 J Clin Aesthet Dermatol. 2021;14(1):34–37.
J Clin Aesthet Dermatol. 2021;14(1):34–37.
by Sumir Kumar, MD; Amandeep Kaur, PG Resident; and Sukhmani Kaur, MD
Drs. Kumar and A. Kaur are with the Department of Dermatology, Leprology and Venereology at Guru Gobind Singh Medical College in Faridkot, Punjab, India. Dr. S. Kaur is with Fortis Clinic, in Chandigarh, India.
FUNDING: No funding was provided for this article.
DISCLOSURES: The authors report no conflicts of interest relevant to the content of this article.
ABSTRACT: Dermatophytosis is one of the most common diseases worldwide and is difficult to treat due to its recalcitrant nature. Conventional treatment modalities are associated with frequent relapses due to the absence of a host immune interaction. Here, we present a case series of three patients with difficult-to-treat and recalcitrant dermatophytosis who were treated with homologous autoimplantation. Complete clearance of dermatophytosis was observed after three months in two of the patients and after two and a half months in one patient without the use of any antifungals. No relapses were observed within six months of follow-up. The outcomes of the three patients presented in this case series support homologous autoimplantation as a safe and effective procedure for the treatment of recalcitrant dermatophytosis. The procedure requires only a single visit that can be performed either alone or in combination with other modalities.
KEYWORDS: Autoimplantation, dermatophytosis, immunotherapy, recalcitrant, relapse, resistant, tinea
Dermatophytosis is a superficial fungal infection of keratinized tissue of the skin. Dermatophytes, which are keratophilic organisms that have the ability to invade hair, nails, and the skin, total 39 species that are closely related to one another across the following three genera: Microsporum, Trichophyton, and Epidermophyton.1 These organisms metabolize keratin and trigger a range of pathologic clinical presentations, including tinea corporis, tinea cruris, and tinea faciale.2 The lesions may become widespread and may have significant negative social, economic, psychological, and occupational health effects and can affect the quality of life significantly.3 High humidity, overcrowding, and poor hygienic conditions are predisposing factors for dermatophytosis, making it a major public health concern in many countries.4
Dermatophytosis is one of the most common skin diseases worldwide, especially in developing countries like India.5 Recently reported prevalence rates of dermatophytosis in India range from 36.6% to 78.4%.6 Various antifungal agents (e.g., itraconazole, terbinafine, and fluconazole) used in conventional regimens appear to have lost their relevance in the current clinical scenario.7 There is a rising trend of patients experiencing relapse following the cessation of antifungal therapy, which has not been conclusively proven to be consequent to drug resistance.5 Possibly, there may be other factors that play a role, including the host immune response and impaired barrier functioning of the epidermis. The use of corticosteroids in fixed-dose combinations (FDCs) with antifungals and their misuse may also account for such relapses.
Healthy individuals have adequate immunity against fungal infections, but such infections are increasing very rapidly8,9 and cell-mediated immunity appears to be of particular importance in this context.
Homologous autoimplantation is a simple technique that works by inducing cell-mediated immune response against the antigens essential for the clearance of dermatophytes. It has already provoked a good clinical response in patients with verruca vulgaris in various clinical studies.12,13 Here, we present a case series of three patients with difficult-to-treat and recalcitrant dermatophytosis who were treated with homologous autoimplantation.
