 J Clin Aesthet Dermatol. 2023;16(7):19–20.
J Clin Aesthet Dermatol. 2023;16(7):19–20.
YouTube as a Source of Information about Seborrheic Dermatitis
Dear Editor:
Seborrheic dermatitis (SD) is a chronic inflammatory eczematous disease characterized by erythematous plaques with greasy scale commonly on the scalp, nasolabial folds, and chest and is accompanied by itch and flaking.1,2 Though common, SD pathogenesis is still poorly understood, and feasible, targeted therapies are lacking, leading to burdensome treatment strategies. Little is known about how patients seek education for chronic dermatologic disease, though studies show most patients with chronic conditions or general skin concerns use the internet as a resource for healthcare guidance.3,4 YouTube, a video-sharing platform, has gained tremendous popularity for communicating medical knowledge, though quality and content of are not routinely evaluated. We hypothesized that SD misinformation was common on YouTube and that most video content was posted by non-healthcare providers (non-HCPs).
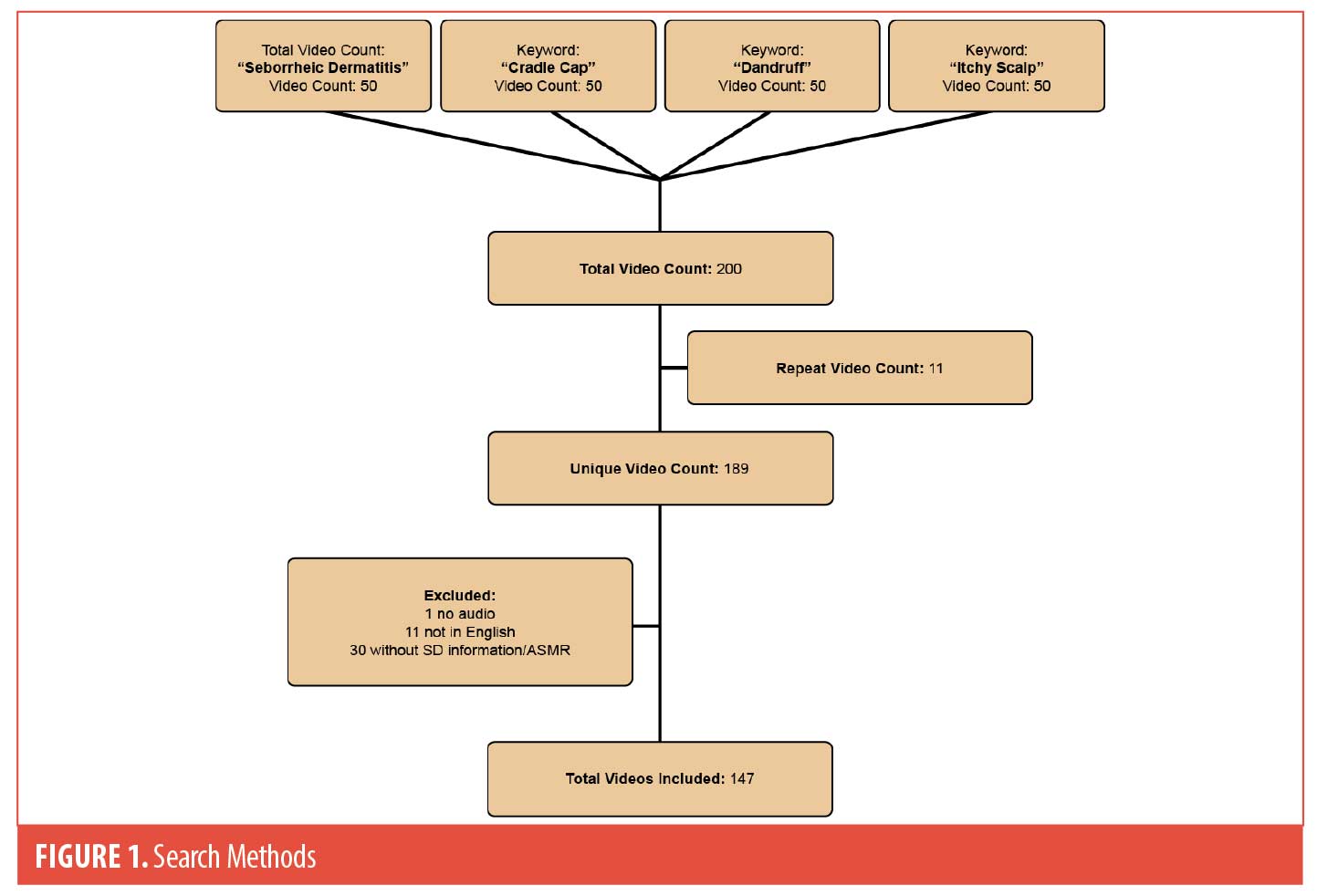
A YouTube search of common terms for SD was performed in August 2022: “seborrheic dermatitis,” “dandruff,” “cradle cap,” and “itchy scalp.” The first 50 videos for each keyword were screened for inclusion, after which the relevancy of video content diminished. Included videos were posted from 2016 to 2022. Videos that were repeated, without audio, not in English, lacking information about SD, or listed as autonomous sensory meridian response (i.e., sensory experience inducing a calming sensation) were excluded. After screening, 147 videos were included for analysis (Figure 1). Videos were characterized by source of information: university/professional organizations, advertisements/for-profit entities, HCPs, and non-HCPs. The number of likes/dislikes, views, and suggested products were also collected. Video content was classified as “useful” (scientifically correct information), “misleading” (inaccurate, scientifically unproven information), and either “useful” or “misleading personal experience” (describing a person’s own experience with SD). Two clinicians (SF, TE) independently reviewed video content with a third reviewer (RC) used in cases of a disagreement.
