 by Dawnielle C. Endly, DO, and Richard A. Miller, DO
by Dawnielle C. Endly, DO, and Richard A. Miller, DO
Dr. Endly is with Advanced Dermatology Skin Cancer and Laser Surgery Center in Aurora, Colorado. Dr. Miller is with Nova Southeastern University/Largo Medical Center, Dermatology Residency Program and Bay Dermatology and Cosmetic Surgery in Largo, Florida.
J Clin Aesthet Dermatol. 2017;10(8):49–55
Funding: No funding was provided for this study.
Disclosures: The authors have no conflicts of interest relevant to the contents of this article.
Keywords: Oily skin, seborrhea, sebum production, topical retinoids, olumacostat glasaretil, niacinamide, green tea, L-carnitine, isotretinoin, spironolactone, oral contraceptives, botulinum toxin, photodynamic therapy, diode laser
Abstract: One of the most common dermatologic concerns is oily skin, and the demand for effective treatment options is ever apparent. This review article addresses numerous topical treatment options such as retinoids, olumacostat glasaretil, and various cosmeceutical agents. Several systemic and procedural techniques that incorporate isotretinoin, spironolactone, oral contraceptives, botulinum toxin, photodynamic therapy, and lasers are reviewed as well. Each treatment option is analyzed in terms of the proposed mechanism of action, efficacy reported in the literature, and potential adverse effects.
Introduction
 Oily skin is a common dermatologic concern reported by all types of patients, including those without acne, given its association with larger facial pores and an “unclean” or “greasy” appearance (Figure 1). Even a quick search on Amazon.com for “oily skin treatment” reveals 9,907 products geared toward treating this very issue. Price ranges for these products vary from just a few dollars to nearly $1,000 each. One product on the high end of the price spectrum claims to be an “anti-aging fluid that combines modern technology with traditional knowledge of healing ingredients for oily or acne-prone skin.” Regardless of whether consumers believe these statements, this scenario sheds light on the demand for an effective treatment for oily skin. Oily skin is a common dermatologic concern reported by all types of patients, including those without acne, given its association with larger facial pores and an “unclean” or “greasy” appearance (Figure 1). Even a quick search on Amazon.com for “oily skin treatment” reveals 9,907 products geared toward treating this very issue. Price ranges for these products vary from just a few dollars to nearly $1,000 each. One product on the high end of the price spectrum claims to be an “anti-aging fluid that combines modern technology with traditional knowledge of healing ingredients for oily or acne-prone skin.” Regardless of whether consumers believe these statements, this scenario sheds light on the demand for an effective treatment for oily skin.
Oily skin is a common dermatologic concern reported by all types of patients, including those without acne, given its association with larger facial pores and an “unclean” or “greasy” appearance (Figure 1). Even a quick search on Amazon.com for “oily skin treatment” reveals 9,907 products geared toward treating this very issue. Price ranges for these products vary from just a few dollars to nearly $1,000 each. One product on the high end of the price spectrum claims to be an “anti-aging fluid that combines modern technology with traditional knowledge of healing ingredients for oily or acne-prone skin.” Regardless of whether consumers believe these statements, this scenario sheds light on the demand for an effective treatment for oily skin. Oily skin is a common dermatologic concern reported by all types of patients, including those without acne, given its association with larger facial pores and an “unclean” or “greasy” appearance (Figure 1). Even a quick search on Amazon.com for “oily skin treatment” reveals 9,907 products geared toward treating this very issue. Price ranges for these products vary from just a few dollars to nearly $1,000 each. One product on the high end of the price spectrum claims to be an “anti-aging fluid that combines modern technology with traditional knowledge of healing ingredients for oily or acne-prone skin.” Regardless of whether consumers believe these statements, this scenario sheds light on the demand for an effective treatment for oily skin.
Unfortunately, why some people suffer from excessive sebum production while others endure dry skin remains difficult to explain. Numerous factors have been proposed to play a role in the pathogenesis of oily skin. Thus, pinpointing one successful treatment is challenging. Here, we review the physiology of sebaceous glands as well as current and up-and-coming treatment options that can be offered to patients concerned about oily skin. Of note, specific over-the-counter products are not reviewed individually due to lack of objective data. Rather, individual active ingredients are impartially discussed.
