 by Blake P. Sampson, MD; Aaron M. Secrest, MD, PhD; Christopher B. Hansen, MD; and Alan C. Geller, MPH, RN
by Blake P. Sampson, MD; Aaron M. Secrest, MD, PhD; Christopher B. Hansen, MD; and Alan C. Geller, MPH, RN
Dr. Sampson is with Oregon Health & Sciences University in Portland, Oregon. Drs. Secrest and Hansen are with the Department of Dermatology at the University of Utah in Salt Lake City, Utah. Mr. Geller is with the Harvard T.H. Chan School of Public Health in Boston, Massachusetts.
Funding: No funding was provided for this study.
Disclosures: The authors have no conflicts of interest to relevant to the content of this article.
Abstract: Background. The commercial tanning industry has opposed efforts to educate the public on the risks of tanning as well as attempts to restrict minors’ access to tanning services. Despite a paucity of supporting literature, statements from the tanning industry claiming that dermatologists routinely use in-office phototherapy for cosmetic treatments and refer patients to tanning salons have successfully derailed and defeated legislation in many states.
Objective. This study aims to evaluate dermatologist referrals for ultraviolet radiation for cosmetic and medical purposes via tanning beds or phototherapy, as well as their opinions on tanning, legislation, and ultraviolet radiation counseling practices.
Design. The study was conducted using a 10-question anonymous survey.
Setting. The participants were surveyed during meetings of three regional dermatologic societies.
Participants. One hundred and fifty-two dermatologists attending society meetings participated in the study.
Measures. The authors measured physician referrals, opinions, and recommendations regarding ultraviolet exposure.
Results. Zero physicians (0/152) recommended tanning salons for cosmetic reasons. These 152 dermatologists referred 458 (417 adult, 41 pediatric) out of an estimated 809,369 patients (0.057%) to tanning salons for medical treatment. Of these physicians, 76 out of 152 and 15 out of 152 reported referring at least one adult or one pediatric patient, respectively, within the last year. All respondents supported ultraviolet tanning legislation and discouraged cosmetic tanning.
Conclusion. These findings directly contradict the assertion that dermatologists use ultraviolet radiation for cosmetic purposes or routinely refer patients to tanning salons. This study underscores the complex nature of ultraviolet radiation, as dermatologists infrequently utilize ultraviolet radiation for medical purposes and unanimously support restrictive legislation. In addition, these dermatologists counsel against cosmetic tanning and list tanning bed use among their highest concerns with regard to the health of pediatric patients.
Keywords: Dermatologist referrals, legislation, pediatric dermatology, phototherapy, public health policy, tanning, tanning regimen, tanning salon, tanning bed, ultraviolet radiation, UV, UV counseling practices, UV exposure
J Clin Aesthet Dermatol. 2018;11(2):41–46
Introduction
Ultraviolet (UV) radiation has been strongly associated with both melanoma and non-melanoma skin cancer, as well as a variety of other dermatological conditions.1,2 Despite these dangers, potential benefits exist for photoresponsive skin conditions.3 Specific beneficial UV wavelengths have been filtered into medical phototherapy devices with narrowed emission spectrums and overall UV exposure has been reduced through standardized protocols and treatment localization.4–9 In this article, “phototherapy” refers to in-office, physician-directed UV radiation, while any reference to “tanning” refers to broad-spectrum UV radiation via commercial tanning devices.
There is a growing global public health movement to limit UV radiation as a risk factor for skin cancer. Recently, the medical and public health communities have improved education regarding the harmful effects of UV radiation and championed public policy efforts to restrict UV tanning access to minors. Tanning industry lobbyists, officials, and their affiliated publications have argued that these activities are the result of “the cosmetic dermatology industry attacking indoor tanning for strictly financial gain.”10 They describe dermatologic diseases as “purely cosmetic” and allege that physicians are either dishonest about the dangers of tanning bed use and “violating their Hippocratic oath” by harming patients for cosmetic benefits.10–12 Through social media and industry publications, commercial tanning leaders refute peer-reviewed literature and question the integrity of medical and research institutions.13–15 The industry also provides misleading information to consumers, while simultaneously dismissing the growing body of research substantiating the dangers directly linked to UV exposure.16–26 Referencing a study by Feldman et al27 that reviewed the declining usage of phototherapy in the treatment of psoriasis, the tanning industry claims that “dermatology’s anger for the loss of billions of dollars of phototherapy treatment” is the motivation behind legislation to restrict underage tanning.10 Rather than acknowledge the concurrent advances in the biologic treatment of psoriasis and changes in insurance coverage that have led to increased cost and decreased availability of phototherapy, the tanning industry seeks to equate tanning beds with in-office phototherapy devices, claiming that many patients are treating diseases in commercial tanning beds at the behest of their dermatologists or other physicians.10,11,27,28
This study was designed to clarify physician referrals for exposure to UV light. For physicians referring to tanning salons, we sought the reasons for referral, as well as recommended treatment schedules. Additionally, we gathered physician opinions on tanning, including legislation, non-UV tanning, counseling practices, and pediatric wellbeing.
