 J Clin Aesthet Dermatol. 2020;13(7):41–44
J Clin Aesthet Dermatol. 2020;13(7):41–44
by Logan W. Thomas, MD; Christine T. Pham, BS; Brandon Coakley, MD; and Patrick Lee, MD
All authors are with the Department of Dermatology, University of California, Irvine, in Irvine, California.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Patients with Brooke-Spiegler Syndrome (BSS) can present with benign cylindromas, spiradenomas, spiradenocylindromas, and trichoepithelioma. Therapy options include excision, electrocautery, CO2 laser ablation, dermabrasion, and radiofrequency. Here, we present a patient with BSS with multiple trichoepitheliomas who was successfully treated with erbium:yttrium-aluminum-garnet (YAG) laser therapy and review similar cases of BSS treated with a YAG laser modality.
Keywords: Brooke-Spiegler syndrome, trichoepithelioma, erbium:YAG laser
Patients with Brooke-Spiegler Syndrome (BSS) can present with benign cylindromas, spiradenomas, spiradenocylindromas, and trichoepithelioma. Therapy options include excision, electrocautery, CO2 laser ablation, dermabrasion, and radiofrequency. Here, we present a patient with BSS with multiple trichoepitheliomas who was successfully treated with erbium:yttrium-aluminum-garnet (Er:YAG) laser therapy and review similar cases of BSS treated with a YAG laser modality.
Case Report
A 28-year-old female patient presented to the clinic with multiple skin-colored papules on her face that had been present for 15 years prior to visiting the clinic. The patient reported that her mother, maternal uncles, and maternal cousins had similar lesions on their face, scalp, and body.
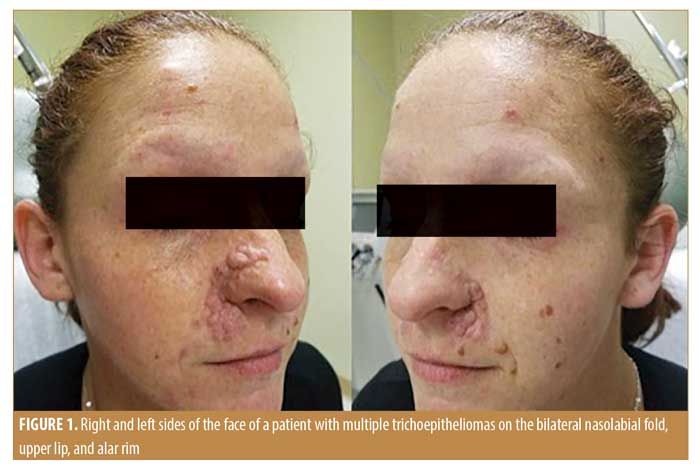
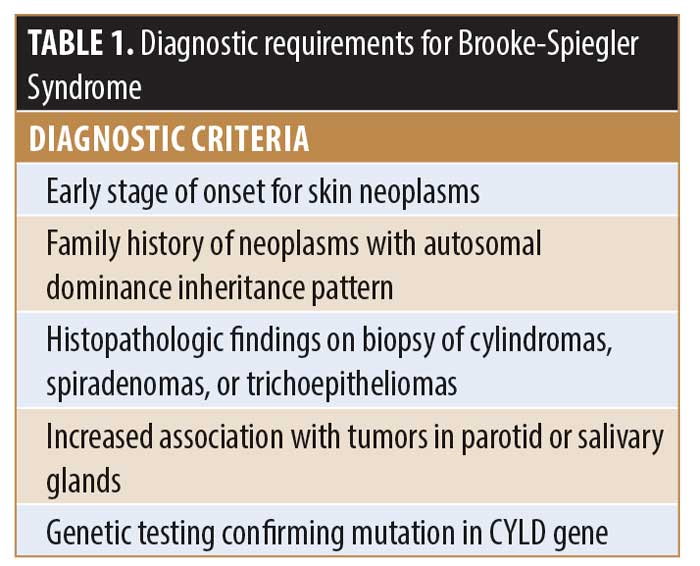
Dermatologic examination showed multiple agminated flesh-colored 2- to 5-mm dome-shaped papules predominantly within the alar grooves, base of the alar rim, and within the nasolabial folds (Figure 1). Two reddish-colored nodules were also identified on the vertex and lateral aspect of the scalp. A deep-seated dermal nodule was additionally noted on the right breast. Three skin biopsies were performed and histopathological examination suggested a cylindroma on the scalp, a spiradenoma on the breast, and a trichoepithelioma on the lip. The combination of diagnostic criteria was necessary to confirm the diagnosis, with genetic testing suggested, though this was not performed in our patient (Table 1). Based on the clinical history, family history, and histopathologic findings, a diagnosis of Brooke-Spiegler syndrome (BSS) was made.