Sebaceous Gland Anatomy and Physiology
Aside from the free sebaceous glands on the vermilion lips (Fordyce granules), eyelids (meibomian glands), areolae (Montgomery tubercles), and labia minora and prepuce (Tyson glands), the duct of the sebaceous gland connects to the infundibulum of a hair follicle.[1] These glands are highly concentrated behind the ear and on the face, upper chest, and back, which happens to be the same distribution as acne vulgaris.[2] The major cells comprising sebaceous glands are sebocytes, and these cells disintegrate and release sebum via holocrine secretion. Sebum is a viscous fluid composed of squalene, wax esters, triglycerides, free fatty acids, cholesterol esters, and free sterols.[3,4]
The amount of sebum a person produces varies throughout the course of his or her life. Sebaceous glands are present at birth and display relatively high production of sebum at this time. Shortly after birth, sebum production decreases until puberty, at which time it dramatically increases. Sebum production does not decline again until after menopause for women and around the sixth to seventh decade for men.1 Androgens, particularly 5alpha-dihydrotestosterone (DHT), play a major role in the differentiation and proliferation of sebaceous glands as well as sebum production.[5,6] The average rate of sebum production in adults is 1mg/10cm2 every three hours.[7] When rates are less than 0.5mg/10cm2 every three hours, patients can suffer from xerosis or dry skin. Conversely, when sebum production exceeds 1.5mg/10cm2 every three hours, it is considered excessive and results in seborrhea or oily skin.[1,7]
 The rate of sebum production among different individuals is highly variable, and the explanation as to why this is remains to be fully elucidated. Several factors have been described and can be used to help explain to some patients why their skin might be more oily than others (Table 1). Men in general have higher sebum output attributed to higher testosterone levels, although sebum production does increase during ovulation in women, likely secondary to increased progesterone.[8] Sebum also varies according to one’s environment and the time of year. Several studies have described an increase in sebum production during the spring and summer and in more humid climates.[9,10] In general, in terms of race, Chinese women display notably smaller pore size and lower density while Black individuals have enlarged pore size that can be attributed to higher rates of sebum output.[11,12]
The rate of sebum production among different individuals is highly variable, and the explanation as to why this is remains to be fully elucidated. Several factors have been described and can be used to help explain to some patients why their skin might be more oily than others (Table 1). Men in general have higher sebum output attributed to higher testosterone levels, although sebum production does increase during ovulation in women, likely secondary to increased progesterone.[8] Sebum also varies according to one’s environment and the time of year. Several studies have described an increase in sebum production during the spring and summer and in more humid climates.[9,10] In general, in terms of race, Chinese women display notably smaller pore size and lower density while Black individuals have enlarged pore size that can be attributed to higher rates of sebum output.[11,12]
Despite the pessimistic view of sebaceous glands as a result of their role in oily skin, they do play a vital role in the skin’s well being. Sebaceous glands display endocrine function (particularly androgen synthesis), compose the fetal vernix caseosa, and play a key role in the epidermal barrier and innate immunity.[13–16] Here, we review current and up-and-coming treatment options that may be utilized to help patients with oily skin.
Topical treatments for oily skin
Retinoids. The topical retinoid family comprises vitamin A (retinol); its natural derivatives such as retinaldehyde, retinoic acid, and retinyl esters; and several synthetic vitamin A derivatives such as adapalene and tazarotene. Their effects on the skin are mediated by their interaction with specific nucleic acid receptors. In human skin, the nuclear retinoic acid receptor (RAR) family comprises three forms: RAR-alpha, RAR-beta, and RAR-gamma. One RAR will partner with a retinoid X receptor (RXR) and make a heterodimer.[17] RAR-gamma accounts for about 90 percent of RARs in the epidermis, and RXR-alpha accounts for roughly 90 percent of the RXRs. Thus, the human skin is primarily regulated by paired heterodimers composed of RAR-gamma and RXR-alpha.[18] These heterodimers go on to bind to a specific area in deoxyribonucleic acid (DNA) known as retinoic acid response elements (RARE). Upon binding, transcription of genes encoding proteins necessary for the repair of photodamaged skin, growth and differentiation of keratinocytes, anti-inflammatory actions, and the suppression of sebum production takes place.[19,20]
As early as the 1970s, the use of topical retinoids for various skin diseases, particularly acne vulgaris, began to be increasingly reported.[21] While the role of retinoids in keratinocyte growth and differentiation has been widely recognized for several decades, their influence on the biological function of sebocytes is now becoming more known. Retinoid receptors RAR-alpha, RAR-gamma, and RXR-alpha, beta, and gamma have all been identified in human sebocytes.[22] In vitro, retinoids have been found to significantly reduce sebocyte proliferation, differentiation, and synthesis of sebum.[22–24]
In-vivo studies and clinical experience with topical retinoids have made known the common adverse effect of dry skin, but direct evidence of reduction in sebum output is lacking. Presumably, the dry skin results from normalization of differentiation and proliferation of the keratinocytes and loosening of their adhesion to one another, thereby resulting in flaky skin.[25] One can also speculate that a topical retinoid would also bind to the sebocyte’s retinoid receptors, resulting in decreased sebum production, but evidence has yet to exclusively illustrate that topical retinoids are sebosuppressive.[26]
Both tazarotene and tretinoin have been reported to reduce facial pore size. This is significant in that larger pores have a direct relationship with larger amounts of sebum production.[11] Kang et al[27] reported that [42] percent of subjects treated with tazarotene once daily for 24 weeks achieved a reduction in pore size according to a double-blind, 5-point physician scale. This is significant in comparison to just a 20-percent reduction in pore size in those receiving placebo. A different study found a significant reduction in pore size via a dermatoscopic analyzer after 60 women applied tretinoin 0.025% cream once daily for 90 days.[28] While the direct relationship between pore size and sebum production makes this interesting, one cannot conclude that topical retinoids decrease sebum production given that studies have not distinctly uncoupled this association. Nonetheless, the above evidence and discussion make topical retinoids a worthwhile consideration for treating oily skin.
