J Clin Aesthetic Dermatol. 2023;16(5):S3
by Ashish Bhatia, MD, FAAD; Cheryl M. Burgess, MD, FAAD;
Gilly Munavalli, MD; and Jason L. Smith, MD
Dr. Bhatia is with Oak Dermatology in Naperville, Illinois; Dr. Burgess is with the Center for Dermatology and Dermatologic Surgery in Washington, DC; Dr. Munavalli is Medical Director and Founder of Dermatology, Laser, & Vein Specialists of the Carolinas in Charlotte, North Carolina; and Dr. Smith is with NWGA Dermatology in Rome, Georgia.
FUNDING: Strata Skin Sciences provided funding for the development of this supplement.
DISCLOSURES: Participants in this roundtable have received consulting fees, honoraria, research grants, and/or other remuneration from the following companies: Dr. Bhatia— Abbvie, Alastin Skincare, Allergan/an Abbvie Company, Avita Medical, Bausch Health, Biomarck, Carpe, Cutera, Cytrellis, DermEd Foundation, Eclipse, Emblation Ltd., Endo Pharmaceuticals, Envy Medical, Evolus, Entrepix Medical, Evolus, Genzum, Medline, Merz Aesthetics, MiMEDx, Novasan, Obagi, Ortho Dermatologics, Paradigm Medical, Pulse Biosciences, R2 Technologies, Revance, Sonoma, Solta Medical, Suneva Medical, Strata Skin Sciences, Theravant Corporation, Vyne Therapeutics Zalea, and ZO Skin; Dr. Burgess—AbbVie, Incyte, Allergan, Merz Aesthetics, Revance, and Strata Skin Sciences; Dr. Munavalli—Abbvie, Candela, Pulse Biosciences, and Strata Skin Sciences; Dr. Smith—Strata Skin Sciences.
Foreword
Acne vulgaris affects up to 50 million Americans each year impacting people of all ages.1 It is the number one and number three reasons for seeking care from a dermatologist among those under 18 years and adults, respectively.2 Despite recent advances in topical and oral medication for acne, it remains challenging to treat and requires long-term therapy.
In 2016, acne treatment guidelines developed by a group of dermatologists aimed to align consensus on therapeutic interventions.3 Regardless of degree of severity, multiple simultaneous drug treatments are recommended to target the multifaceted nature of acne.4 Antibiotic stewardship is paramount. However, both oral and topical medications take time to work and are associated with some unpleasant side effects.3,5 Furthermore, some drug treatments may be unsuitable for certain populations, such as pregnant patients, young children, and individuals with skin of color.3,5
Rarely has the focus of acne treatment been on the use of noninvasive devices, either as mono- or adjuvant therapy. However, devices can provide a drug-free, noninvasive treatment option for patients desiring this type of intervention.
Genetic and environmental factors impact several key root causes of acne. Hyperkeratinization, excess sebum production, and colonization with Cutibacterium acnes (C. acnes) foster localized inflammation and formation; lesions may persist or worsen due to clogged pores and bacterial overgrowth.4
Within this supplement to the Journal of Clinical and Aesthetic Dermatology, we explore the merits of TheraClear®X Acne System (Strata Skin Sciences, Horsham, Pennsylvania), a combination broadband light and vacuum suction device that mechanically clears obstructed pores and visibly reduces acne lesions in a short period of time. The first article provides an overview of the device, including its likely mechanism of action. Treatment protocols and clinical results are discussed. The second article provides key highlights of an expert roundtable discussion regarding practical uses of the TheraclearX system, giving professional tips on its use and a description of outcome expectations for both user and patient.
We hope this issue provides the reader with a thorough understanding of the TheraClearX system and how it fits into the acne treatment landscape.
References
- American Academy of Dermatology. Skin conditions by the numbers. https://www.aad.org/media/stats-numbers. Accessed April 30, 2023.
- Perche PO, Peck GM, Robinson L, et al. Prescribing trends for acne vulgaris visits in the United States. Antibiotics (Basel). 2023;12(2):269.
- Zaenglein AL, Pathy AL, Schlosser BJ, et al. Guidelines of care for the management of acne vulgaris. J Am Acad Dermatol. 2016;74(5):945–973.e33.
- Lai JJ, Chang P, Lai KP, et al. The role of androgen and androgen receptor in skin-related disorders. Arch Dermatol Res. 2012;304(7):499–510.
- Elsaie ML. Hormonal treatment of acne vulgaris: an update. Clin Cosmet Investig Dermatol. 2016;9:241–248.
Photopneumatic Technology for the Treatment of Mild-to-moderate Acne Vulgaris —A Review
J Clin Aesthetic Dermatol. 2023;16(5):S4–6
by Gilly Munavalli, MD
Dr. Munavalli is Medical Director and Founder of Dermatology, Laser, & Vein Specialists of the Carolinas in Charlotte, North Carolina.
ABSTRACT: Acne vulgaris, despite being one of the most common dermatological diseases, remains challenging to treat. Acne lesion location and type, skin tone, genetics, and environmental factors influence mono- or multimodal therapeutic decisions. Combination topical and oral treatments may successfully reduce lesion count; however, these agents take time to work, and side effects are not uncommon. The long-term therapeutic engagement required to treat acne may be too costly or burdensome for many patients, which may impact treatment adherence, which can negatively impact patient outcomes. There is increased interest in noninvasive acne treatments to reduce side effects, provide rapid results, and foster treatment adherence. TheraClearX® X Acne System combines broadband pulsed light and vacuum suction technology. The combination of these two treatment modalities mechanically clears congested follicles and targets endogenous porphyrins produced by Cutibacterium acnes and other acnegenic bacteria. This article describes the proposed mechanism of action, treatment advantages, examples of treatment protocols, and anecdotal results using this combination device in the treatment of acne. Keywords. Acne, vacuum, broadband light, noninvasive
Brief Overview of Acne Treatment Devices
Pulsed light treatments (IPLs). IPLs have been used both alone and in combination with other modalities to rapidly reduce active acne.1–4 Postulating that a broadband light source would activate endogenous porphyrins, researchers have assessed the use of pulsed light and heat devices in the treatment of acne, reporting noticeable improvements in acne lesions.5,6 Chang et al7 evaluated a pulsed light device with a cut-off filter between 530 and 750nm in the treatment of inflammatory acne and post-acne-related erythematous lesions. Patients were randomized to a split-face treatment, using benzoyl peroxide as the control. Results showed a decrease in lesion count on both sides of the face, with no statistical difference; however, the pulsed light-treated side was noted to have marked improvement in acne- related sequelae, such as post-inflammatory erythema and hyperpigmentation.8
Vacuum. The use of vacuum suction for the treatment of acne was first described in dermatology literature by Moschowitz,9 who described eight patients with acne who were treated with a rubber bulb to apply slight suction to acne lesions so as to cause localized hyperemia.