Methods
A 10-question anonymous survey evaluating physicians referrals by and attitudes toward artificial UV exposure was developed and exempted from International Review Board (IRB) review by the Harvard TH Chan School of Public Health IRB Committee. Data collection was completed from 2012 to 2013, with statistical analysis from 2015 to 2016. Three regional dermatologic organizations participated in the survey: Intermountain Dermatology Society (IDS; members primarily from Idaho, Utah, and neighboring states), Colorado Dermatology Society (CDS, members primarily from Colorado and neighboring states), and Pennsylvania Academy of Dermatology (PAD, members primarily from Pennsylvania and neighboring states). Member dermatologists in attendance at these meetings were offered a paper survey. The surveys were collected in anonymous drop boxes.
The survey queried members on their recommendation of UV tanning devices at a tanning salon and medical phototherapy devices to adults and minors within the past year. Each recommendation was stratified by either cosmetic or medical conditions. The survey included recommendations for non-UV tanning alternatives, opinions on legislation prohibiting minors from using commercial UV tanning, how often UV tanning device usage was included in the social history of patients, which patients receive counseling regarding UV exposure, what counseling is provided, and level of concern for twelve common issues impacting pediatric patients’ wellbeing. (Survey included as Appendix 1)
Univariate significance was tested using the Student’s t-test or the ÷2 test, as appropriate. Statistical significance was considered using a two-sided p<0.05. All analyses were performed using SPSS 22 (IBM, Armonk, New York). Where applicable, standard error was calculated.
The patient population represented in this survey was estimated by multiplying the average number of patients seen per week by 52 weeks, then multiplied by the number of responding providers (average patients per week x 52 weeks x n providers).
Results
Referrals to tanning salons and phototherapy. In this study, zero out of the 152 physicians surveyed recommended tanning salons for cosmetic reasons to any patient, adult or pediatric. Phototherapy was recommended to 0.00025 percent of adult patients (2/809,369) by 1.3 percent of physicians (2/152) for non-medical reasons, and was not recommended to any children for non-medical reasons. Regarding tanning salons, the 152 physicians referred approximately 0.051 percent of adults (417/809,369) and 0.005 percent of pediatric patients (41/809,369) for medical treatment, or about three patients (2.74 adults and 0.27 minors) per provider per year. Fifty percent of the responding physicians (76/152) reported having referred at least one adult within the last year; 9.9 percent (15/152) reported having referred at least one pediatric patient. Regarding phototherapy, an estimated 3,147 (0.389%) adult and 353 (0.044%) pediatric patients were referred for medical treatment, with 83.6 percent (127/152) and 43.4 percent (66/152) respondents referring at least one adult or pediatric patient, respectively, within in the past year.
Specific conditions recommended for UV light treatment included psoriasis, atopic dermatitis, vitiligo, pruritus, cutaneous T-cell lymphoma, lichen planus, pityriasis rosea, graft versus host disease, alopecia, granuloma annulare, contact dermatitis, urticaria, prurigo nodularis, polymorphous light eruption, lipodermatosclerosis, lymphomatoid papulosis, pityriasis lichenoides chronica, folliculitis, actinodermatitis, necrobiosis lipoidica diabeticorum, and tinea versicolor (Table I).