Olumacostat glasaretil (DRM01). Dermira, a biopharmaceutical company, recently released hopeful data from a Phase 2b trial conducted for a topical sebum production inhibitor, olumacostat glasaretil (OG, formerly DRM01). This novel small molecule functions by inhibiting acetyl coenzyme-A carboxylase (Figure 2).[29–31] This enzyme catalyzes the first rate-limiting step in the synthesis of fatty acids. Triglycerides and fatty acids together make up the largest portion of sebum content; therefore, OG has the potential to decrease sebum output.[32] Further, when evaluated in animal models, topical OG consistently reduced sebaceous gland size.[33]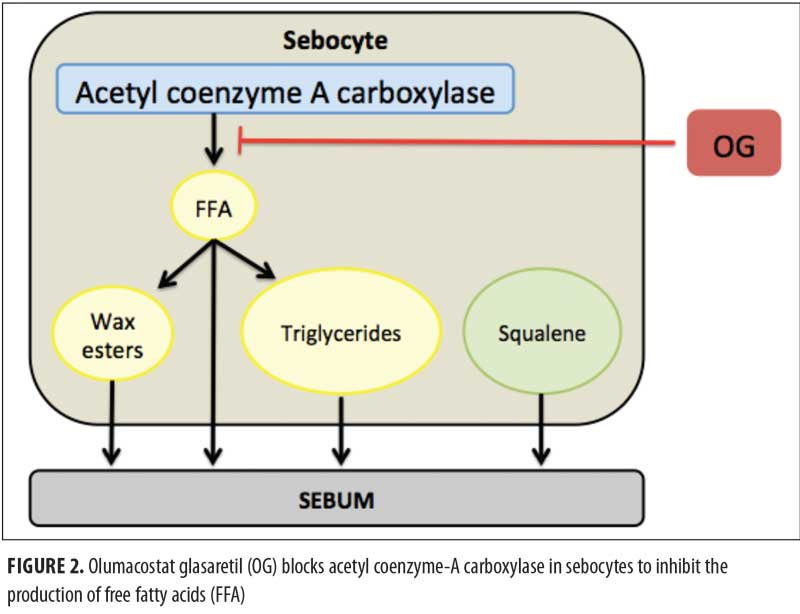
While this molecule was “designed to inhibit sebum production following topical application,” per Dermira’s website, none of the primary endpoints for the trials directly evaluated sebum output or the appearance of oily skin. Rather, the primary endpoints related only to acne lesion counts. The Phase 2a and 2b trials revealed a significant reduction of inflammatory and noninflammatory acne lesion counts following 12 weeks of topical OG at both 7.5% twice daily and 4.0% once daily.[29–31] Topical OG is reportedly well tolerated with no serious treatment-related adverse events and may be an up-and-coming topical agent to treat oily skin. Further studies are warranted to directly evaluate whether topical OG significantly affects sebum production.
Cosmeceuticals. Numerous cosmeceutical products and ingredients make claims that their use will reduce oily skin, but this discussion will be limited to evidence-based ingredients. Draelos et al[34] conducted a double-blind, placebo-controlled study of 100 subjects that revealed topical 2% niacinamide significantly lowered sebum excretion rates after two and four weeks of use. While topical niacinamide may be helpful for those with oily skin, further studies are needed to outline the mechanism of action and ideal treatment regimen.
Another cosmeceutical ingredient with some evidence behind its application for oily skin is green tea. One small study had 10 patients apply a 3% green tea emulsion for eight weeks. When facial skin was evaluated by a sebumeter (a noninvasive photometric device), there was a significant reduction in sebum production compared to baseline.[35] A slightly larger study with 22 participants also found a significant reduction in sebum secretion after 60 days of a topical green tea emulsion.[36] Topical cosmeceuticals containing green tea may prove beneficial for patients with oily skin.
