Soc Prom. Health. 2008; 128(4):164–169.
- White KM, Starfelt LC, Young RMD, et al. Predicting Australian adults’ sun-safe behaviour: examining the role of personal and social norms. B J Health Psychol. 2015; 20(2):396–412.
- Pokharel M, Christy KR, Jensen JD, et al. Do ultraviolet photos increase sun safe behavior expectations via fear? A randomized controlled trial in a sample of U.S. adults. J Behav Med. 2019; 42(3):401–422.
- Aleo G, Bagnasco A, Cozzani E, et al. Sun-safe behaviours, personal risk, level of concern, and knowledge about cutaneous melanoma in Italy: time for social marketing? J Prevent Med Hygiene. 2020; 61(2):258.
- Dudley DA, Cotton WG, Winslade MJ, et al. An objective and cross-sectional examination of sun-safe behaviours in New South Wales primary schools. Bmc Public Health. 2017; 17(1), 21–22.
- Hewitt M, Denman S, Hayes L, et al. Evaluation of ‘sun-safe’: a health education resource for primary schools. Health Edu Res. 2001;16(5):623–633
- Reinau D, Weiss M, Meier CR, et al. Outdoor workers’ sun-related knowledge, attitudes and protective behaviours: a systematic review of cross-sectional and interventional studies. Br J Dermatol. 2013 May; 168(5):928–940.
- Suppa M, Cazzaniga S, Fargnoli MC, et al. Knowledge, perceptions and behaviours about skin cancer and sun protection among secondary school students from central Italy. J Eur Acad Dermatol Ven. 2013;27(5):571–579.
- Kyle RG, MacMillan I, Forbat L, et al. Scottish adolescents’ sun-related behaviours, tanning attitudes and associations with skin cancer awareness: a cross-sectional study. BMJ Open. 2014; 4(5).
- Alves TLde L, Amorim AFA, Bezerra MCC. Not one less! Adaptation to the home office in times of covid-19. Revista de administração contemporânea. 2021;25(Spe).
- Pregowska A, Masztalerz K, Garlinska M, et al. A worldwide journey through distance education–from the post office to virtual, augmented and mixed realities, and education during the covid-19 pandemic. Education Sciences. 2021; 11.
- Shen Q, Xu L, Jiang Y, et al. 2020 3rd International Symposium on Big Data and Applied Statistics, ISBDAS 2020 3 2020 07 10 – 2020 07 12. Survey and statistical analysis of Hangzhou citizens’ awareness of harmful blue light and consciousness of protection against blue light. J Phys. 2020; 1616(1).
- Kanellis VG, Kanellis AL. Parental and primary caregiver’s attitudes towards sun safe hat and sunscreen use at a major national children’s playground in Canberra, Australia. J Dermatol. 2020; 61(3):332.
- Hamilton K, Cleary C, White, KM et al. Keeping kids sun safe: exploring parents’ beliefs about their young child’s sun-protective behaviours. Psycho-Oncology, 25(2), 158–163.
- Bryant J, Zucca A, Brozek I, et al. Sun protection attitudes and behaviours among first generation Australians with darker skin types: results from focus groups. J Immigr Minor Health. 2015; 17(1):248–254.
- Wright CY, Albers PN, Oosthuizen MA, et al. Self-reported sun-related knowledge, attitudes and behaviours among schoolchildren attending south African primary schools. Photodermatol Photoimmunol Photomed. 2014; 30(5):266–276.