Methods
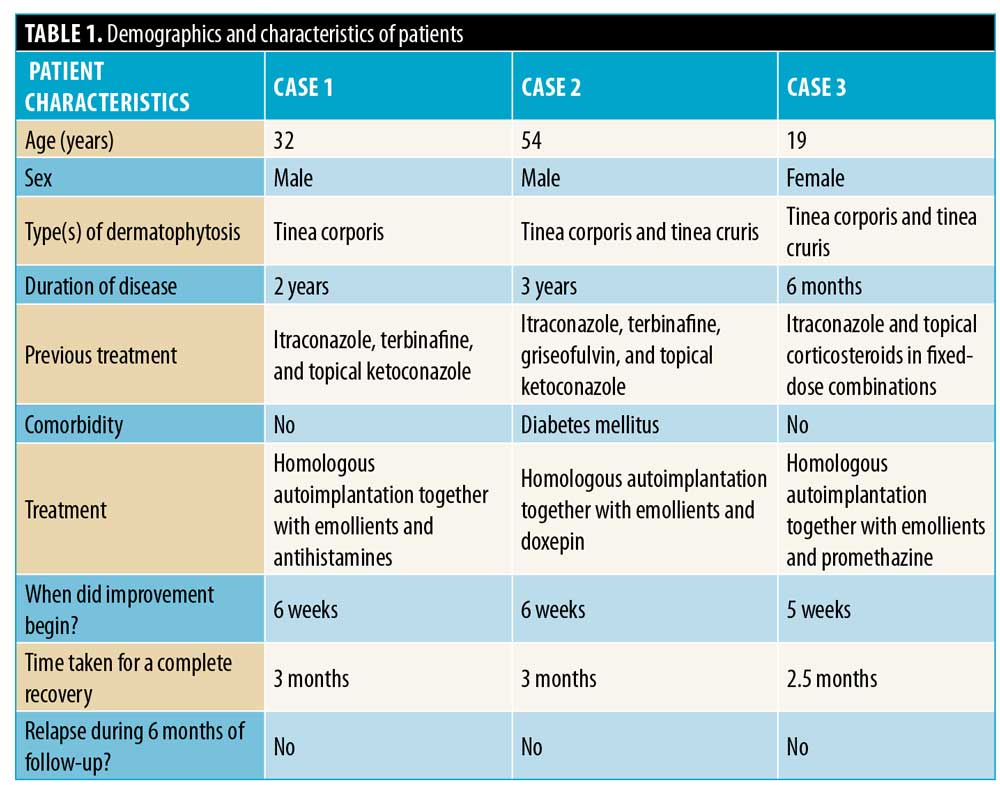
Homologous autoimplantation therapy is an easy, minimally invasive, single-sitting procedure. Informed written consent was collected from all patients before the procedure. Demographics and characteristics of the three patients described here are summarized in Table 1.
Procedure. Donor tissue for autografting was harvested by superficially paring the tinea lesion. The lesion to be pared was first cleaned with povidone iodine to achieve asepsis. Paring was done using a NO. 11 sterile surgical blade and a elevated margin of the tinea lesion of 5mm in size was established. Hemostasis was achieved by applying pressure over the donor area. Pared tissue was transferred on a sterile surgical swab. The donor tissue was then cut into multiple small pieces by supporting on a sterile glass slide. Autografting was done on the right upper anteromedial thigh. The site of engraftment was cleaned with povidone iodine and filled with 0.5 mL of lignocaine with adrenaline. A subcutis deep stab incision of 3mm was created using a different NO. 11 surgical blade in accordance with the resting skin tension lines. Using a backwards and forwards motion with an 18-gauge needle, a subcutaneous pocket was created. The small chunks of pared tissue were cleaned with normal saline and gently introduced deep into the subcutis using the same 18-gauge needle. The margins of the wound were approximated with pressure and closed with an adhesive bandage. The patients were advised not to wet or remove the plaster for five days.
Case Series
Case 1. A 32-year-old man with extensive tinea corporis persisting for two years presented to the clinic after having failed to clear the infection using other treatment modalities, including itraconazole, terbinafine, and topical ketoconazole. Three months prior to presenting to our clinic, the patient had ceased using all treatment modalities. His diagnosis was confirmed by potassium hydroxide mounting. The baseline hematological investigations were within the normal limits. Homologous autoimplantation was performed and emollients and antihistamines were prescribed to reduce itching. A significant improvement was seen after six weeks in the form of decreased erythema and itching; thereafter, complete clearance was observed after three months. The patient was followed up with for six months and no relapse was observed (Figure 1)

Case 2. A 54-year-old man with a three-year history of extensive tinea corporis and tinea cruris presented to the clinic. Diagnosis was confirmed by potassium hydroxide mounting. The patient had taken itraconazole for three months, terbinafine for two weeks, and griseofulvin for one month at different intervals together with topical antifungals (e.g., ketoconazole), with frequent relapses. He also had diabetes mellitus. The results of other baseline hematological investigations were normal. Homologous autoimplantation was completed and emollients and doxepin 25mg were prescribed to reduce itching. Improvement was first observed at six weeks and complete recovery was seen within three months. No relapse had occurred at six months of follow-up (Figure 2).