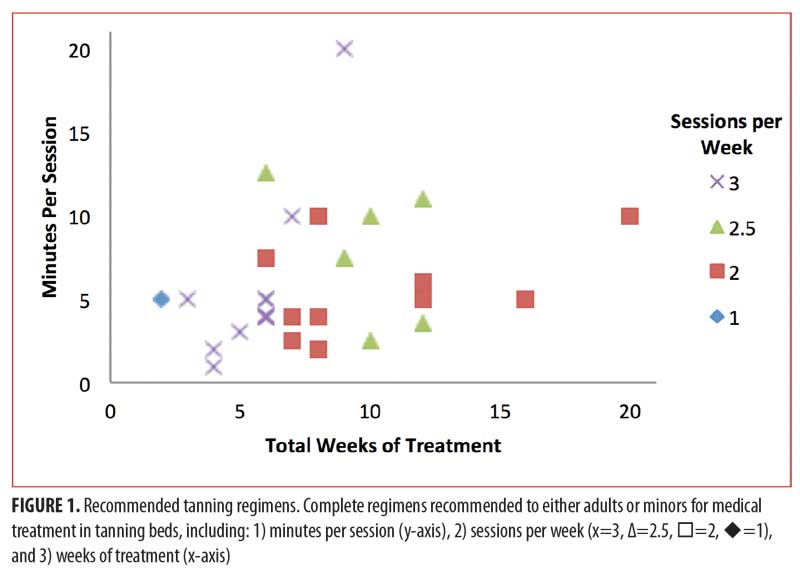
Providers who recommended medical treatment in tanning beds were asked to provide the specific regimens they instruct patients to follow. Of these 76 physicians, 41 percent (31/76) reported a complete regimen with instructions for 1) number of sessions per week, 2) duration of each session, and 3) treatment duration. An additional 20 percent (15/76) reported incomplete regimens. Of the 31 complete regimens reported, 90 percent (28/31) were unique from one another. For physicians referring minor patients to tanning salons for medical treatment, 47 percent (7/15) provided complete regimens and an additional 13 percent (2/15) provided incomplete regimens. Of the seven complete regimens, 86 percent (6/7) were unique from one another (Figure 1).
Non-UV tanning. Of the 152 responders, 89.5 percent (136/152) and 65.1 percent (99/152) reported recommending non-UV tanning methods, such as spray tanning or self-tanners, as alternatives to UV tanning devices to adult and minor patients, respectively, within the last year.
Tanning legislation. Every provider surveyed expressed support for legislation prohibiting minors under age 18 years from using UV tanning devices at commercial tanning salons.
Patient counseling. Providers reported actively discussing the use of UV tanning devices with a variety of patients, including minors and their parents/guardians and patients with skin cancer history. For pediatric patients, female patients received counseling more frequently than male patients (82% vs. 37%, p<0.01). Similar discrepancies were seen by patient sex at all age groups (p<0.01). Female providers were significantly less likely to discuss tanning bed use with male patients of all ages compared to their male provider counterparts (Table 2). When counseling patients, 99.3 percent (150/151) opposed cosmetic tanning (92.7 percent strongly discouraged it and 6.6 percent moderately discouraged the practice).

Concern for pediatric patients’ wellbeing. Physicians rated their level of concern for the wellbeing of pediatric patients related to a variety of health issues using a 1 to 3 scale (1=none, 2=moderate, 3=high) (Figure 2). The highest average levels of concern were for smoking (2.92±0.32), illicit drug use (2.87±0.38), UV tanning (2.77±0.44), texting while driving (2.74±0.54), alcohol (2.68±0.47), and obesity (2.66±0.50).
Practice setting. A trend was noted for increased patient referrals to tanning beds for medical reasons from providers located in rural areas compared to providers located in urban areas (64% vs. 35%, respectively, p=0.06). An inverse trend was noted between rural and urban providers recommending adult phototherapy (62% vs. 82%, respectively, p=0.09). Providers with access to an in-office phototherapy unit were significantly more likely to recommend phototherapy than providers without an in-office unit for both adults (92% vs. 69%, respectively, p<0.001) and minors (57% vs. 26%, respectively, p<0.001). However, physicians were no less likely to recommend tanning beds for medical reasons if they had access to in-office phototherapy (49% vs. 48% for adults and 8% vs. 10% for minors). Having access to in-office phototherapy does not appear to impact whether a dermatologist recommends tanning beds to their patients for medical reasons (49% with access vs. 48% without access for adults and 8% with access vs. 10% without access for minors).