L-carnitine has also become increasingly popular in the discussion of potential ingredients that can decrease the appearance of oily skin. Naturally produced in the body, L-carnitine functions to augment beta-oxidation, the catabolic process by which fatty acids are broken down. Topical 2% L-carnitine has been shown to significantly decrease intracellular fatty acid content in human sebocytes and resulted in significant sebum reduction.[37] While further studies evaluating the efficacy of L-carnitine’s sebosuppressive properties are warranted, it is a reasonable ingredient to recommend to patients concerned about oily skin.
Systemic treatments for oily skin
Isotretinoin. Also known as 13-cis retinoic acid, isotretinoin is an oral retinoid that has been proven to result in the greatest reduction of sebum among all other mentioned treatment options.[38] As described above in the discussion of topical retinoids, 13-cis retinoic acid has also been proven to decrease the size and secretion of sebaceous glands.[23,24] Sebum production decreases by 90 percent during oral isotretinoin therapy and offers some much needed optimism for patients with severe seborrhea.[38]
One year after the completion of isotretinoin therapy, sebum excretion rates have been found to remain significantly suppressed for most individuals.[39] A lower dose of isotretinoin (<0.5mg/kg/day) is often employed when treating oily skin alone without nodulocystic acne, but this lower dose is clearly associated with a higher relapse rate.[40] Overall, up to 17 percent of patients will require a second course of oral isotretinoin despite achieving the recommended cumulative dose of 120 to 150mg/kg.[41,42]
Regardless of the severity of their oily skin, all patients should be reminded that this sizeable reduction in sebum production does not go without adverse effects. Most commonly, patients will experience generalized dry skin, chapped lips, xerophthalmia, and secondary skin infections.[38] Clinicians should educate their patients and provide tips to minimize these common side effects.
One major consideration to discuss with patients prior to starting oral isotretinoin is teratogenicity. This very concern dictates the use of the iPLEDGE system, a computer-based risk management program designed to help eliminate fetal exposure to isotretinoin, even if low doses are being used to treat oily skin. To help prevent this severe adverse risk, sexually active women must use two forms of contraception, and pregnancy testing is required for all female patients of childbearing potential at baseline and monthly until completion of therapy.
Spironolactone. While this potassium-sparing diuretic has classically been utilized in medicine as an antihypertensive agent, it has become increasingly employed by dermatologists for the treatment of oily skin, acne, hirsutism, and androgenic alopecia in women.[43,44] Spironolactone has been shown to directly reduce sebum production when dosed 50 to 200mg daily.[45] In addition to being an alderosterone antagonist, spironolactone also functions as an androgen receptor blocker and an inhibitor of 5alpha-reductase.[38] Human sebocytes contain Type 1 5alpha-reductase, which converts testosterone to the potent androgen 5alpha-dihydrotestosterone (DHT).[46] This androgen plays an important role in inducing sebocyte proliferation. Thus, by inhibiting production of DHT and blocking testosterone and DHT from binding to sebocytes, spironolactone has been proven to inhibit sebocyte proliferation in a dose-dependent manner.[47]
Prior to starting a female patient on spironolactone for oily skin, several potential side effects need to be addressed. In an eight-year follow-up study, no serious immediate or long-term complications attributable to spironolactone for treatment of acne were reported.[48] Still, mild side effects were present in 59 percent of the subjects, with menstrual irregularity being among the most common.[48] Hyperkalemia is often discussed as a potential concern; however, a retrospective study of 974 healthy women taking spironolactone for acne found only 0.72 percent of serum potassium measurements were abnormal compared to the 0.76 percent baseline rate of hyperkalemia.[49] Considering these results and other similar reports, many dermatologists deem routine potassium monitoring as unnecessary for healthy women on spironolactone, but ultimately, lab monitoring is left to each provider’s discretion. Given spironolactone has endocrine effects, it is plausible that it could increase the risk of hormonally dependent cancers, such as breast, ovarian, or endometrial cancers. Contrary to this notion, a large cohort of more than 74,000 patients treated with spironolactone found no evidence of an increased risk of breast, ovarian, or endometrial cancer.[50] These results have been supported by several other recent studies that investigated the potential relationship between spironolactone and risk of hormonally dependent cancers.[51,52] All in all, spironolactone is a safe systemic medication to consider for healthy women seeking treatment for oily skin.
Oral contraceptives. Oral contraceptives are beneficial for oily skin in that they result in a decrease in ovarian and adrenal androgens and increase sex hormone-binding globulin, which limits free testosterone. As described above, androgens stimulate sebocyte proliferation and contribute to seborrhea. Estrogens, all in all, have been found to exhibit an inhibitory effect on excessive sebaceous gland activity in vivo.[53] In order to avoid the risk of endometrial hyperplasia, or even cancer, that can result from unopposed estrogen, it must be used in combination with a progestin.
