J Clin Aesthet Dermatol 2020;13(1):E53–E58
 by Dr. Martyn King; Dr. Lee Walker; Dr. Cormac Convery; and Emma Davies, RN, NMP
by Dr. Martyn King; Dr. Lee Walker; Dr. Cormac Convery; and Emma Davies, RN, NMP
ABSTRACT: Vascular occlusion has been cited as the most severe and feared early complication in aesthetic treatment1 and the incidence appears to be on the increase. There are several steps practitioners can take to minimize this risk and early identification and treatment of this complication is paramount. This guideline undertakes to educate and inform practitioners on steps to minimize risk, diagnose and manage a vascular occlusion in order to prevent skin necrosis.
KEYWORDS: Dermal filler, complication, injectable, skin necrosis, vascular compromise, vascular occlusion, cosmetic medicine
Expert Group: Dr Martyn King (Chair); Emma Davies, RN NIP (Vice Chair); Sharon King, RN, NIP; Dr. Cormac Convery, Dr. Lee Walker, Linda Mather, RN, NIP
Consensus Group: Helena Collier, RN, NIP; Dr. Ben Coyle; Dr. Ravi Jain; Dr. Sam Robson; Mr. Taimur Shoaib; Lou Sommereux, RN, NIP; Frances Turner-Traill, RN, NIP
Definition
A vascular occlusion occurs when blood is no longer able to pass through a blood vessel.1 It may be a complete occlusion or partial occlusion, resulting in a diminished blood supply. A vascular occlusion may be caused by an internal obstruction, such as a blood clot, a foreign body, such as filler material, or occur as a result of external compression. If left untreated, a vascular occlusion of a blood vessel supplying the skin can result in skin necrosis and tissue death.
Necrosis can be defined as, “the death of most or all of the cells in an organ or tissue due to disease, injury, or failure of the blood supply.”2
Unlike normal cell death (i.e., apoptosis), which is a programmed and ordered phenomenon, necrosis is the accidental death of the cell caused by various mechanisms, such as an insufficient supply of oxygen, thermal or mechanical trauma, or irradiation. Cells that are undergoing necrosis swell, then burst (i.e., cytolysis), releasing their contents into the surrounding area. This results in a locally triggered inflammatory reaction characterized by swelling, pain, heat, and redness. The necrotic cells are subsequently phagocytosed and removed by the immune system.
Introduction
The three proposed mechanisms of vascular occlusion associated with cosmetic injection are:3
- Intravascular embolism
- Extravascular compression
- Vascular spasm.
A study by Chang et al4 failed to show that vascular compression was reproducible in an animal model, although a case report by Lima et al5 showed that tissue hypoperfusion occurred following vascular compression identified using high frequency ultrasound. Vascular occlusion is possible via several mechanisms following cosmetic injections; however, intravascular embolism is the pathophysiology best supported by the evidence.3
When a blood vessel is inadvertently injected with filler material, the normal circulation can become impaired, leading to reduced tissue perfusion and compromise of the tissue relating to its angiosome.6 Most soft tissue fillers used in cosmetic practice consist of hyaluronic acid, and although hyaluronic acid is well-tolerated outside the vessel wall, it is highly inflammatory within blood vessels. Using histopathologic analysis of tissue obtained from rabbit ears, experimental study demonstrated that biphasic hyaluronic acid globules within an arterial vessel lumen produces intense vessel wall inflammation and spasm.6 It is speculated that this inflammation and spasm restricts blood flow and leads to further dispersal of foreign material into the adjacent vascular territory. It is apparent that complications associated with hyaluronic acid injection into an artery involve not just embolus with inflammation of the vessel wall, but spasm of the surrounding anastomoses to limit further spread and protection against wider areas of necrosis.6
Many cases of vascular compromise occur immediately with injection1 and the practitioner needs to be aware of the signs of this. However, there are several published papers that describe delayed onset of symptoms of vascular occlusion.1,7,8,9
Although the exact mechanism for a delayed onset of presentation is not properly understood, there are several proposed mechanisms:
1. Due to the hydrophilic nature of hyaluronic acid fillers in attracting water molecules, this can lead to delayed swelling posttreatment and a subsequent external compression of a vessel.