Discussion
As with most medical treatments, UV radiation has both harmful and therapeutic properties. Contrary to tanning industry claims, dermatologic diseases are far from purely cosmetic, and, in some cases, the benefit of UV treatment might outweigh the risk. Psoriasis, for example, has major systemic health implications, including erosive inflammatory arthritis and increased risk of cardiovascular disease, metabolic syndrome, diabetes, and obesity.29–34
While commercial tanning beds and in-office phototherapy units have a similar appearance, they utilize different equipment and emit a vastly different spectrum of UV radiation. For example, narrowband UVB phototherapy devices emit a concentrated dose of 311 to 313nm UVB, while tanning beds emit an average of five-percent broad spectrum UVB (290–320nm) with the remaining 95 percent composed of UVA light (320–400nm). Therefore, tanning beds might be an inefficient source of UV exposure in the treatment of dermatological disease when more ideal options like phototherapy are unavailable due to cost or proximity.35
Interpretation of results. By our estimation, these results represent approximately 809,369 patient visits per year. Only an estimated 0.057 percent, or 458 (417 adult, 41 pediatric) out of the 809,369 patients were referred to tanning salons for medical treatment. We estimate the rates of dermatologist referral to tanning salons for medical treatment to be extremely low; only one adult out of every 1,940 patients and one child out of every 19,450 patients. In other words, the average dermatologist in our study saw 4,000 to 6,500 patients per year and referred approximately three of them (2.74 adults and 0.27 minors) for medical treatment in tanning salons.
Our findings, albeit limited to responses from only 152 physicians, strongly contradict the idea that dermatologists use UV radiation therapy for cosmetic purposes. In our study, none of the 152 physicians who participated in the survey recommended tanning salons for cosmetic reasons to any patient, adult or pediatric. Phototherapy was recommended for cosmetic reasons to two adults, accounting for 0.00025 percent of patients, and zero minors. We suspect the two providers reporting these two patients might have been describing referrals for phototherapy to treat conditions they considered to be cosmetic (e.g., some consider vitiligo treatment to be cosmetic). Additionally, it is important to recognize that the recommendations to use tanning beds for medical reasons were not based on whether the physicians had access to an in-office phototherapy unit. (49% vs. 48% for adults and 8% vs. 10% for minors). This further suggests that referrals by dermatologists are driven by individual patient factors (e.g., insurance coverage, proximity to phototherapy, cost to patient), rather than financial gain.
Recommended treatment regimen. Interestingly, we observed an unexpected level of variability among the treatment regimens recommended to patients for medical treatment in tanning salons. Of the 38 complete treatment regimens, 90 percent of treatments for adults and 86 percent of treatments for minors were unique between providers. Consistent with these findings, there are few published recommendations and no widely accepted standardized treatment protocols for medical use of tanning beds. Future studies to investigate optimal treatment regimens are needed, but the movement toward standardization of dermatologic disease treatment presents several challenges. In addition to physiologic differences between disease conditions, treatment with tanning beds is complicated by individual variability in skin type, dose-response, and exposure history. Perhaps more importantly, inter- and intra-device variability in UV emission, imprecise spectral targeting, and administration by the patient or non-medical staff all have potential to lead to unpredictable variations in dosing.
The composite average of the recommended treatment regimens in this study was 2.5 sessions per week for 6.1 minutes per session for 8.3 weeks. Other publications have suggested 3 to 7 sessions per week starting at a low dose of 2 to 3 minutes per session, with small incremental increases ranging from 15 seconds to one minute per session until the desired effect is achieved, and subsequent clinical follow up 4 to 6 weeks after initiation of treatment.34,36,37 It is suggested that a combination of these techniques in conjunction with patient education to monitor for signs of treatment efficacy (e.g., mild erythema, disease improvement) or overdose (e.g., pain, sunburn, blistering) is the most prudent approach to minimize damage to the skin while optimizing treatment. Additionally, patients should be encouraged to have explicit conversations with tanning salon employees regarding goals (e.g., disease treatment rather than tanning) and methods to minimize dosing variability (e.g., using a specific tanning bed, requesting notification of any bulb or equipment changes).
Limitations. Potential limitations are those inherent to survey studies, including nonresponse bias, sampling bias, and recall bias. Further limitations include the small sample size and regionalized, but limited, distribution of this survey. Due to an inability to discern the specific number of dermatologists who accepted the survey or were in attendance at the surveyed sessions from the total number of registered attendees, which included some non-physician staff and students who were not invited to complete the survey, we were forced to use the entire meeting registry, 350 (IDS=60, CDS=185, PAD=105) in calculating response rate. By assuming all 350 registrants were dermatologists who received the survey, we were able to calculate the minimum possible response rate. However, this method almost certainly resulted in an artificially deflated overall response rate of 43.4 percent. Additionally, time constraints at PAD limited verbal introduction to only the CDS and IDS meetings, where minimum response rates were 52 percent and 53 percent, respectively. We suspect that the brevity and anonymity of the survey, as well as distribution and collection methods, might have limited nonresponse bias despite moderate response rates.