It is important to consider which progestin is in the combination oral contraceptive, as some progestins have intrinsic androgenic activity. Levonorgestrel, desogestrel, norgestimate, and norethindrone notably have the lowest androgenic activity.[54] Some newer progestins, such as drospirenone or cyproterone acetate, even antagonize the androgen receptors and display antiandrogenic properties.[55,56]
Several studies have shown that oral contraceptives do indeed reduce facial oiliness. In a double-blind, randomized study of 128 women receiving either an ethinyl estradiol/drospirenone combination or an ethinyl estradiol/cyproterone acetate combination, both preparations significantly reduced sebum production.[55] Katz et al57 found a 60-percent relative reduction in sebum output on the cheeks and a 30-percent relative reduction in sebum output on the forehead of 41 women after six cycles of a combination ethinyl estradiol/desogestrel pill. The use of this same combination oral contraceptive was also proven to improve oily skin after just one cycle of treatment.[58]
An important consideration prior to starting an oral contraceptive is the potential increased risk of venous thromboembolism. The newer oral contraceptives have lowered the estrogen doses in an effort to eliminate this risk.[38] Some of the more common but also transient side effects of oral contraceptives include nausea, breast tenderness, and breakthrough menstrual bleeding. Using a combination oral contraceptive that contains the lowest dose of each hormone can limit or even prevent these common adverse effects while still offering the benefit of an improved complexion.[59]
Other treatments for oily skin
Botulinum toxin. Within the last few years, several studies have evaluated the efficacy of botulinum toxin for the treatment of oily skin with promising results. One of the first reports in the literature to mention botulinum toxin’s potential to improve oiliness of the skin appeared in 2008. A retrospective study was performed where 20 subjects with oily skin and large pores were evaluated after intradermal onabotulinum toxin A was injected in the T-zone. One month after treatment, 17 of the 20 subjects had photographic improvement in oiliness and pore size and 17 of the 20 subjects also personally noted an improvement in sebum production.[60] Li et al[61] later performed a double-blind, split-face study in 20 individuals and found a marked decrease in sebum production on the botulinum-treated side. Another significant prospective study evaluated 25 patients with oily skin that received intradermal forehead injections of botulinum toxin and revealed significantly lower sebum production per a sebumeter at one week and one, two, and three months after the injections.[62] Additionally, 91 percent of subjects were satisfied with intradermal botulinum toxin as a treatment for their oily skin.[62]
In terms of the mechanism of action, botulinum toxin cleaves proteins involved in vesicle fusion with the plasma membrane of the presynaptic neuron’s axon terminal. These vesicles contain acetylcholine, and botulinum toxin blocks the release of this neurotransmitter into the synaptic cleft where it would normally bind to a muscarinic receptor on a post-synaptic cell. In sebaceous glands, both immature and mature sebocytes express muscarinic acetylcholine receptors that are important for sebocyte differentiation and sebum production.[61,63,64] Considering the evidence and mechanism of action, intradermal botulinum toxin may be a promising treatment option for oily skin.
Photodynamic therapy. Photodynamic therapy (PDT) following the application of delta-aminolevulinic acid (ALA) is used by some to treat acne vulgaris. ALA is preferentially absorbed by pilosebaceous units, and sebocytes metabolize ALA to light-sensitive protoporphyrin IX (PpIX).[65,66] When exposed to light at a suitable dose and wavelength, PpIX forms cytotoxic free radicals that result in cell destruction and apoptosis of sebocytes. Despite plentiful evidence showing improvement in acne, several studies have failed to show a significant reduction in sebum output after PDT with ALA.[67,68] However, one supportive study found that lower sebum excretion persisted even 20 weeks after multiple PDT sessions, but not after a single PDT session. Histologic evaluation acutely after PDT revealed sebocyte destruction and 20 weeks later revealed smaller sebaceous glands.[69] PDT may be a valuable tool to offer patients concerned about oily skin.
Lasers. There are countless lasers on the market that may be suitable for patients with oily skin. The 1,450nm diode laser appears to be one of the more widely studied lasers for this purpose. Perez-Maldonado et al[70] observed an 18-percent reduction in total sebum collected six weeks after three 1,450nm diode laser treatments. Another study found significant improvement in sebum production in 26 subjects after four treatments on the face with the 1,450nm diode laser.[71] On the other hand, Laubach et al[72] reported that three 1,450nm diode laser treatment sessions did not cause significant changes in sebum excretion. The diode laser is not the most efficacious of the treatment options reviewed, but it still offers a unique treatment modality to address oily skin.
Conclusion
Oily skin is a common chief complaint of dermatologic patients. While sebaceous glands play an integral role in cutaneous function, they are troublesome for some patients when sebum is excessively produced. Numerous treatment options exist to help tame sebum excretion rates, but a clear consensus on the preferred treatment regimen is yet to be described. Each treatment option comes with its own inherent advantages and disadvantages that should be discussed with patients at length, and treatment can then be personalized to each patient’s needs. As more knowledge is gained about the complex pathogenesis behind oily skin, more novel and targeted therapies will hopefully be developed to more satisfactorily treat oily skin.