Combination pulsed light and vacuum. A combination of pulsed light and vacuum has been evaluated in the treatment of acne. In a multicenter retrospective study, Shamban et al10 assessed the effectiveness of a combination of pulsed light and vacuum device, reporting physician-evaluated mean clearance rates of 50 percent (following a single treatment) to 90 percent (following four treatments) in patients with mild-to-severe acne.
Based on performing over 150 acne treatments using a combination pulsed light and vacuum device, the current author has observed that marked improvement in acne lesions can be achieved in as few as two treatments spaced 1 to 2 weeks apart.
Corroborating this, Gold et al11 administered four treatments using a pulsed light and vacuum device to patients with acne at three-week intervals. At 91 days (1 month after the final treatment), the median inflammatory lesion count (n=10 subjects with complete data) decreased from 22.0 (inter-quartile range) to 10.5 (P=0.0196). For noninflammatory lesions, the median counts decreased from 25.0 to 10.0 (P=0.0956). The corresponding reduction percentages ([baseline count-post treatment count/baseline count] X100) were 78.8 percent for inflammatory lesion counts and 57.8 percent for noninflammatory lesion counts. At 153 days (n=6 with complete data), reductions were significant for both inflammatory (P=0.0137) and noninflammatory (P=0.0383) counts.
In a study involving 20 patients with mild-to-severe facial acne who were treated with a combination of pulsed light and vacuum, Wankiphakdeedecha et al12 reported that the greatest improvements in acne clearance were achieved in patients with severe acne.
TheraClear® X acne system overview
The TheraClear®X Acne System (Strata Skin Sciences, Horsham, Pennsylvania) delivers a combination of broadband pulsed light (500–1200nm) concurrent with the application of vacuum.8,13 The TheraClearX system is technologically based on principals of physics and biology, and functions by mechanically clearing congested follicles of the affected pilosebaceous apparatus using a suction-activated tip while simultaneously administrating broadband light with a cut-off filter from 500 to 1200nm to activate endogenous porphyrins in pathogenic bacteria. The device is capable of generating vacuum with pressure up to three pounds per square inch (psi) in a confined treatment area, which effectively lifts the dermal structures toward the epidermis and expels follicular contents onto the skin’s surface.8,9,14