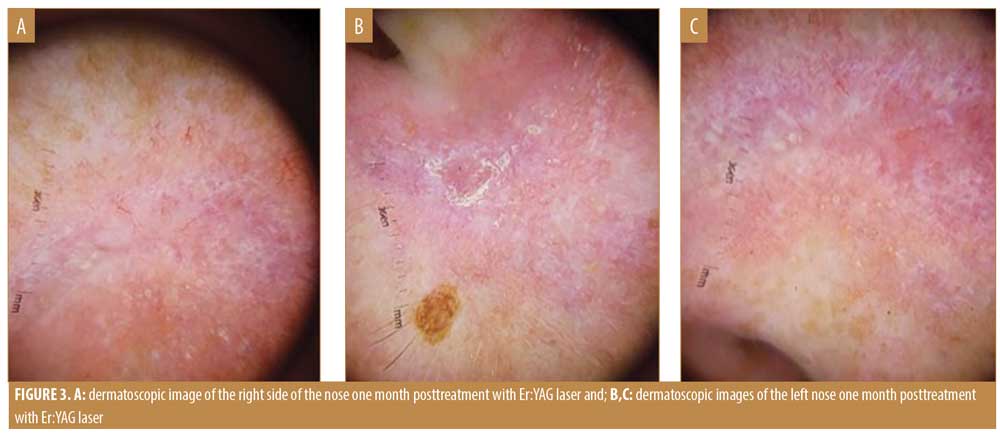
 The patient was recommended to undergo Er:YAG laser therapy using the Sciton profractional laser (Sciton, Palo Alto, California). The treatment area was anesthetized by the combination of a topical anesthetic and nerve blocking with 1% lidocaine and epinephrine. The Er:YAG laser was set at the setting of 50u and an ablation depth at 10 Hz, with suction and no coagulation. The tumors were ablated to the depth of the papillary dermis and no complications were noted aside from expected erythema and tenderness. At both the one- and 31-month follow-up, no recurrence was observed (Figures 2, 3, 4).
The patient was recommended to undergo Er:YAG laser therapy using the Sciton profractional laser (Sciton, Palo Alto, California). The treatment area was anesthetized by the combination of a topical anesthetic and nerve blocking with 1% lidocaine and epinephrine. The Er:YAG laser was set at the setting of 50u and an ablation depth at 10 Hz, with suction and no coagulation. The tumors were ablated to the depth of the papillary dermis and no complications were noted aside from expected erythema and tenderness. At both the one- and 31-month follow-up, no recurrence was observed (Figures 2, 3, 4).

Discussion
BSS is a rare autosomal dominant genetic disorder marked by the development of cutaneous neoplasms, such as cylindroma, spiradenoma, spiradenocylindroma, and trichoepithelioma. The syndrome results from a gene mutation in the cylindromatosis gene (CYLD), located on chromosome 16q12-q13.1 The cutaneous neoplasms are usually benign tumors but, because of the progressive nature of the condition, some reports detail findings of nodules becoming malignant, growing, and developing ulcers and bleeding.2 Volter et al3 observed that malignant transformation is more likely with multiple cylindromas and close follow-up is recommended.3 The condition usually presents itself in young adults and worsens with age. The tumors are normally situated on the scalp, face, and neck area, measuring about 0.5 to 3cm in diameter and varying from a few to several hundred nodules.1
Different treatment modalities have been used to treat BSS, including excision, electrocautery, CO2 laser ablation, dermabrasion, and radiofrequency.4–7 Recurrence of the nodules are common and excessive scarring can occur. In this case, an Er:YAG laser treatment (10 Hz) was adopted with the following settings: 4mm spot size, 5 Joules, and 10 Hz. These settings allowed the laser surgeon to precisely and uniformly remove 250u of tissue per second, which enabled gradual thinning of the target area. The entire procedure took approximately 10 minutes, during which time, the tumors were ablated in a meticulous and controlled manner. The Er:YAG laser was chosen due to research showing successful results with ablation and contour and blend with surrounding tissue.8,9 Also, using an Er:YAG laser facilitates the visualization of hamartomatous tissue while ablating due to a lack of the tissue carbonization normally seen with CO2 lasers. This improved visualization prevents excessive damage and scarring to normal tissue.5,7 The CO2 laser beam is scattered within the cutaneous tissue layer, causing thermal coagulation necrosis not only in the deep tissues directly underneath the laser but also in the surrounding tissues. In contrast, the Er:YAG laser is more precise and does not affect the surrounding tissues like the CO2 laser does. Thermal damage is minimized during the ablation process, leading to the reduction of scarring.