References
- Schaller M, Plewig G. Structure and function of eccrine, apocrine, and sebaceous glands. In: Bolognia JL, Jorizza JL, Schaffer JV, eds. Dermatology. 3rd ed. Elsevier; 2012:539–544.
- Leyden JJ. New understandings of the pathogenesis of acne. J Am Acad Dermatol. 1995;32:S15–25.
- Camera E, Ludovici M, Galante M, et al. Comprehensive analysis of the major lipid classes in sebum by rapid resolution high-performance liquid chromatography and electrospray mass spectrometry. J Lipid Res. 2010;51:3377–3388.
- Nikkari T. Comparative chemistry of sebum. J Invest Dermatol. 1974;62:257–267.5. Chen W, Zouboulis CC. Hormones and the pilosebaceous unit. Dermatoendocrinol. 2009;1:81–86.
- Rosenfield RL, Deplewski D, Kentsis A, Ciletti N. Mechanisms of androgen induction of sebocyte differentiation. Dermatology. 1998;196:43–46.
- Plewig G, Kligman A. Acne and Rosacea. 3rd ed. Springer; 2000:58–67.
- Kim BY, Choi JW, Park KC, Youn SW. Sebum, acne, skin elasticity, and gender difference- which is the major influencing factor for facial pores? Skin Res Technol. 2013;19:E45–53.
- Man MQ, Xin SJ, Song SP, et al. Variations of skin surface pH, sebum content, and stratum corneum hydration with age and gender in a large Chinese population. Skin Pharmacol Physiol. 2009;22:190–199.
- Wan MJ, Su XY, Zheng Y, et al. Seasonal variability in the biophysical properties of forehead skin in women in Guangzhou City, China. Int J Dermatol. 2015;54:1319–1324.
- Roh M, Han M, Kim D, Chung K. Sebum output as a factor contributing to the size of facial pores. Br J Dermatol. 2006;155:890–894.
- Sugiyama-Nakagiri Y, SugataK, Hachiya A, et al. Ethnic differences in the structural properties of facial skin. J Dermatol Sci. 2009;53:135–139.
- Fritsch M, Orfanos CD, Zouboulis CC. Sebocytes are the key regulators of androgen homeostasis in human skin. J Invest Dermatol. 2001;116:793–800.
- Zouboulis CC, Frimmel S, Ortmann J, et al. Sebaceous glands. In: Hoath SB, Maibach HI, eds. Neonatal Skin: Structure and Function. 2nd ed. Basel: Taylor and Francis; 2003:59–88.
- Fluhr JW, Mao-Qiang M, Brown BE, et al. Glycerol regulates stratum corneum hydration in sebaceous gland deficient (asebia) mice. J Invest Dermatol. 2003;120:728–737.
- Lee D-Y, Yamasaki K, Zouboulis CC, et al. Sebocytes express functional cathelicidin antimicrobial peptides and can act to kill Propionibacterium acnes. J Invest Dermatol. 2008;128:1863–1866.
- Brand N, Petkovich M, Krust A, et al. Identification of a second human retinoic acid receptor. Nature. 1988;332:850–853.
- Fisher GJ, Talwar HS, Xiao JH, et al. Immunological identification and functional quantification of retinoic acid and retinoid X receptor proteins in human skin. J Biol Chem. 1994;269:20629–20635.
- Duell EA, Astrom A, Griffiths CE, et al. Human skin levels of retinoic acid and cytochrome P-450-derived 4-hydroxyretinoic acid after topical application of retinoic acid in vivo compared to concentrations required to stimulate RAR-mediated transcription in vitro. J Clin Invest. 1992;4:1269–1274.
- Baron JM, Heise R, Blaner W, et al. Retinoic acid and its 4-oxo metabolites are functionally active in human skin cells in vitro. J Invest Dermatol. 2005;125:143–153.
- Mills OH, Marples RR, Kligman AM. Acne vulgaris. Oral therapy with tetracycline and topical therapy with vitamin A. Arch Dermatol. 1972;106:200–203.
- Zouboulis CC. Sebaceous gland receptors. Dermatoendocrinol. 2009;1:77–80.
- Tsukada M, Schroder M, Roos TC, et al. 13-cis retinoic acid exerts its specific activity on human sebocytes through selective intracellular isomerization to all-trans retinoic acid and brinding to retinoid acid receptors. J Invest Dermatol. 2000;115:321–327.
- Zouboulis CC, Korge B, Akamatsu J, et al. Effects of 13-cis-retinoic acid, all-transretinoic acid, and acitretin on the proliferation, lipid synthesis and keratin expression of cultured human sebocytes in vitro. J Invest Dermatol. 1991;96:792–797.