Mechanism of Action
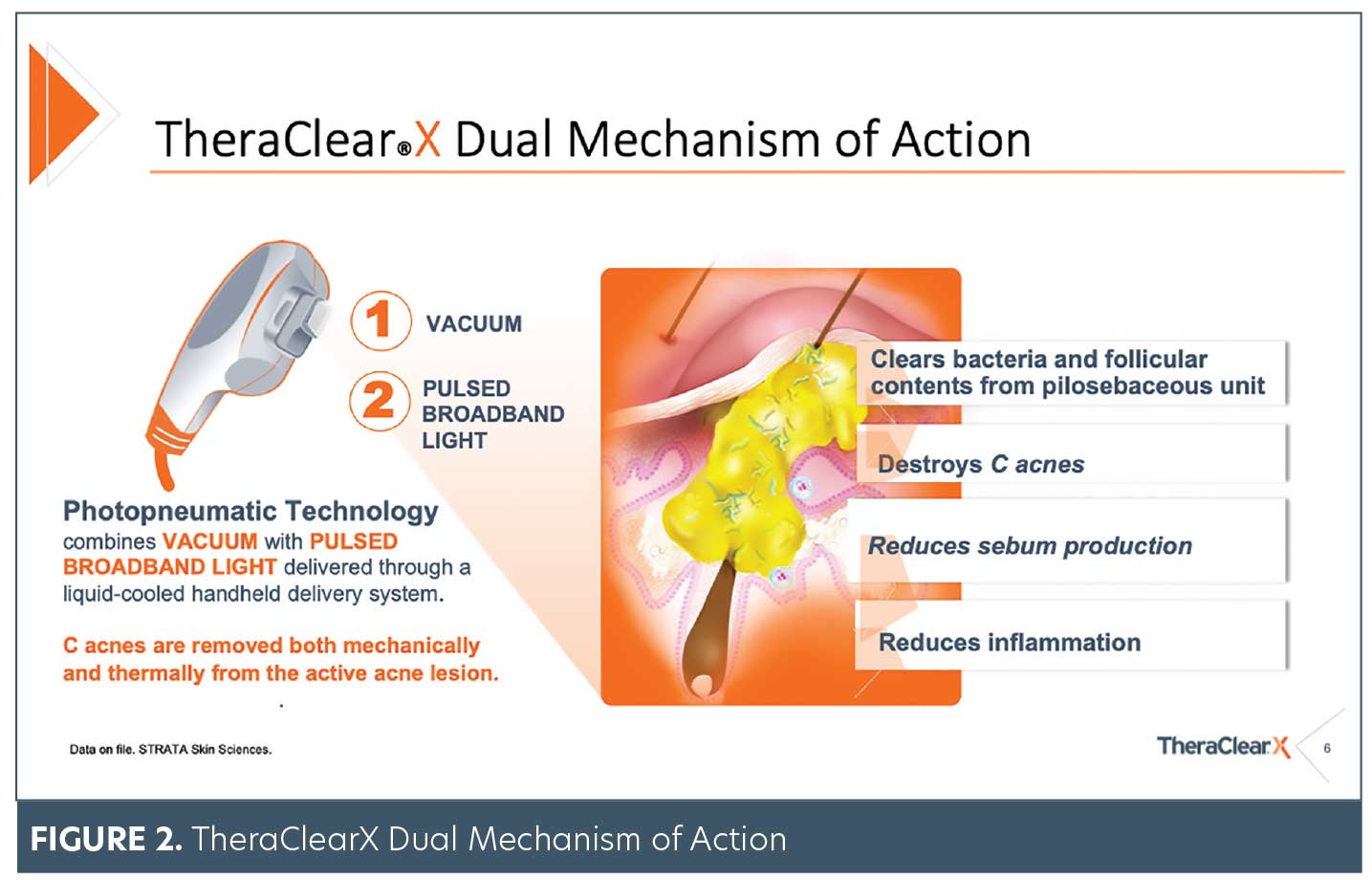
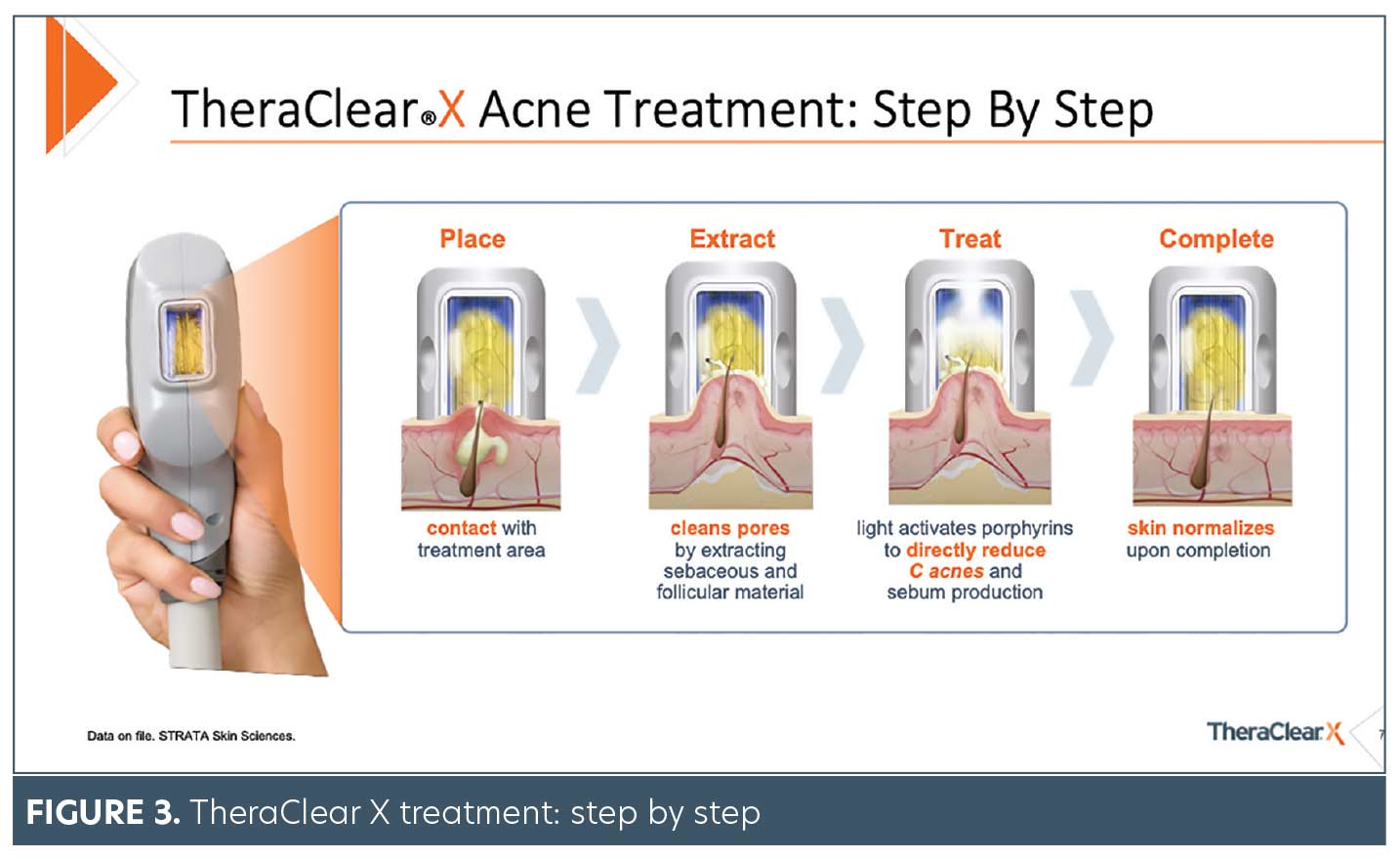
The TheraClearX device works by placing the treatment chamber over the area to be treated. When complete contact with the treatment surface is detected, a vacuum is applied, drawing affected skin into the treatment chamber. The effect of vacuum elevates the sebaceous gland toward the surface, momentarily stretching the skin 25 to 35 percent, extracting the obstructed sebaceous material. An array of flash lamps subsequently irradiate the treatment area. Along with targeted heating of the dermis, the endogenous effect of light activates porphyrins to destroy Cutibacterium acnes (C. acnes) and reduce sebum production. When the process is completed, the vacuum is released and the skin is normalized.
Therapeutic effect of vacuum. The immediate and rapid pressure change on the follicular ostia of the pilosebaceous unit dislodges keratin plugs and allows evacuation of sebum onto the surface of the skin. When sebum is extracted from the clogged pilosebaceous duct, various commensal and pathogenic bacteria residing in the pilosebaceous unit are simultaneously extruded or thermally injured.15 In studies conducted with similar devices, researchers demonstrated that both antibiotic-resistant and antibiotic-susceptible bacteria can be mechanically extruded.7 These reports indicated that much of the bacteria was antibiotic-resistant and presumably unresponsive to topical or oral antibiotics. Mechanical extrusion of bacteria significantly reduced bacterial load on the sebaceous gland, effectively diminished the localized inflammation, and clinically resolved the acne lesions.7,12
Endogenous effect of light. The TheraClearX system uses a series of xenon flash lamps that provide a broadband output ranging from 500 to 1200nm. An optical coating removes the shorter wavelengths that can potentially damage the heavily melanated epidermis of patients with darker skin types, making the spectrum safe for the treatment of all Fitzpatrick skin types (I–VI).