2. An embolus might obstruct a vessel in an area of skin that has a poor collateral circulation, and, although immediate signs of occlusion fail to manifest, the poor collateral supply fails to deliver enough nutrition to the skin over the following hours when signs of vascular compromise occur.1
3. Delayed vascular occlusion might be due an intra-arterial injection, which does not initially occlude the vessel but creates a nidus for platelet aggregation, subsequently leading to a blockage.
4. An intra-arterial injection might initially occur in a larger vessel or at a bifurcation point where it can later become dislodged, leading to an occlusion in a terminal branch.
Incidence
Although necrosis can occur as a result of many aesthetic treatments, it is most commonly associated with the injection of soft tissue fillers. The incidence of necrosis related to the injection of collagen has been reported at 9 in 100,000 cases, of which 50 percent of cases were in the glabellar region,10 and for all dermal fillers, an incidence of 1 in 100,000 cases.11 However, it is widely recognized that although the incidence of vascular occlusions following injection of soft tissue filler is increasing, likely due to increasing popularity of these treatments and procedures being performed by less experienced practitioners, incidence data is very poor due to under-reporting. In an internet-based survey completed by 52 experienced injectors worldwide, 62 percent reported one or more intravascular events.12,13
Skin necrosis has occurred as a result of injection of all types of dermal filler, including collagen, hyaluronic acid, Polymethylmethacrylate beads (PMMA), calcium hydroxylapatite, and autologous fat.7
Signs and Symptoms of Vascular Occlusion (TABLE 1)
Pain. Severe pain is usually experienced by the patient at the time of injection. However, if local anesthetic has been used (either topically, a nerve block, or administered with the product) this symptom can be less reliable. Extraordinary pain is not a feature of soft tissue filler treatments, and if a patient complains of sudden or escalating pain during treatment or in the hours following treatment, this should alert the practitioner to the possibility that a vascular occlusion has occurred and warrants an urgent review. Injectors should be aware that pain distant from the injection area can also be a warning sign of vascular occlusion.1,7,8,10,13,14,15
Blanching. When the vasculature is affected, the area will often initially look pale, white, or dusky, due to the reduction in blood supply to the affected tissue. This color will remain after removal of the needle or cannula. The blanching might initially be transient and local, but if unresolved, the pattern of the blanching will become reticulated or irregular, following the same path as the blood supply that has been restricted. This blanching might be masked initially, if adrenaline or certain topical anesthetics have been used.1,7,8,10,13,14,15
Dusky, purple discoloration. This is more typical several hours following treatment and is due to the accumulation of deoxygenated blood in the affected tissues. The appearance can mimic that of bruising, but bruises do not blanch, as they are caused by blood leaking into the skin.1,7,15
Coolness. When the blood supply has been affected, the tissues are not being perfused, so the temperature will be reduced; this will not be apparent immediately following injection.15
Areas of Caution
It is essential to consider that there are no safe areas of the face and all areas should be treated with the same respect and anatomical knowledge. Special attention should be given when injecting into the midline, as this area appears to be a more dangerous area to inject in terms of vascular occlusion and cases of visual loss, as documented in a literature review.16,17
Evidence dictates that there are two main areas on the face that have a higher incidence of vascular occlusion following soft tissue augmentation with filler: the glabellar region and the nasolabial fold, nasal tip, and alar triangle.
Glabellar region. Supratrochlear artery, supraorbital artery and cutaneous branches of the ophthalmic artery.
Fifty percent of cases of vascular occlusion occur as a result of intravascular injection of dermal fillers into the glabellar region due to the poor collateral circulation in this watershed area.1,10,11,13,15,17
Nasolabial fold, nasal tip, and alar triangle. Facial artery,15 angular artery15 and lateral nasal artery.
The nasal tip and alar are also commonly affected due to these being supplied by an end artery with limited collateral blood flow.1 The angular artery turns sharply within the alar triangle and is prone to external compression or inadvertent injection leading to vascular occlusion.10,11,15
Minimizing the risk of vascular occlusion
- Practitioners should have a detailed knowledge of the three-dimensional anatomy of the area being treated.15,18 They must also understand the distribution and depth of vessels of the target area and possible variations of these.