- Thielen A-M, Saurat J-H. Retinoids. In: Bolognia JL, Jorizza JL, Schaffer JV, eds. Dermatology. 3rd ed. Elsevier; 2012:2089–2103.
- Gollnick H, Schramm M. Topical therapy in acne. J Eur Acad Dermatol Venereol. 1998;11:S8–29.
- Kang S, Krueger GG, Tanghetti EA, et al. Tazarotene cream in photodamage study group. A multicenter, randomized, double-blind trial of tazarotene 0.1% cream in the treatment of photodamage. J Am Acad Dermatol. 2005;52:268–274.
- Bouloc A, Vergnanini AL, Issa MC. A double-blind randomized study comparing the association of retinol and LR2412 with Tretinoin 0.025% in photoaged skin. J Cosmet Dermatol. 2015;14:40–46.
- Dermira Presents Data from DRM01 Phase 2b Clinical Program at Annual Meeting for Dermatologists. http://investor.dermira.com/phoenix.zhtml?c=253686&p=RssLanding&cat= news&id=2213702. October 21, 2016. Accessed October 22, 2016.
- Dermira Announces Positive Topline Phase 2b Clinical Trial Results for DRM01 in Patients with Facial Acne Vulgaris. http://investor.dermira.com/phoenix.zhtml?c=253686&p=irol-newsArticle&ID=2166760. May 10, 2016. Accessed October 22, 2016.
- Bissonnette R, Poulin Y, Drew J, et al. Olumacostat glasaretil, a novel topical sebum inhibitor, in the treatment of acne vulgaris: A phase IIa, multicenter, randomized, vehicle controlled study. J Am Acad Dermatol. 2017;76:33–39.
- Green RS, Downing DT, Pochi PE, Strauss JS. Anatomical variation in the amount and composition of human skin surface lipid. J Invest Dermatol. 1970;54:240–247.
- Hunt DWC, Hofland HEJ. DRM01, a novel acetyl coenzyme A carboxylase inhibitor, reduces sebum production. J Invest Dermatol. 2014;134:S70.
- Draelos ZD, Matsubara A, Smiles K. The effect of 2% niacinamide on facial sebum production. J Cosmet Laser Ther. 2006;8:96–101.
- Mahmood T, Akhtar N, Khan BA, et al. Outcomes of 3% green tea emulsion on skin sebum production in male volunteers. Bosn J Basic Med Sci. 2010;10:260–264.
- Mahmood T, Akhtar N, Moldovan C. A comparison of the effects of topical green tea and lotus on facial sebum control in healthy subjects. Hippokratis. 2013;17:64–67.
- Peirano RI, Hamann T, Dusing HJ, et al. Topically applied L-carnitine effectively reduces sebum secretion in human skin. J Cosmet Dermatol. 2012;11:30–36.
- Gollnick H, Cunliffe W, Berson D, et al. Management of acne: a report from a Global Alliance to Improve Outcomes in Acne. J Am Acad Dermatol. 2003;49:S1–37.
- Hughes BR, Cunliffe WJ. A prospective study of the effect of isotretinoin on the follicular reservoid and sustainable sebum excretion rate in patients with acne. Arch Dermatol. 1994;130:315–318.
- Stainforth JM, Layton AM, Taylor JP, Cunliffe WJ. Isotretinoin for the treatment of acne vulgaris: which factors may predict the need for more than one course? Br J Dermatol. 1993;129:297–301.
- Cunliffe WJ, Layton A, Knaggs HE. Retinoids. In: Saurat JH, ed. Retinoids: 10 Years On. Karger; 1991:272–280.
- Leyden JJ. The role of isotretinoin in the treatment of acne: personal observations. J Am Acad Dermatol. 1998;39:S45–49.
- Muhlemann MF, Carter GO, Cream JJ, Wise P. Oral spironolactone: an effective treatment for acne vulgaris in women. Br J Dermatol. 1986;115:227–232.
- Burke BM, Cunliffe W. Oral spironolactone therapy for female patients with acne, hirsutism, or androgenic alopecia. Br K Dermatol. 1985;112:124–125.
- Goodfellow A, Alaghband-Zadeh J, Carter G, et al. Oral spironolactone improves acne vulgaris and reduces sebum excretion. Br J Dermatol. 1984;111:209–214.
- Fritsch M, Orfanos CE, Zouboulis CC. Sebocytes are the key regulators of androgen homeostasis in human skin. J Invest Dermatol. 2001;116:793–800.
- Akamatsu H, Zouboulis CC, Orfanos CE. Spironolactone directly inhibits proliferation of cultured human facial sebocytes and acts antagonistically to testosterone and 5alpha-dihydrotestosterone in vitro. J Invest Dermatol. 1993;100:660–662.