The sebaceous material that clogs the pilosebaceous duct causing inflammatory acne is composed of a variety of substances, including sebum and tissue (e.g., keratin, melanin) that once formed the epidermis. Consequently, this sebaceous material’s absorption spectrum is more complex than the absorption spectrum of porphyrins associated with C. acnes bacteria. In the study by Chang et al,7 investigators collected the extracted sebaceous material to determine its absorption spectrum, reporting that sebum closely resembles that of melanin. This observation is not surprising when one considers that melanin is one of the major constituents of this extruded sebaceous material.
Comparing the spectral output of the TheraClearX system to the absorption spectrum of the material extracted from the sebaceous gland, light output between 800 and 1000nm plays an important role in heating this material. Consistent with clinical literature, the broadband light source of the TheraClearX system activates endogenous porphyrins and also has an effect on perilesional erythema/inflammation due to absorption in the 500 to 600 nm range.10–15
Key Features
Continuously cooled handpiece. Continuous cooling keeps the walls of the treatment chamber cool for added safety for both patient and provider. In other products, the metallic walls must be manually cooled every 5 to 10 pulses of light with an exogenous cryogen spray. However, TheraClearX device’s continuously cooled treatment inserts allow the operator to perform the treatments quickly and with less risk of error, which could potentially occur with frequent pauses to manually cool skin.
Water temperature sensors. In the TheraClearX device, sensors monitor water temperatures keeping temperature in a safe range. In older vacuum and light technologies, the only indication that the walls exceeded safe temperatures was the clinical appearance of the treated skin and the pain response of the patient.
Water cooled lamps. The TheraClearX device uses water-cooled lamps to increase lamp life and reduce the cost of consumables.
Customizable vacuum settings. TheraClearX’s customizable vacuum settings allow for microadjustments to the vacuum, making the treatment more comfortable for the patient and allowing better access on previously challenging areas. Three new soft vacuum modes greatly reduce potential for purpura on sensitive areas such as the forehead, temples, and nose.
Single light filter optimizes spectral output for all Fitzpatrick skin types. A highly optimized spectral output allows for a single light filter to effectively treat all skin types, including Fitzpatrick Skin Types IV to V patients.
Soft silicon treatment inserts. All treatment inserts have soft silicon flanges that enable easier contact with the treatment area and enhance patient comfort, especially when treating aggravated areas.
Clinical Outcomes
The TheraClearX system is US Food and Drug Administration (FDA)-cleared for the treatment of mild-to-moderate inflammatory, comedonal, and pustular acne on all skin types.
Treatment protocols. Treatment Protocol: Prior to treatment, gentle cleansing with a warm washcloth helps soften skin and helps facilitate extraction of comedones. Energy settings are selected based on skin types. Vacuum settings are selected based on treatment areas, with vacuum settings being reduced when treating delicate areas, such as the forehead.
For all our patients, we use a double pulse with two passes over the entire face. Patients are typically treated at weekly intervals for 4 to 5 treatments, based on the severity of acne.
Evaluation and outcomes. Patients in our clinic who were treated with TheraClearX were evaluated using standardized photographs. Each patient was photographed before first treatment and then before each one of five subsequent treatments. Patients were evaluated for a reduction in lesions, a reduction in erythema (redness) caused by acne, changes in skin texture and improvements in skin texture. Patients were also evaluated for treatment related side effects.
All patients demonstrated at least a 50-percent improvement in lesion counts post-first treatment. Subjective evaluations included a visible reduction in redness around acne lesions as well as visible reduction in crusting. The majority of patients reported a reduction in redness 24 to 72 hours post-first treatment.
Patients uniformly described the treatment as being very comfortable. Consequently, adherence rates were high for all study patients. Patients also reported less oily skin. This was also visible upon skin evaluation. Patients with hyperpigmentation caused by acne noted visibly more even skin tone after first treatment. Patients with large pores reported a reduction in pore size and a consequent improvement in skin texture.
No significant side effects were reported. The most commonly reported treatment-related side effect was minor purpura that resolved 24 to 72 hours post-treatment. This was not observed when using the soft vacuum modes on the device. Immediate post-treatment skin reactions were limited to localized mild and transient erythema, which resolved within 30 minutes of treatment. Patients reported satisfaction with outcomes.
Conclusion
Our experience to date demonstrates that TheraClearX treatments are well tolerated by patients and effective for the treatment of a wide range of mild-to-severe acne. There was little to no discomfort during treatments and no downtime. No anesthetics or numbing gels were used prior to treatment. Most noticeably, patients noted an immediate reduction in redness post first treatment as is indicated by the photographs.
While these initial findings warrant larger scale randomized studies, we do believe that the TheraClearX System is effective for the treatment of a wide range and severity of acne.
References
- Bhardwaj SS, Rohrer TE, Arndt K. Lasers and light therapy for acne vulgaris. Semin Cutan Med Surg. 2005;24(2):
107–12. - Yeung CK, Shek SY, Bjerring P, et al. A comparative study of intense pulsed light alone and its combination with photodynamic therapy for the treatment of facial acne in Asian skin. Lasers Surg Med. 2007;39(1):1–6.
- Prieto VG, Zhang PS, Sadick NS. Evaluation of pulsed light and radiofrequency combined for the treatment of acne vulgaris with histologic analysis of facial skin biopsies. J Cosmet Laser Ther. 2005;7(2):63–68.
- Taub AF. A comparison of intense pulsed light, combination radiofrequency and intense pulsed light, and blue light in photodynamic therapy for acne vulgaris. J Drugs Dermatol. 2007;6(10):1010–1016.
- Elman M, Lask G. The role of pulsed light and heat energy (LHE) in acne clearance. J Cosmet Laser Ther. 2004;6(2):
91–95. - Gregory AN, Thornfeldt CR, Leibowitz KR, Lane M. A study on the use of a novel light and heat energy system to treat acne vulgaris. Cosmet Dermatol. 2004;17(5):287–292.
- Chang SE, Ahn SJ, Rhee DY, Choi JH, Moon KC, Suh HS, et al. Treatment of facial acne papules and pustules in Korean patients using intense pulsed light device equipped with 530- to 750-nm filter. Dermatol Surg. 2007;33(6):676–679
- Munavalli GS, Weiss RA. Evidence for laser- and light-based treatment of acne vulgaris. Semin Cutan Med Surg. 2008;27(3):207–211.