- Aspiration prior to injection is encouraged, so as to ascertain that the injection is not intravascular. Although it is well known that aspiration might not always be possible, even if the needle tip is within a vessel.1,7,15,17,19 Practitioners should not depend solely on aspiration as a stand-alone test for safety. Evidence from Casabona et al20 showed the reliability of aspiration to be 53 percent. Van Loghem and colleagues21 measured reliability between 33 percent and 63 percent, depending on factors such as needle size, pull back time, and needle length. Torbeck et al22 suggested that the rheology of the filler used is a major factor in gaining a true positive aspirate. Rheology determines the amount of pull back and time of pull back; these parameters ranged from 0.5 to 30 seconds using either 0.2ml or 0.5ml.22 Therefore, injectors should adjust the amount of time to aspirate and adjust the volume pulled back on the syringe if this test is to have any reliance.
- Practitioners should employ a slow injection technique under low pressure with the filler delivered at the appropriate depth and tissue plane.7,13
- The smallest possible volume to achieve the desired effect should be used. Avoid overfilling an area,1 and if more product is required, a repeat treatment in 7 to 14 days is a safer option.13,15,17
- Avoid areas of previous scarring, as deep tissue scars can fix arteries in place and make them easier to penetrate.1,15
- Avoid bolus injections in areas at risk of vascular occlusion.25
- Avoid using adrenaline, or products containing adrenaline, as this can mask the blanching produced by an occlusion.1,8
- Injection of local anesthetic or premixed with a soft tissue filler can mask any pain experienced by the patient in the event of a vascular occlusion, and the practitioner should not rely on this warning sign alone.
- Do not inject into the tip of the nose, as this is a highly vascular area with restricted tissue space.
- Use caution when injecting into the glabellar region.13 Injections should be placed superficially (intradermal) and medially.17 Practitioners are encouraged to use botulinum toxin in the glabella first to reduce severity of wrinkles before injecting soft tissue filler. This area should only be injected by experienced injectors.
- The use of blunt-ended cannulas of 25G or larger bore diameters are less likely to penetrate vessels and lead to an inadvertent intravascular injection.1,15 The risk of penetration of a vessel wall with a blunt-tipped cannula increases with the force used and the age of the patient.
- Patient selection is paramount; be cautious when treating patients who have undergone rhinoplasty10 or other surgical procedures, as the anatomy and vasculature can be altered.