Of the 147 included videos, 50.0 percent were made by non-HCPs, 30.4 percent by HCPs (60% dermatologist), 11.5 percent by professional organizations, and 6.8 percent advertising companies (Table 1). Nearly half of the videos were either misleading (22%) or had misleading personal experience (24%), while 43 percent were useful and 11 percent contained useful personal experience. Misleading videos were most common amongst advertisements (40%), followed by HCPs (29%), and non-HCPs (20%). Videos created by universities or professional organizations were the most popular with an average of 750,535 views followed by HCPs and non-HCPs with 532,694 and 290,078 views, respectively, with a similar trend for mean number of likes. The most common recommended products included: coconut oil (14.3%), zinc pyrithione (13.6%), ketoconazole (10.2%), selenium sulfide (8.2%), tea tree oil (8.2%), apple cider vinegar (7.5%), coal tar (4.8%), lemon (4.8%), baby/mineral oil (4.8%), salicylic acid (4.1%), topical steroids (3.4%), and ciclopirox (2.0%).
Social media has an significant ability to impact SD patient education, as evidenced by nearly 6 million views across 147 videos in this study. Despite a plethora of content, most SD videos on YouTube were posted by non-HCPs, and nearly half contained incorrect or misleading information. Interestingly, videos posted by HCPs, of which most were dermatologists, had the second highest amount of misinformation, suggesting that misinformation is common across all types of content creators. We hypothesize that this may in part be due to incompletely understood SD pathogenesis, lack of well-designed clinical trials examining commonly used therapies, and limited research and development towards targeted therapies– leading to non-evidence-based treatment recommendations. This contrasts with atopic dermatitis, where most YouTube misinformation was specifically found to come from non-HCPs.5 These findings suggest that accurate, evidence-based educational tools are needed to combat SD misinformation. Additional studies are needed to characterize content that exists across various social media platforms and further understand how patients search for and respond to this information to optimize online content quality and enhance patient outcomes.
With regard,
by Sheiva Fakhraie, BS; Taylor Erickson MD; and Raj Chovatiya MD, PhD
Keywords. Seborrheic dermatitis, social media, education, YouTube
Affiliations. All authors are with the Department of Dermatology at Northwestern University Feinberg School of Medicine in Chicago, Illinois.
Funding. No funding was provided for this article.
Disclosures. Dr. Chovatiya has served as an advisory board member, consultant, and/or investigator for AbbVie, Apogee, Arcutis, Arena, Argenx, ASLAN, Beiersdorf, Boehringer Ingelheim, Bristol Myers Squibb, Cara Therapeutics, Dermavant, Eli Lilly and Company, EPI Health, Incyte, LEO Pharma, L’Oréal, National Eczema Association, Pfizer Inc., Regeneron, Sanofi, and UCB, and speaker for AbbVie, Arcutis, Dermavant, Eli Lilly and Company, EPI Health, Incyte, LEO Pharma, Pfizer Inc., Regeneron, Sanofi, and UCB. All other authors have no dislcosures relevant to the content of this article.
References
- Dall’Oglio F, Nasca MR, Gerbino C, et al. An Overview of the Diagnosis and Management of Seborrheic Dermatitis. Clin Cosmet Investig Dermatol. 2022;15:1537–1548.
- Gupta AK, Bluhm R. Seborrheic dermatitis. Journal of the European Academy of Dermatology and Venereology. 2004;18:13–26.
- Gallo Marin B, Ezemma O, Frech FS, et al. An Analysis of Information Sources of YouTube Videos Pertaining to Tattoo Removal: Cross-Sectional Study. JMIR Dermatol. 2022;5.
- Zanatta ET, Wanderley GPM, Branco IK, et al. Fake news: the impact of the internet on population health. Rev Assoc Med Bras. (1992) 2021;67:926–830.
- Freemyer B, Drozd B, Suarez A. A cross-sectional study of YouTube videos about atopic dermatitis. J Am Acad Dermatol. 2018;78:612–613.