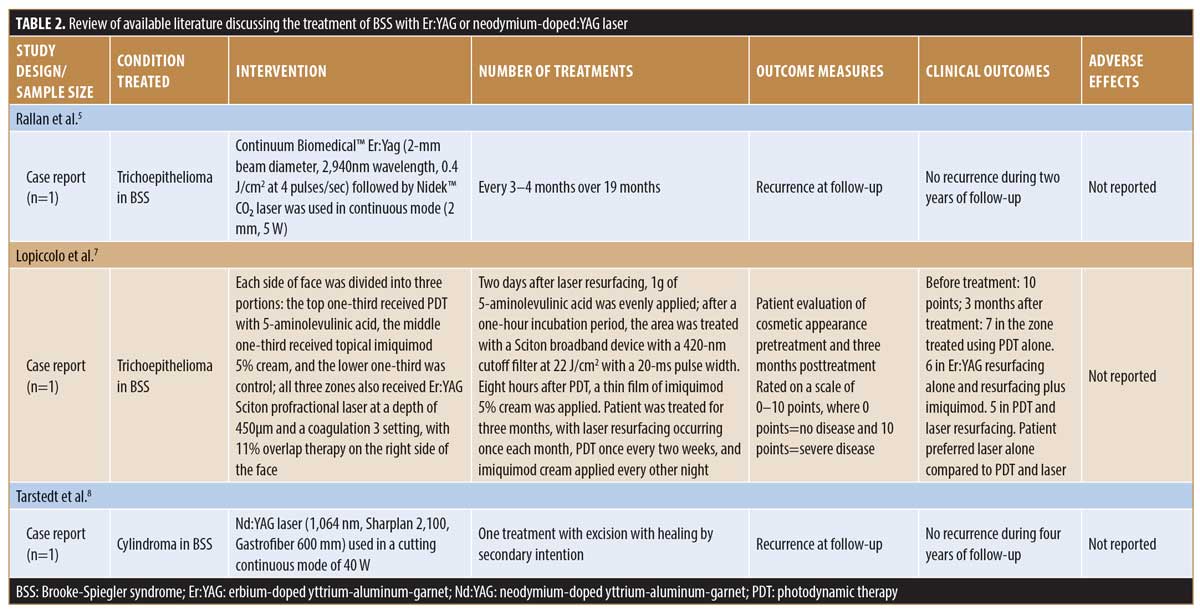
A review of the literature returned three case reports that have used either the Er:YAG laser or neodymium-doped:YAG laser for treatment of either cylindromas and trichoepitheliomas found in BSS (Table 2). One report detailed the successful treatment of trichoepitheliomas on the lip and nasolabial folds with use of an Er:YAG laser (2-mm beam diameter, 2940-nm wavelength, 0.4 J/cm2 at 4 pulses/sec) for ablation, followed by CO2 laser (2mm, 5 W) application for homeostasis, with no recurrence within two years.5 Another case study of one patient compared the efficacy of Er:YAG laser resurfacing, photodynamic therapy (PDT) with 5-aminolevulinic acid, and imiquimod 5% cream in the treatment of multiple trichoblastoma of the face and found that Er:YAG combined with PDT therapy was slightly better than laser therapy alone. Ultimately, however, the patient favored laser therapy alone due to the ease of treatment despite combined PDT and laser therapy showing slightly better results.7 Another report presented the successful treatment of a patient with dermal cylindroma of the scalp with a neodymium-doped:YAG laser. Bleeding was decreased in comparison with when using a CO2 laser due to the neodymium-doped:YAG laser’s ability to seal large blood vessels up to 2mm in diameter by internal heating of the cylindroma. In addition, no relapse occurred after more than four years.10
 The relapse of nodules in BSS is a common occurrence. No relapse occurred during the patient’s one- and 31-month follow-up appointments in this case and the results were deemed to be aesthetically pleasing. However, continuing to monitor patients for a longer period of time is necessary to deduce the effectiveness of Er:YAG laser application in preventing relapse. Furthermore, other treatment modalities should be explored. A case study involving CO2 laser treatment and topical 1% sirolimus cream as suppressive therapy to treat patients with multiple trichoepitheliomas showed limited progression of the disease.7 Another study compared neodymium-doped:YAG, Er:YAG, and CO2 laser treatment and saw significant improvements in skin rejuvenation using the neodymium-doped:YAG laser.11