- Pay attention when injecting. Look for warning signs and listen to your patient!
- The risk of vascular occlusion is higher when using fillers of a greater density (higher G prime) as these have the potential to create a greater extrinsic pressure on a vessel.
- Practitioners, particularly less experienced practitioners, should consider using only reversible hyaluronic acid fillers, as this can make the management of a vascular occlusion easier due to its hydrolysis by hyaluronidase.1
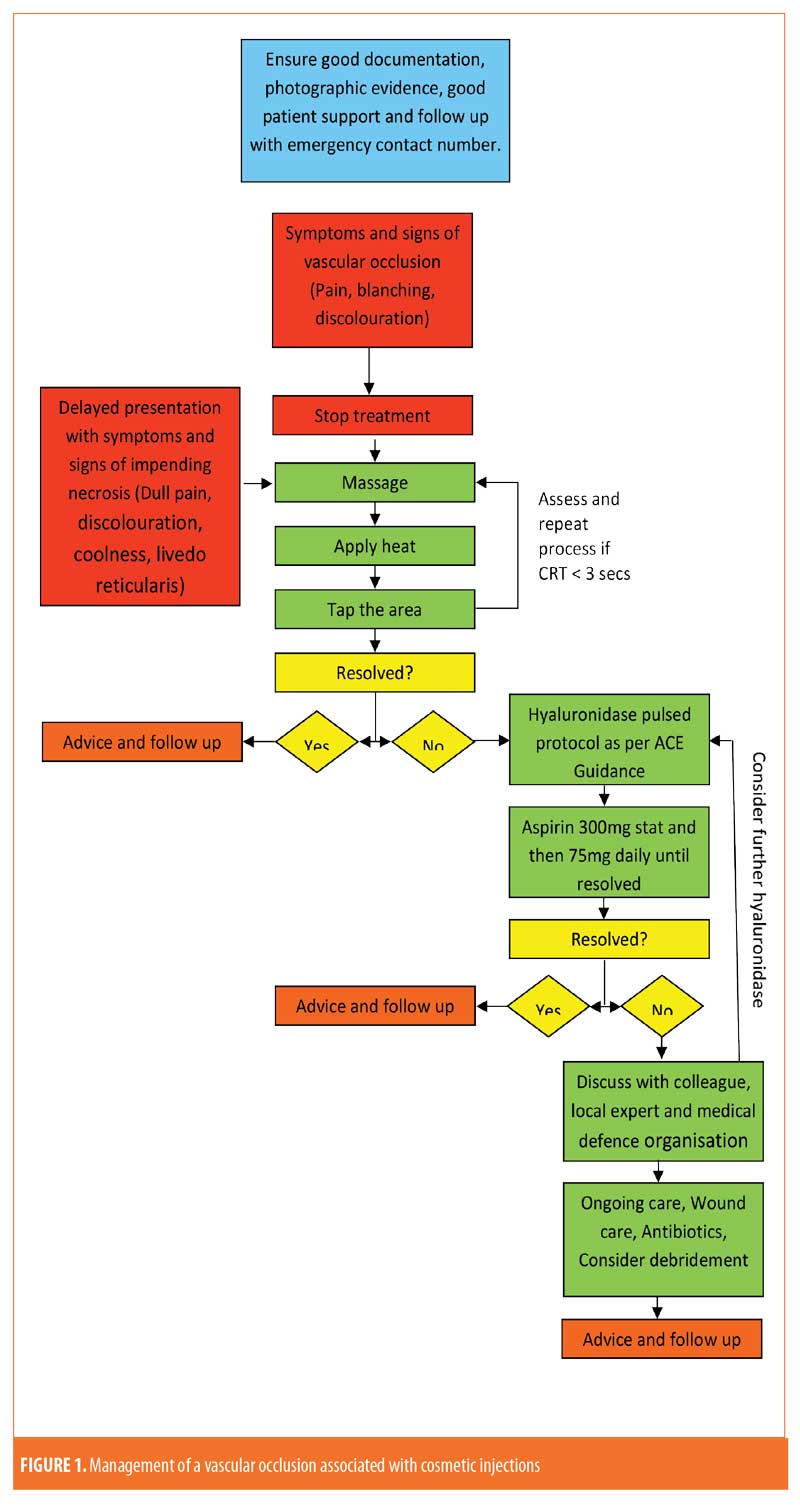
Treatment of Vascular Occlusion
A vascular occlusion can result from arterial occlusion by direct injection into an artery or embolization of product, typically presenting immediately with acute pain and blanching. It can also result from venous occlusion from external compression of a vessel by soft tissue filler or subsequent edema and compression, more often with hyaluronic acid fillers. Venous occlusion usually presents later with a less severe, dull pain, or no pain at all, and dark discoloration of the skin.13,14
In some cases, it might be possible to resolve the occlusion with conservative measures, such as massage, tapping, and/or heat applied to the area. However, if conservative methods fail, hyaluronidase should be administered without delay when a hyaluronic acid dermal filler has been used.
Immediately stop treatment. As soon as the practitioner suspects the blood supply has been compromised, typically due to pain and blanching in the injected area, the most important step is to immediately discontinue injecting any more product, and if possible, aspirate any product when withdrawing the needle or cannula.23 Inform the patient of the problem. If the practitioner is not confident or is inexperienced in the management of a vascular occlusion, they should quickly seek the immediate advice of a more experienced practitioner. A vascular occlusion needs prompt management, as the risk of tissue damage and skin necrosis increases over time.7,8,10,11,13,14,17,18
Assess capillary refill time (CRT). The capillary refill time should be assessed on the affected and unaffected sides. Capillary refill time (CRT) is defined as the time needed by a distal body region, such as the fingertip, to regain the original color after having been compressed. Sansone et al24 considers a normal physiological capillary refill time to be two and three seconds, for men and women under 65 years of age, respectively, and four seconds for elderly patients of both sexes. CRT greater than three seconds can be indicative of a vascular compromise. A fast capillary refill time on a background of a bluish skin discoloration can indicate venous insufficiency.15 It is prudent to observe and assess skin color and capillary refill prior to treatment as a benchmark for posttreatment assessment.