- Moschowitz E. Acne. A new method of treatment of. J Cutan Dis. 1906;24(10):491.
- Shamban AT, Enokibori M, Narurkar V, Wilson D. Photopneumatic technology for the treatment of acne vulgaris. J Drugs Dermatol. 2008;7(2):139–145.
- Gold M, Biron J. Treatment of acne with pneumatic energy and broadband light. J Drugs Dermatol. 2008; 7(7):
639–642. - Wanitphakdeedcha R, Tanzi E, Alster T. Photopneumatic therapy for the treatment of acne. J Drugs Dermatol. 2009;8(3):239–241.
- Munavalli GS and Weiss RA. Combination light therapies for the treatment of acne: an overview and introduction to photopneumatic therapy. Med Las Appl. 2008;23;3:
141–146. - Data on File. STRATA Skin Sciences. 2023.
- Omi T, Munavalli GS, Kawana S, Sato S. Ultrastructural evidence for thermal injury to pilosebaceous units during the treatment of acne. J Cosmet Laser Ther. 2008;10(1):
7–11.
Photopneumatic Technology for the Treatment of Mild-to-moderate Acne Vulgaris Expert Perspectives
J Clin Aesthetic Dermatol. 2023;16(5):S7–S11
An expert roundtable featuring Ashish Bhatia, MD, FAAD; Cheryl M. Burgess, MD, FAAD; Gilly S. Munavalli, MD, MHS, FACMS; and Jason L. Smith, MD
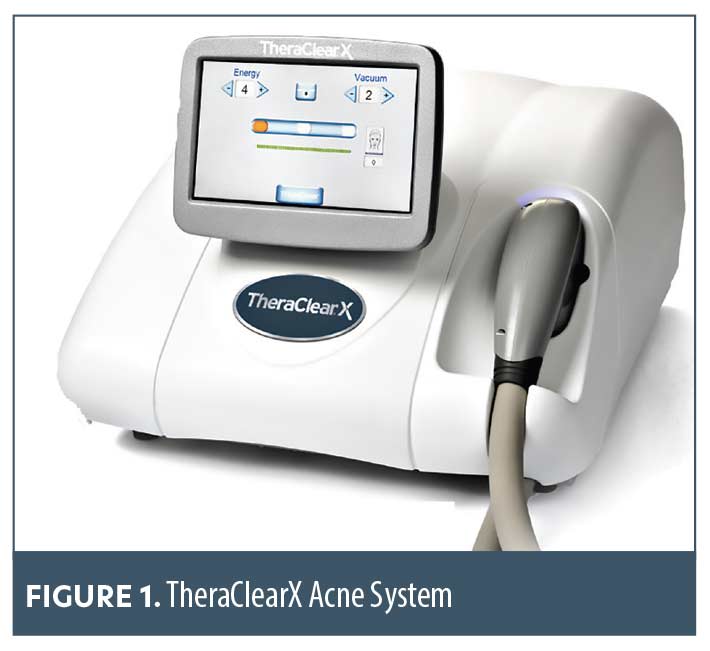
TheraClear®X Acne System (Strata Skin Sciences, Inc) is a photopneumatic device specifically engineered and indicated for the treatment of mild-to-moderate acne, including comedonal, pustular, and inflammatory acne vulgaris (Figure 1). This article highlights expert perspectives derived from a virtual roundtable meeting conducted in February 2023, in which participants discussed the use of the TheraClearX Acne System, including its indication, dual mechanism of action, customizable settings for all skin types, treatment protocols, and practice integration.
Background
Acne is the most common skin condition in the United States, affecting up to 50 million Americans annually.1 It is one of the most common reasons why patients seek treatment from dermatologists.2 Eighty-five percent of adolescents and young adults (12–24 years of age) experience some degree of acne, and occurrence in adults is increasing.1,3 More than 90 percent of acne cases are classified as mild-to-moderate.4
First-line treatment for mild-to-moderate acne is typically a combination of topical and oral medications,2 and early intervention has been shown to reduce the risk of acne scarring and postinflammatory hyperpigmentation (PIH).5,6 However, topical and oral therapies can take time to work, and disappointment from lack of “instant” results may lead some patients to discontinue treatment.7,8 Additionally, some therapies may be unsuitable for certain populations, such as young children, pregnant patients, and individuals with skin of color; they also can be costly and may cause unpleasant side effects, potentially resulting in poor treatment adherence.9,10 The use of noninvasive acne treatment devices has recently generated interest as an alternative acne treatment tool.
Indication
TheraClearX was specifically designed and FDA-cleared for the treatment of mild-to-moderate acne, including comedonal, pustular, and inflammatory acne vulgaris.
Mechanism of Action
The photopneumatic technology of TheraClearX combines a vacuum with pulsed broadband light delivered through a liquid-cooled, handheld delivery system to target many of the key causes of mild-to-moderate acne, both mechanically and thermally.13 It is postulated that the TheraClearX vacuum removes the occlusive material from the infundibulum of the pilosebaceous unit, thereby making the local environment less hospitable to bacterial colonization within the lesion, while the light therapy destroys Cutibacterium acnes (C. acnes) and reduces sebum production (Figures 2 and 3).11–13
System Settings
TheraClearX allows for customization of vacuum and energy settings, as well as offers two insert sizes.
Vacuum settings. Selecting the proper vacuum setting is an important part of TheraClearX treatment because the vacuum targets chromophore and the structure glands closer to the skin surface, allowing more of the treatment area to become irradiated.