- Shaw JC, White LE. Long-term safety of spironolactone in acne: results of an 8-year followup study. J Cutan Med Surg. 2002;6:541–545.
- Plovanich M, Weng QY, Mostaghimi A. Low usefulness of potassium monitoring among healthy young women taking spironolactone for acne. JAMA Dermatol. 2015;151:941–944.
- Mackenzie IS, Morant SC, Wei L, et al. Spironolactone use and risk of incident cancers: a retrospectice, matched cohort study. Br J Clin Pharmacol. 2017;83:653–663.
- Biggar RJ, Andersen EW, Wolhfahrt J, Melbye M. Spironolactone use and the risk of breast and gynaecologic cancers. Cancer Epidemiol. 2013;37:870–875.
- Mackenzie IS, Macdonald TM, Thompson A, et al. Spironolactone and risk of incident breast cancer in women older than 55 years: retrospective, matched cohort study. BMJ. 2012;345:e4447.
- Heemers HV, Tindall DJ. Androgen receptor (AR) coregulators: a diversity of functions converging on and regulating the AR transcriptional complex. Endocr Rev. 2007;28:778–808.
- Speroff L, DeCherney A. Evaluation of a new generation of oral contraceptives. Obstet Gynecol. 1993;81:1034–1047.55. van Vloten WA, van Haselen CW, van Zuuren EJ, et al. The effect of 2 combined oral contraceptives containing either drospirenone or cyproterone acetate on acne and seborrhea. Cutis. 2002;69:2–15.
- Raudrant D, Rabe T. Progestogens with antiandrogenic properties. Drugs. 2003;63:463–492.
- Katz HI, Kempers S, Akin MD, et al. Effect of a desogestrel-containing oral contraceptive on the skin. Eur J Contracept Reprod Health Care. 2000;5:248–255.
- Prilepskaya VN, Serov VN, Zharov EV, et al. Effects of a phasic oral contraceptive containing desogestrel on facial seborrhea and acne. Contraception. 2003;68:239–245.59. Koulianos GT. Treatment of acne with oral contraceptives: criteria for pill selection. Cutis. 2000;66:281–286.60. Shah AR. Use of intradermal botulinum toxin to reduce sebum production and facial pore size. J Drugs Dermatol. 2008;7(9):847–850.
- Li ZJ, Park SB, Sohn KC, et al. Regulation of lipid production by acetylcholine signaling in human sebaceous glands. J Dermatol Sci. 2013;72:116–122.
- Rose AE, Goldberg DJ. Safety and efficacty of intradermal injection of botulinum toxin for the treatment of oily skin. Dermatol Surg. 2013;39:443–448.
- Kurzen H, Berger H, Jager C, et al. Phenotypical and molecular profiling of the extraneuronal cholinergic system of the skin. J Invest Dermatol. 2004;123:937–949.
- Kurzen H, Schallreuter KU. Novel aspects in cutaneous biology of acetylcholine synthesis and acetylcholine receptors. Exp Dermatol. 2004;13:27–30.
- Ibbotson SH. Topical 5-aminolaevulinic acid photodynamic therapy for the treatment of skin conditions other than nonmelanoma skin cancer. Br J Dermatol. 2002;146:178–188.
- Kosaka S, Kawana S, Zouboulis CC, et al. Targeting of sebocytes by aminolevulinic acid-dependent photosensitization. Photochem Photobiol. 2006;82:453–457.
- Pollock B, Turner D, Stringer MR, et al. Topical aminolaevulinic acid photodynamic therapy for the treatment of acne vulgaris: a study of clinical efficacy and mechanism. Br J Dermatol. 2004;51:616–622.
- Horfelt C, Stenquist B, Larko O, et al. Photodynamic therapy for acne vulgaris: a pilot study of the dose-response and mechanism of action. Acta Derm Venereol. 2007;87:325–329.
- Hongcharu W, Taylor CR, Chang Y, et al. Topical ALA-photodynamic therapy for the treatment of acne vulgaris. J Invest Dermatol. 2000;115:183–192.
- Perez-Maldonado A, Runger TM, Krejci-Papa N. The 1,450-nm diode laser reduces sebum production in facial skin: a possible mode of action of its effectiveness for the treatment of acne vulgaris. Lasers Surg Med. 2007;39:189–192.
- Yeung CK, Shek SY, Yu CS, et al. Treatment of inflammatory facial acne with 1,450-nm diode laser in type IV to V Asian skin using an optimal combination of laser parameters. Dermatol Surg. 2009;35:593–600.
- Laubach HJ, Astner S, Watanabe K, et al. Effects of a 1,450 nm diode laser on facial sebum excretion. Lasers Surg Med. 2009;41:110–115.