To test capillary refill time, moderate pressure with either a finger or small, firm, flat object should be applied to the area being assessed for five seconds and then released. The time for the skin to return to its normal color should be observed and recorded. The test should be conducted over the entire area and on both the affected and unaffected sides for comparison. If capillary refill time is sluggish, but not less than three seconds, an initial attempt using conservative measures, such as massage, tapping, and heat should be used. If capillary refill time is not improved by conservative measures or CRT is greater than three seconds, practitioners should employ the ACE Group high-dose pulsed hyaluronidase protocol.25
Firmly massage the area. Firm and prolonged massage can encourage blood flow and remove any obstruction caused by a foreign body occluding a vessel. Massage might be required for several minutes.7,8,10,11,13,14,17,26
Apply heat. Heat will encourage vasodilatation and increase blood flow to the area.7,8,10,11,13,14,17,18,19,23,26
Tap the area. Tapping over an area can dislodge intra-arterial emboli located at the site or further up in the vessel.14,19
Inject with hyaluronidase.1,7,10,11,13,14,18,19,23,26 Where hyaluronic acid fillers are the culprit, injecting with hyaluronidase can relieve the problem before complications even occur.25 Practitioners must remember that this is a time-critical event, and that test patching is not required if hyaluronidase is used for a vascular occlusion, as the risk of tissue damage is generally greater than the risk of anaphylaxis. As with any aesthetic treatments, it is important to have appropriate resuscitation equipment available to deal with any potential complications.15 There is some evidence to suggest that using hyaluronidase when a non-hyaluronic acid soft tissue filler has been injected can lessen the subsequent tissue damage, due to dissolving native hyaluronic acid and decreasing pressure on the blood supply.11,23
Practitioners should employ the ACE Group High-dose, Pulsed Hyaluronidase Protocol.25 Despite the simplicity of the intervention, it has prevented necrosis in virtually all cases since it has been implemented, even up to 48 hours after the initial treatment. The protocol involves repeated administration of relatively high doses of hyaluronidase into the whole area of compromised tissue, not just where the filler was injected,14 repeated hourly until clinical resolution is observed, denoted by improvements in capillary refill, skin color and pain. This technique has also led to successful and complete recovery without the need for any adjunctive treatment.2
There is contradictory evidence to suggest that hyaluronidase diffuses into the lumen of blood vessels even when injected externally to it. However, when treating a vascular occlusion, it is not necessarily essential to inject directly into the vessel, but the surrounding area is also likely to result in dissolution of the product. Indeed, the injection of hyaluronidase into the subcutaneous plane, rather than attempting intra-arterial injection, has shown more favorable outcomes.27
Aspirin.1,15 Following the evidence for the use of aspirin in cardiovascular disease, in order to limit platelet aggregation, clot formation, and further vascular compromise, a stat dose of 300mg should be given immediately, followed by 75mg a day until the vascular occlusion has resolved where there are no contraindications.28 Concomitant use of gastric protection medication might be recommended in some patients. If treatment of a vascular occlusion has failed, necrosis might ensue. The patient should be monitored regularly, and if tissue breakdown occurs, a referral for specialist management and care might be appropriate (Refer to ACE Guidelines on Necrosis).
Antibiotics.1,10,13,23 Necrosis consists of dead cells and tissue and is prone to secondary opportunistic infection. Depending on the extent of necrosis, topical and/or oral antibiotics might be required to promote healing and to prevent further complications. Antiherpetic medication might be necessary if necrosis occurs in a susceptible patient in a perioral distribution.1,11 In the case of a treated vascular occlusion without any signs of skin damage, antibiotics should not be given for prophylaxis.
Superficial debridement. Referral to a plastic surgeon might be required for removal of dead tissue to promote healing.7,10,13,17,18
Wound care management. Apply appropriate dressings and wound care to encourage healing.1,10,17
Pain management. Pain management needs to be considered in cases of necrosis; although over-the-counter medication might be all that is required, necrosis can cause severe pain requiring opioid analgesia.
Refer. It is always sensible to involve other practitioners experienced in the management of vascular occlusion for further advice and/or treatment.
Speak to your medical defense organization. A vascular event can be a distressing ordeal for both patient and practitioner. Whether or not it is managed well and resolved, a claim may ensue.
Other Treatment Options
Hyperbaric oxygen therapy (HBOT) has been successfully used in nasal tip grafting following cases of cancer or trauma with positive results on revascularization, although there is limited evidence to recommend this for necrosis secondary to aesthetic procedures.10,13,29 Several case reports have described an improvement in aesthetic outcomes using HBOT1 but some authors do not feel that the costs, risks and inconvenience is warranted.30 HBOT increases the supply of oxygen to the compromised tissue and helps to remove toxic free radicals.23,29
Low molecular weight heparin1,11 has been used to prevent thrombosis and embolization in one case report,31 although there is not enough evidence to recommend this as a standard treatment.