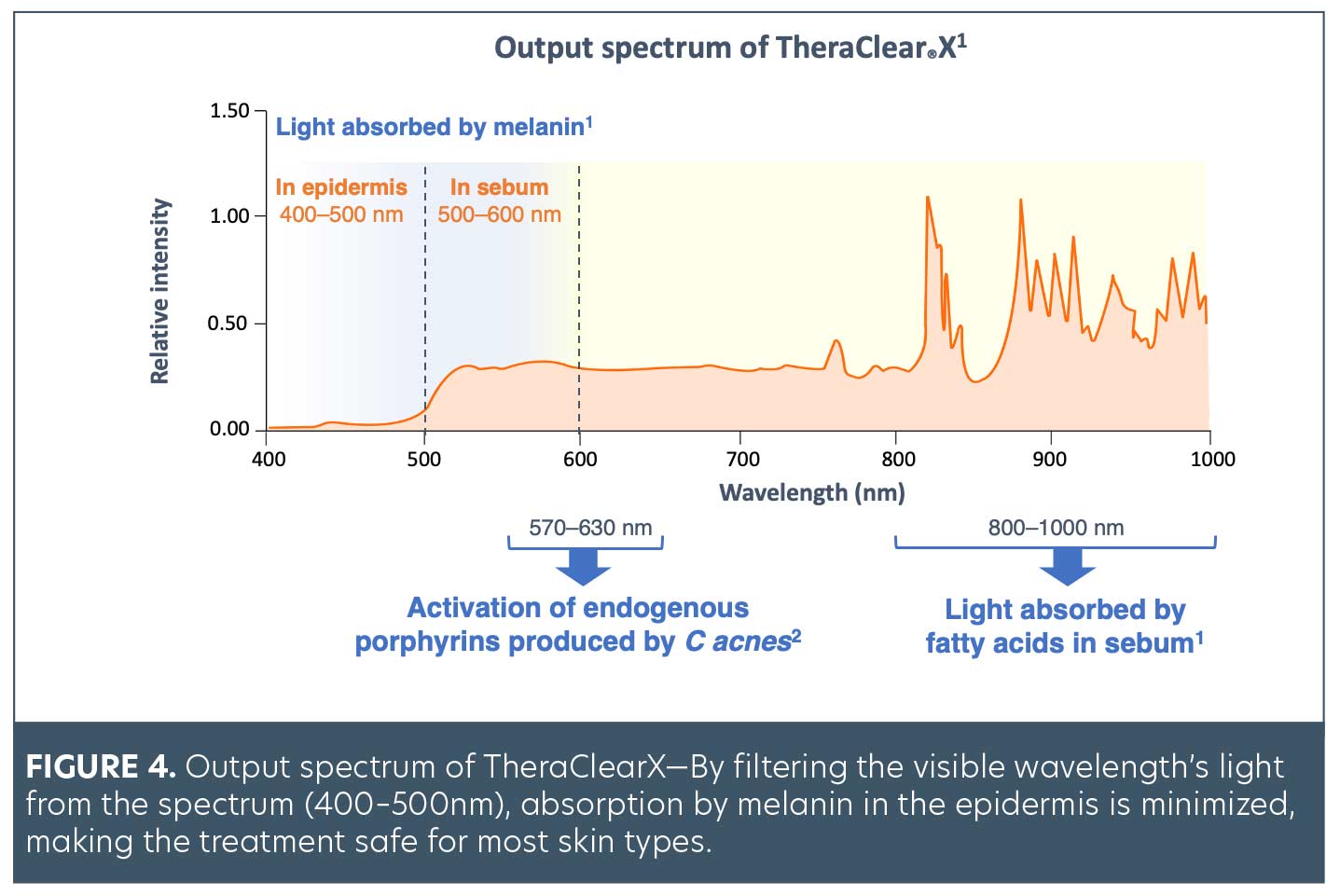
Energy settings. The energy settings of the TheraClearX Acne System are selected based on each patient’s Fitzpatrick skin type. The light spectrum of TheraClearX ranges from 500nm to over 1200nm. Wavelengths in the 570 to 630nm range activate endogenous porphyrins produced by C. acnes,14 and wavelengths in the 800 to 1000nm range are absorbed by the fatty acids in the sebum (Figure 4).14,15
Inserts. TheraClearX inserts are available in two sizes: large and small. The large insert is ideal for larger treatment areas of the face, as well as the chest and back regions. The small insert allows treatment in the contours of the face, including the nose, chin, and upper lip. The ability to treat contours of the face is a key benefit of TheraClearX; other systems are not designed to do so.
Treatments
Initial therapy. Initial treatments with TheraClearX typically comprise 4 to 6 treatment sessions, scheduled one or two weeks apart, depending on disease severity and individual patient preference.
Maintenance therapy. Since acne is a fluid disease with many components of active and dormant disease, maintenance treatments are beneficial to address flare-ups or maintaining clearer skin. Some experts recommend patients come back for maintenance therapy whenever they have a flare-up while others recommend that their patients come back once a month for a few months and then every 6 to 8 weeks or as needed.
Treatment administration. TheraClearX treatments can be performed by physicians, mid-level clinicians (e.g., RNs, NPs, PAs), and/or aestheticians (state laws apply).
Patient Selection
TheraClearX is ideal for teen and adult patients with mild-to-moderate comedonal, pustular, and inflammatory acne vulgaris. Other ideal patient candidates for TheraClearX include patients who are hesitant to use topical or systemic medications or for whom such therapies are contraindicated (e.g., pregnant patients), as well those who are interested in enhancing their existing acne therapy and/or expediting their acne clearance.
The experts recommend that TheraClearX be used concomitantly with other therapies to expedite acne clearance. Theoretically, by opening the pores, the TheraClearX Acne System allows for better penetration of topical medications. Additionally, these experts agree that, compared to other devices, TheraClearX is more effective in improving erythema and inflammatory lesions in patients with acne.