The relapse of nodules in BSS is a common occurrence. No relapse occurred during the patient’s one- and 31-month follow-up appointments in this case and the results were deemed to be aesthetically pleasing. However, continuing to monitor patients for a longer period of time is necessary to deduce the effectiveness of Er:YAG laser application in preventing relapse. Furthermore, other treatment modalities should be explored. A case study involving CO2 laser treatment and topical 1% sirolimus cream as suppressive therapy to treat patients with multiple trichoepitheliomas showed limited progression of the disease.7 Another study compared neodymium-doped:YAG, Er:YAG, and CO2 laser treatment and saw significant improvements in skin rejuvenation using the neodymium-doped:YAG laser.11
Conclusion
BSS is a rare condition that requires further investigation into proper lesion removal modalities and best results for the prevention of lesion recurrence. This case reports shows the effectiveness of Er:YAG laser therapy alone in the removal of facial trichoepitheliomas.
References
- Kazakov, DV. Brooke-Spiegler Syndrome and phenotypic variants: an update. Head Neck Pathol. 2016;10(2):125–130.
- Kazakov DV, Zelger B, Rutten A, et al. Morphologic diversity of malignant neoplasms arising in preexisting spiradenoma, cylindroma, and spiradenocylindroma based on the study of 24 cases, sporadic or occurring in the setting of Brooke-Spiegler syndrome. Am J Surg Pathol. 2009;33(5):705–719.
- Volter C, Baier G, Schwager K, et al. Cylindroma in a patient with Brooke-Spiegler syndrome. Laryngorhinootologie. 2002;81:243–246.
- Chaudhary S, Dayal S. Radiofrequency ablation: a safe and economical modality in treatment of Brooke-Spiegler syndrome. Dermatol Online J. 2012;18(8):7.
- Rallan D, Harland CC. Brooke-Spiegler Syndrome: treatment with laser ablation. Clin Exp Dermatol. 2005;30(4):355–357.
- Tu JH, Teng JMC. Use of topical sirolimus in the management of multiple familial trichoepitheliomas. Dermatol Ther. 2017;30(2).
- LoPiccolo MC, Sage RJ, Kouba DJ. Comparing ablative fractionated resurfacing, photodynamic therapy, and topical imiquimod in the treatment of trichoblastomas of Brooke-Spiegler Syndrome: a case study. Dermatol Surg. 2011;37(7):1047–1050.
- Pearson IC, Harland CC. Epidermal naevi treated with pulsed erbium:YAG laser. Clin Exp Dermatol. 2004;29(5):494–496.
- Armenores P, James CL, Walker PC, Huilgol SC. Treatment of actinic cheilitis with the Er:YAG laser. JAAD. 2010;63(4):642–646.
- Tarstedt M, Molin L. Nd:YAG laser for effective treatment of multiple cylindroma of the scalp. J Cosmet Laser Ther. 2004;6(1):41–43.
- Alshami MA. New application of the long-pulsed Nd-YAG laser as an ablative resurfacing tool for skin rejuvenation: a 7-year study. J Cosmet Dermatol. 2013;12(3):170–178.