Oral vasodilators, including cGMPspecific phosphodiesterase type 5 (PDE5) inhibitors or prostaglandin E1 (PGE1)1 have also been advised for the treatment of vascular occlusion, but evidence is lacking for their wider use for this indication.11
Treatment No Longer Recommended
Nitroglycerin paste. Two-percent nitroglycerin (glyceryl trinitrate) paste induces vasodilatation and increases blood flow to the area. It has been recommended to be used topically in the event of a vascular occlusion to encourage reperfusion.1,7,8,10,11,13,17,19,26,32 Dayan et al32 reported a series of nine patients whose vascular occlusion was successfully healed with a protocol of hyaluronidase and nitroglycerine paste 2cm applied daily with massage in clinic plus a daily dose of aspirin 325mg with antacid until capillary refill was less than two seconds. Nitroglycerin paste (Rectogesic®, used off label) is applied under an occlusive dressing and used for several days, it was recommend applying for 12 hours and then removing for 12 hours until clinical improvement was seen or until it was no longer tolerated.17 Nitroglycerin can lead to skin reactions, irritation, and erythema, as well as systemic effects including dizziness and hypotension. However, a study by Hwang et al34 failed to show any improvement in outcomes using topical nitroglycerin ointment 2% in induced arterial occlusion in an animal model using rabbit ears. Conversely, it tended to cause a more congested appearance and worsen perfusion by allowing filler material to diffuse from capillaries into larger arterioles, further compromising the circulation. The authors do not recommend the use of topical nitroglycerin for vascular occlusion following soft tissue augmentation.
Follow-up
All patients presenting with a vascular occlusion require follow up until the problem has completely resolved; this might be on a day-by-day basis initially. Immediate follow up is required when a patient contacts the practitioner and a delayed onset of vascular occlusion is suspected. All practitioners carrying out soft tissue augmentation should provide patients with an emergency out of hours number, and if a patient reports symptoms that appear to be consistent with a vascular occlusion, an immediate in-person review should be arranged. It is not acceptable to do this via electronic media. Diligent follow up, ongoing support, and full explanations to the patient is the best approach to prevent a complication from turning into a litigious medical malpractice claim.
References
- Souza Felix Bravo B, Klotz De Almeida Balassiano L, Roos Mariano Da Rocha C, et al. Delayed-type necrosis after soft-tissue augmentation with hyaluronic Acid. J Clin Aesthet Dermatol. 2015;8(12):42–47.
- Oxford Dictionary.
- De Lorenzi, C. New high dose pulsed hyaluronidase protocol for hyaluronic acid filler vascular adverse events. Aesthet Surg J. 2017;37(7):814–825.
- Chang SH. External compression versus intravascular injection: a mechanistic animal model of filler-induced tissue ischemia. Ophthalmic Plast Reconstr Surg. 2016;32(4) 261–266.
- Lima, VGF. External vascular compression by hyaluronic acid filler documented with high-frequency ultrasound. J Cosmet Dermatol. 2019;18(6):1629–1631.
- Ashton MW, Taylor GI, Corlett RJ. The role of anastomotic vessels in controlling tissue viability and defining tissue necrosis with special reference to complications following injection of hyaluronic acid fillers. Plast Reconstr Surg. 2018;141(6):818e–830e.
- Ozturk CN, Li Y, Tung R, et al. Complications following injection of soft-tissue fillers. Aesthet Surg J. 2013;33(6):862–877.
- Narins RS, Jewell M, Rubin M, et al. Clinical conference: management of rare events following dermal fillers–focal necrosis and angry red bumps. Dermatol Surg. 2006;32(3):426–434.
- Maruyama S. A histopathologic diagnosis of vascular occlusion after injection of hyaluronic acid filler: findings of intravascular foreign body and skin necrosis. Aesthet Surg J. 2017;37(9):NP102–NP108.
- Grunebaum L, Allemann I, Dayan S, et al. The risk of alar necrosis associated with dermal filler injection. Dermatol Surg. 2009;35 Suppl 2:1635–1640.