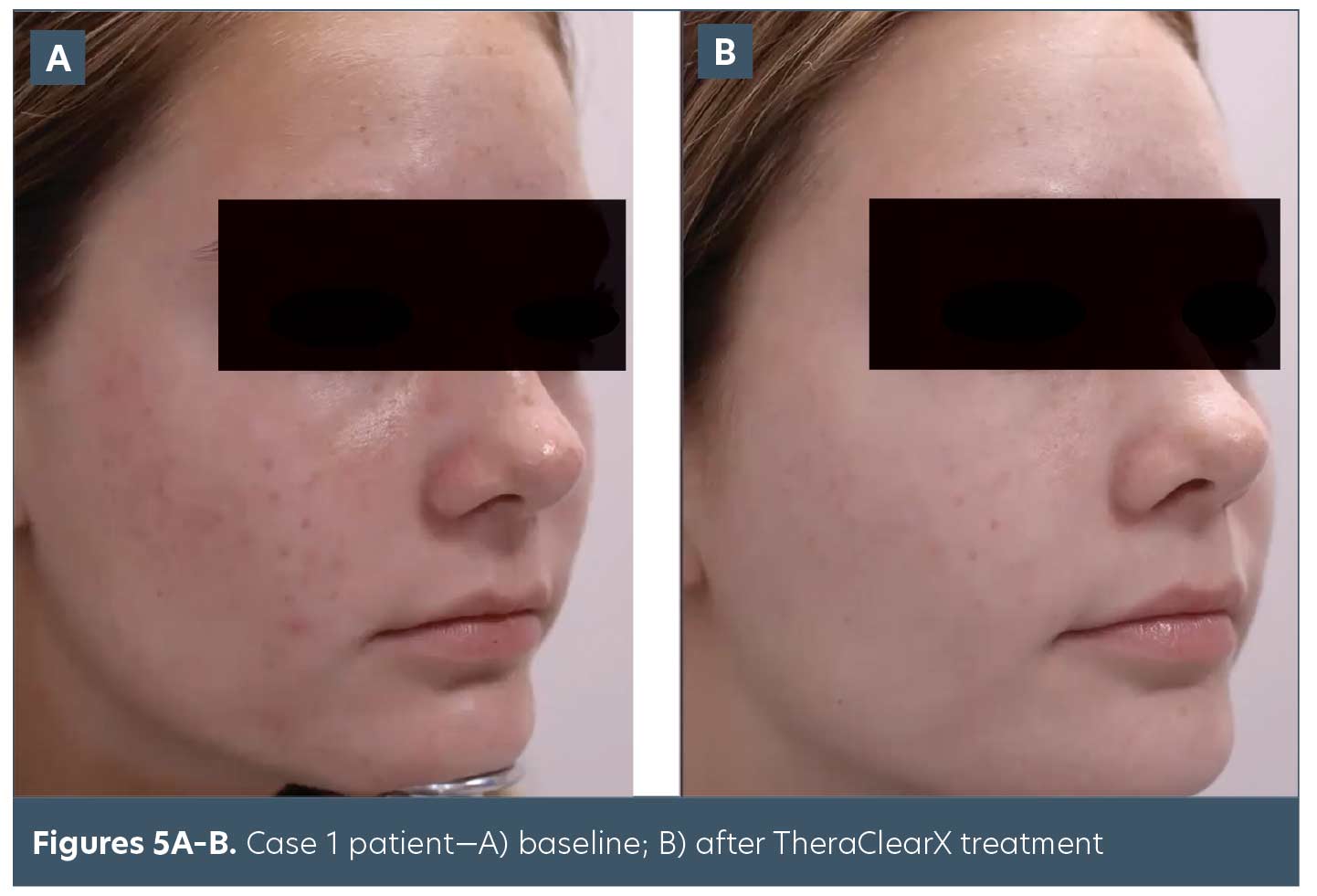
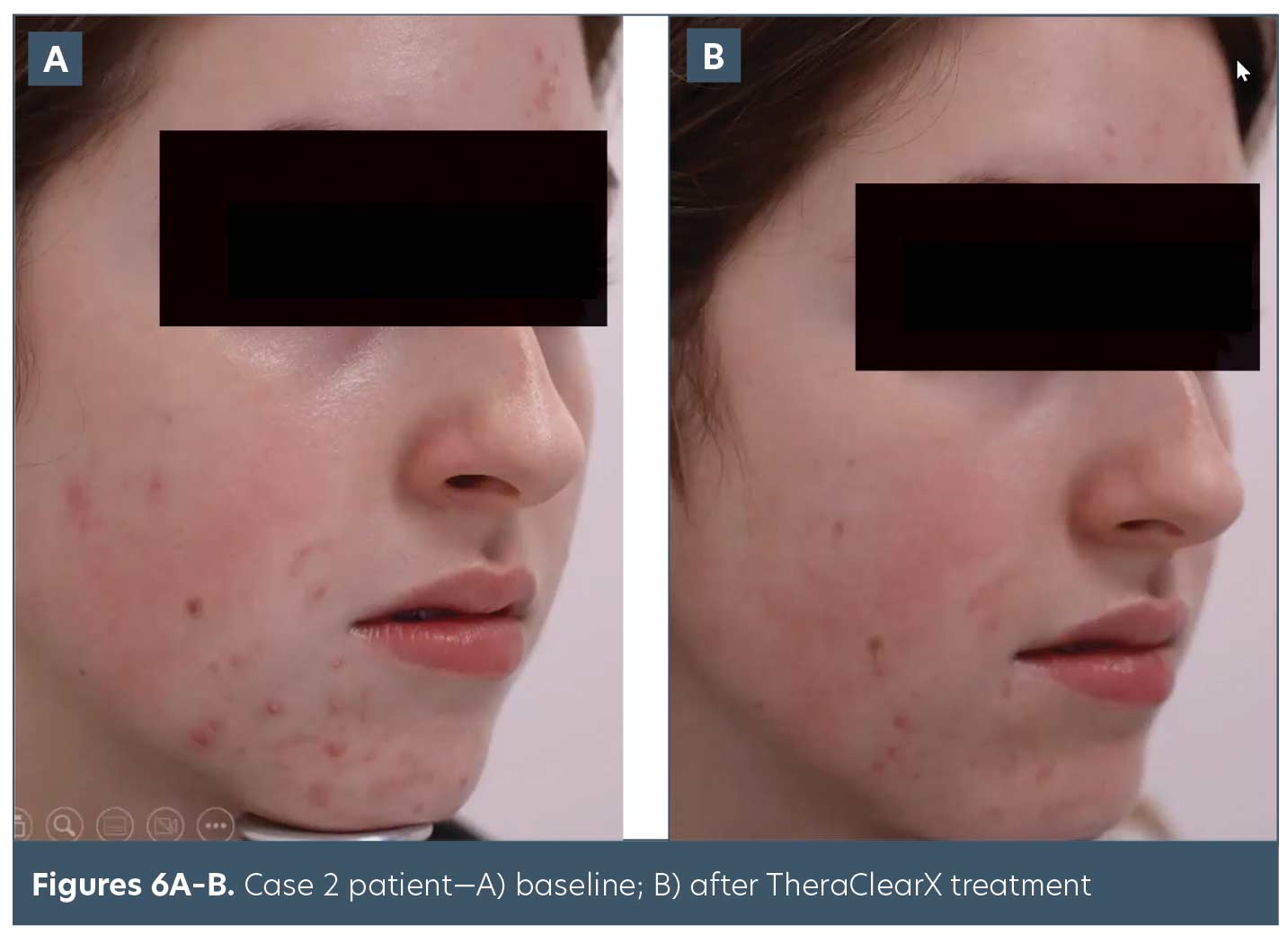
Clinical Cases*
Case 1. The patient in Case 1 (Figures 5A–B) did not present with many inflammatory lesions but was concerned about postinflammatory erythema in her acne scars. Compared to baseline, erythema showed improvement after TheraClearX treatment. The patient was very pleased with results.