Conclusion
Skin cancer is a rapidly growing and potentially preventable worldwide health concern, and reducing unnecessary UV exposure might prove to be a critical component in reducing the global burden of disease. Our findings underscore the complex nature of UV radiation. While many dermatologists appear to recognize the therapeutic utility of UV radiation, they unanimously support restrictive legislation, counsel against cosmetic tanning, and list tanning bed use among their highest concerns with regard to the health of pediatric patients. Indeed, for some patients experiencing special circumstances (inability to obtain a home-phototherapy unit, limited proximity to office-based phototherapy, difficulty with insurance coverage and/or cost), there might be a role for tanning salons in the treatment of dermatologic disease. However, the acknowledgment of the potential beneficial effects of UV therapy does not mean UV radiation is free of harmful effects; rather it highlights the importance of education, risk-benefit analysis, and the pivotal role clinicians play in the longitudinal management of disease.
References
- Runger TM. ultraviolet light. In: Bolognia J, Jorizzo J, Rapini R, (eds). Dermatology, 3rd ed. Spain: Saunders/Elsevier; 2012:1455–1465.
- Cadet J, Douki T, Ravanat J. Oxidatively generated damage to cellular DNA by UVB and UVA radiation. Photochem Photobiol. 2015;91: 140–155.
- Honigsmann H, Schwarz T. Chapter 134: Ultraviolet Therapy. In: Bolognia J, Jorizzo J, Rapini R, (eds). Dermatology, 3rd ed. Spain: Saunders/Elsevier; 2012;2219–2235.
- Parrish JA, Jaenicke KF. Action spectrum for phototherapy of psoriasis. J Invest Dermatol. 1981;76(5):359–362.
- Lapidoth M, Adatto M, David M. Targeted UVB phototherapy for psoriasis: a preliminary study. Clin Exp Dermatol. 2007;32(6):642–645.
- Levin AA, Aleissa S, Dumont N, et al. A randomized, prospective, sham-controlled study of localized narrow-band UVB phototherapy in the treatment of plaque psoriasis. J Drugs Dermatol. 2014;13(8):922–6.
- Barbagallo J, Spann CT, Tutrone WD, Weinberg JM. Narrowband UVB phototherapy for the treatment of psoriasis: a review and update. 2001;68:345–347.
- Tjioe M, Smits T, van de Kerkhof PC, Gerritsen MJ. The differential effect of broad band vs narrow-band UVB with respect to photodamage and cutaneous inflammation. Exp Dermatol. 2003;12(6):729–733.
- Hearn RM, Kerr AC, Rahim KF, et al. Incidence of skin cancers in 3867 patients treated with narrow-band ultraviolet B phototherapy. Br J Dermatol. 2008;159:931–935.
- International Smart Tan Network site. U.S. derms refer 900,000 to sunbeds: survey. https://smarttan.com/news/index.php/u-s-derms-refer-900000-to-sunbeds-survey-3/. February 23, 2012. Accessed April 26, 2017.
- International Smart Tan Network site. According to Smart Tan an estimated 1.5 million Americans utilize tanning salons to informally treat psoriasis in lieu of phototherapy in a dermatologist’s office. phototherapy procedures use the same equipment found in tanning salons. https://www.facebook.com/SmartTan/posts/10153589333943068. March 4, 2016. Accessed April 26, 2017.
- Russell M. Loudest voice. Smart Tan Magazine. March 2012. 27(3): 23.
- Levy J. [Smart Tan]. Joe Levy on Mayo Study. [Video]. https://www.youtube.com/watch?v=bMRFblOc7Uo&index=46&list=PLD5A114FFE303F663. April 6, 2012. Accessed April 26, 2017.
- International Smart Tan Network site. Derm study more politics than science: Smart Tan News. https://www.facebook.com/SmartTan/posts/112026388839956. May 19, 2010. Accessed April 26, 2017.
- International Smart Tan Network site. Smart Tan Is Right: Dermatologist. http://smarttan.com/news/index.php/smart-tan-is-right/. March 11, 2016. Accessed April 26, 2017.