- Tracy L, Ridgway J, Nelson JS, et al. Calcium hydroxylapatite associated soft tissue necrosis: a case report and treatment guideline. J Plast Reconstr Aesthet Surg. 2014;67(4):564–568.
- Graiche, J. Overview of complications of sclerotherapy. Presented at: Australian College of Phlebology, Scientific Meetings and Workshops; September 18–21, 2007; Sydney, Australia.
- Sclafani AP, Fagien S. Treatment of injectable soft tissue filler complications. Dermatol Surg. 2009;35 Suppl 2:1672–1680.
- Urdiales-Gálvez F, Delgado NE, Figueiredo V, et al. Treatment of soft tissue filler complications: expert consensus recommendations. Aesthetic Plast Surg. 2018;42(2):498–510.
- DeLorenzi C. Complications of injectable fillers, part 2: vascular complications. Aesthet Surg J. 2014;34(4):584–600.
- Belezany K, Carruthers JDA. Update on avoiding and treating blindness from fillers: a recent review of the world literature. Aesth Surg Jour. 2019;39(6):662–674.
- Glaich AS, Cohen JL, Goldberg LH. Injection necrosis of the glabella: protocol for prevention and treatment after use of dermal fillers. Dermatol Surg. 2006;32:276–281.
- Nettar K, Maas C. Facial filler and neurotoxin complications. Facial Plast Surg. 2012;28(3):288–293.
- Cohen JL. Understanding, avoiding, and managing dermal filler complications. Dermatol Surg. 2008;34:S92–S99.
- Casabona G. Blood aspiration test for cosmetic fillers to prevent accidental intravascular injection in the face. Dermatol Surg. 2015;41(7):841–847.
- Van Loghem J. Sensitivity of aspiration as a safety test before injection of soft tissue fillers. J Cosmet Dermatol. 2018;17(1):39–46.
- Torbeck, R. In vitro evaluation of preinjection aspiration for hyaluronic fillers as safety checkpoint. Dermatol Surg. 2019;45(7):954–958.
- Hong JY, Seok J, Ahn GR. Impending skin necrosis after dermal filler injection: a “golden time” for first-aid intervention. Dermatol Ther. 2017;30(2).
- Sansone CM, Prendin F, Giordano G, et al. Relationship between capillary refill time at triage and abnormal clinical condition: a prospective study. Open Nurs J. 2017;11:84–90.
- King M, Convery, C, Davies E. This month’s guideline: the use of hyaluronidase in aesthetic Practice (v2.4). J Clin Aesthet Dermatol. 2018;11(6):E61–E68.
- Deok-Woo K, Eul-Sik Y, Yi-Hwa J, et al. Vascular complications of hyaluronic acid fillers and the role of hyaluronidase in management. J Plast Reconstr Aesthet Surg. 2011;64(12):1590–1595.
- Wang M, Li W, Zhang Y, et al. Comparison of intra-arterial and subcutaneous testicular hyaluronidase injection treatments and the vascular complications of hyaluronic acid filler. Dermatol Surg. 2017;43(2):246–254.
- Antithrombotic therapy: a national clinical guideline. SIGN Guideline No. 36. Scottish Intercollegiate Guidelines Network. March 1999.
- Darling MD, Peterson JD, Fabi SG. Impending necrosis after injection of hyaluronic acid and calcium hydroxylapatite fillers: report of 2 cases treated with hyperbaric oxygen therapy. Dermatol Surg. 2014;40(9):1049–1052.
- DeLorenzi C. Complications of injectable fillers, part I. Aesthetic Surg J. 2013;33(4):561–575.
- Schanz S, Schippert W, Ulmer A, et al. Arterial embolization caused by injection of hyaluronic acid (Restylanes). Br J Dermatol. 2002;146: 928–929.
- Kleydman K, Cohen JL, Marmur E. Nitroglycerin: a review of its use in the treatment of vascular occlusion after soft tissue augmentation. Dermatol Surg. 2012;38:1889–1897.
- Dayan S, Arkins JP, Mathison CC. Management of impending necrossis associated with soft tissue filler injections. J Drugs Dermatol. 2011;10:1007–1012.
- Hwang CJ, Morgan PV, Pimentel A, et al. Rethinking the role of nitroglycerin ointment in ischemic vascular filler complications: an animal model with ICG imaging. Ophthalmic Plast Reconstr Surg. 2016;32(2)118–122.