Case 2. The patient in Case 2 (Figures 6A–B) had mild-to-moderate, papular, inflammatory lesions with some scarring beginning to form. TheraClearX was used concomitantly with medical treatment. After 4 to 6 treatments, improvements in postinflammatory erythema in the scars were observable. Patient was very happy with her results.
*Clinical cases provided by Dr. Munavalli. Patient photos used with permission.
Patient Expectations
The experts agree it is important to manage expectations when discussing TheraClearX as a potential acne treatment option with patients. As with any treatment, when to expect results; what to expect before, during, and after treatment; and other potential outcomes should be reviewed with each patient.
Results. Most patients experienced visible improvement of their acne as soon as the second treatment session using TheraClearX. In addition, they also typically experience visible improvement in skin texture, pore size and erythema.
Patient satisfaction. The experts report that most of their patients are highly satisfied with their results.
Patient comfort. The experts agree that most patients find TheraClearX to be a comfortable treatment that does not require pretreatment topical anesthetics and no downtime.
Acne flares. Some patients may experience an acne flare after the first treatment with TheraClearX. Patients then typically start to see visible results after the second treatment session and continue to see improvement with consecutive treatments.
Potential side effects. Mild erythema is common but typically resolves within 30 minutes when using TheraClearX, and mild bruising, which typically resolves within 48 to 72 hours post-treatment, may also occur. Superficial erosions of the treatment area, which typically resolve without intervention, may also be visible post-treatment. Pigmentary changes that resolve over time without intervention have rarely been reported. Although rare, blistering, and purpura may be evident for 1 to 3 days following treatment with TheraClearX.
Practice Integration
STRATA Partnership provides clinical training, product education, marketing initiatives, and technical support to assist in the integration of TheraClearX within your practice.
Training. Experts discussed the importance of hands-on training, educational resources, and training the entire office staff to ensure everyone within the practice can discuss TheraClearX with patients. In addition, they discussed the benefits of staff treatments, which creates TheraClearX in-office ambassadors.
Positioning and pricing. Experts recommend positioning TheraClearX as a hybrid medical/aesthetic treatment (e.g., a medical-grade facial) and pricing it comparatively to similar treatments. All agreed that pricing may vary based on the practice’s geographical location and not to underestimate parents’ willingness to pay for their child’s acne treatments.
Conclusion
This report provided expert opinions about the practical use of TheraClearX for the treatment of mild-to-moderate acne. As the treatment of acne evolves, inclusion of alternative therapies, such as TheraClearX, will provide patients and providers with an additional treatment to optimize and expedite acne clearance.
References
- Skin conditions by the numbers. American Academy of Dermatology site. https://www.aad.org/media/stats-numbers. Accessed 22 Sep 2021.
- Perche PO, Peck GM, Robinson L, Grada A, Fleischer AB Jr, Feldman SR. Prescribing Trends for Acne Vulgaris Visits in the United States. Antibiotics (Basel). 2023;12(2):269. Published 2023 Jan 28.
- White GM. Recent findings in the epidemiologic evidence, classification, and subtypes of acne vulgaris. J Am Acad Dermatol. 1998;39(2 Pt 3):S34–37.
- Tan JK, Bhate K. A global perspective on the epidemiology of acne. Br J Dermatol. 2015;172 Suppl 1:3–12.
- Thiboutot D, Dréno B, Sanders V, et al. Changes in the management of acne: 2009–2019. J Am Acad Dermatol. 2020;82(5):1268–1269.
- Alexis AF, Harper JC, Stein Gold LF, Tan JKL. Treating acne in patients with skin of color. Semin Cutan Med Surg. 2018;37(3S):S71–S73.
- Ip A, Muller I, Geraghty AWA, McNiven A, et al. Young people’s perceptions of acne and acne treatments: secondary analysis of qualitative interview data. Br J Dermatol. 2020 Aug;183(2):349-356.
- Ip A, Muller I, Geraghty AWA, Platt D, et al. Views and experiences of people with acne vulgaris and healthcare professionals about treatments: systematic review and thematic synthesis of qualitative research. BMJ Open. 2021;11(2):e041794.
- Snyder S, Crandell I, Davis SA, Feldman SR. Medical adherence to acne therapy: a systematic review. Am J Clin Dermatol. 2014;15(2):87–94.
- Moradi Tuchayi S, Alexander TM, Nadkarni A, Feldman SR. Interventions to increase adherence to acne treatment. Patient Prefer Adherence. 2016;10:2091–2096
- Gold MH, Biron J. Efficacy of a novel combination of pneumatic energy and broadband light for the treatment of acne. J Drugs Dermatol. 2008;7(7):639-642.
- Wanitphakdeedecha R, Tanzi EL, Alster TS. Photopneumatic therapy for the treatment of acne. J Drugs Dermatol. 2009;8(3):239-241.
- Omi T, Munavalli GS, Kawana S, Sato S. Ultrastructural evidence for thermal injury to pilosebaceous units during the treatment of acne using photopneumatic (PPX) therapy. J Cosmet Laser Ther. 2008;10(1):7-11.
- Patwardhan SV, Richter C, Vogt A, et al. Measuring acne using coproporphyrin III, protoporphyrin IX, and lesion-specific inflammation: an exploratory study. Arch Dermatol Res. 2017;309:159–167.
- Data on File. STRATA Skin Sciences. 2023.