- S. House of Representatives Committee on Energy and Commerce – Minority Staff. False and misleading health information provided to teens by the indoor tanning industry: investigative report. Carver College of Medicine site. https://www.medicine.uiowa.edu/uploadedFiles/Departments/Dermatology/Content/About_Us/Investigative%20report.pdf. February 1, 2012. Accessed April 26, 2017.
- Levine JA, Sorace M, Spencer J, Siegel DM. The indoor UV tanning industry: a review of skin cancer risk, health benefit claims, and regulation. J Am Acad Dermatol. 2005;53:1038–1044.
- National Toxicology Program. Report on Carcinogens, Thirteenth Edition. Research Triangle Park, NC: U.S. Department of Health and Human Services, Public Health Service. http://ntp.niehs.nih.gov/pubhealth/roc/roc13/. 2014. Accessed April 26, 2017.
- El Ghissassi F, Baan R, Straif K, et al. WHO international agency for research on cancer monograph working group. a review of human carcinogens – part D: radiation. Lancet Oncol. 2009;10(8):751–752.
- Ferrucci LM, Cartmel B, Molinaro AM, et al. Indoor tanning and risk of early-onset basal cell carcinoma. J Am Acad Dermatol. 2012;67:552–562.
- Lazovich D, Vogel RI, Berwick M, et al. Indoor tanning and risk of melanoma: a case-control study in a highly exposed population. Cancer Epidemiol Biomarkers Prev. 2010;19:1557–1568.
- Boniol M, Autier P, Boyle P, Gandini S. Cutaneous melanoma attributable to sunbed use: systematic review and meta-analysis. 2012;345:e4757.
- Ferrucci LM, Vogel, RI, Cartmel B, et al. Indoor tanning in businesses and homes and risk of melanoma and nonmelanoma skin cancer in 2 US case-control studies. J Am Acad Dermatol. 2014;71(5):882–887.
- Wehner MR, Shive ML, Chren MM, et al. Indoor tanning and non-melanoma skin cancer: systematic review and meta-analysis. BMJ. 2012;345:e5909.
- Guy GP Jr., Watson M, Haileyesus T, Annest JL. Indoor tanning-related injuries treated in a national sample of US hospital emergency departments. JAMA Intern Med. 2015;175(2):309–311.
- Wehner MR, Chren MM, Nameth D, et al. International prevalence of indoor tanning: a systematic review and meta-analysis. JAMA Dermatol. 2014;150(4): 390–400.
- Housman TS, Rohrback JM, Fleischer AB, Feldman SR. Phototherapy utilization for psoriasis is declining in the United States. J Am Acad Dermatol. 2002;46(4): 557–559.
- Lim HW, Silpa-archa N, Amadi U, et al. Phototherapy in dermatology: a call for action. J Am Acad Dermatol. 2015;72(6):1078–1080.
- Farley E, Menter A. Psoriasis: comorbidities and associations. G Ital Dermatol Venereol. 2011;146(1): 9–15.
- Onumah N, Kircik LH. Psoriasis and its comorbidities. J Drugs Dermatol. 2012;11(5 Suppl):s5–s10.
- Gelfand JM, Yeung H. Metabolic syndrome in patients with psoriatic disease. J Rheumatol Suppl. 2012;89:24–28.
- Lai YC, Yew YW. Psoriasis as an independent risk factor for cardiovascular disease: an epidemiologic analysis using a national database. J Cutan Med Surg. 2016;20(4):327–333.
- Armstrong EJ, Harskamp CT, Armstrong AW. Psoriasis and major adverse cardiovascular events: a systemic review and meta-analysis of observational studies. J Am Heart Assoc. 2013 Apr; 2(2):e000062.
- Horreau C, Pouplard C, Brenaut E, et al. Cardiovascular morbidity and mortality in psoriasis and psoriatic arthritis: a systematic literature review. J Eur Acad Dermatol Venereol. 2013;27(Suppl 3):12–29.
- Radack KP, Farhangian ME, Anderson KL, Feldman SR. A review of the use of tanning beds as a dermatological treatment. Dermatol Ther. 2015;5:37–51.
- Fleischer AB Jr, Clark AR, Rapp SR, et al. Commercial tanning bed treatment is an effective psoriasis treatment: results from an uncontrolled clinical trial. J Invest Dermatol. 1997;109(2):170–174.
- Carlin CS, Callis KP, Krueger GG. Efficacy of acitretin and commercial tanning bed therapy for psoriasis. Arch Dermatol. 2003;139(4):436–442.