Case 3. A 19-year-old woman presented with a six-month history of extensive tinea corporis and tinea cruris. Microscopic examination showed fungal hyphae. A history of the use of topical corticosteroids in fixed-dose combinations was noted. She had also taken itraconazole for 2.5 months, with minimal relief, then stopped the medicine and reported new lesions after one month. Her baseline hematological investigations were normal. Homologous autoimplantation was performed and emollients and tablet promethazine 25mg were prescribed to reduce itching. Improvement was seen at five weeks and complete clearance was seen at 2.5 months. No relapse was recorded during six months of follow-up (Figure 3).

Discussion
Dermatophytosis has persisted among the common infective dermatoses reported in tropical countries due to their high levels of humidity and moist environments. This infection is apparently resilient, having the tendency to reoccur frequently, and the overall number of patients presenting with recalcitrant dermatophytosis is rising drastically.7
Recalcitrant dermatophytosis refers to the relapse, recurrence, reinfection, persistence, and possibly microbiological resistance of dermatophytosis.10
Factors implicated in recalcitrant dermatophytosis include the following5:
- Host-fungal immune response (Th1/17 being protective and Th2 causing chronicity of infection)
- Virulence potential of the infecting strain or species
- Clinical type of dermatophytosis
- Barrier defects
- Local factors (e.g., heat, humidity, sweating, and type of clothing)
- Pharmacological factors (e.g., quality of the drug, patient adherence to treatment, pharmacokinetics, and absorption of the drug)
- Reinfection from other sources
In developing countries like India, other factors, including poverty, inaccessibility to dermatologists, availability of over-the-counter topical corticosteroids, overcrowding of housing, humans co-habitating with domestic animals, and the introduction of tight clothing appear to have contributed to widespread or extensive cases of this condition.4 As mentioned earlier, the standard recommendations taken from current guidelines are no longer relevant in the modern Indian context.7
In one study, Sardana et al5 concluded that in-vitro resistance to antifungals is not common and should not be frequently labeled as a cause of treatment failure. Instead, the problem lies in the intricate host-fungus interaction. The viability of the immune system and cell-mediated immunity appear to be particularly important. The mechanisms involved in generating immunologic reactions in the skin are complex, with epidermal Langerhans cells, other dendritic cells, lymphocytes, microvascular endothelial cells, and the keratinocytes themselves all participating in one way or another.11
Dermatophytes usually invade the outer layers of skin (i.e., remaining restricted to the stratum corneum) and do not invade living tissue. Homologous autoimplantation leads to the immune system being exposed to dermatophyte strains, allowing it to mount a delayed type of hypersensitivity response to dermatophyte antigens with the production of Th1 cytokines (e.g., inteleukin-2, -4, -5, and -8; interferon-gamma; and tumor necrosis factor alpga) and causing activation of natural killer and cytotoxic cells. This cytokine profile is altered towards a Th1-predominant type, decreasing the Th2 response and inducing strong cell-mediated immunity. Since the response is systemic, dermatophytosis at all sites shows a response.12,13 Given reports of successive treatment of difficult-to-treat warts13 and extensive molluscum contagiosum14 with homologous autoimplantation, this approach may be viable for the treatment of extensive and recalcitrant dermatophytosis.
There is an expected time lag of a minimum of 4 to 6 weeks between the procedure and the response and the patient may complain of itching during this period, which can be easily managed with antihistamines. Once immunity is generated against the dermatophyte infection, recurrence of that specific type is not commonly observed.
Conclusion
Presently, the treatment of dermatophytosis is difficult due to the development of resistance to available modalities and the failure of the immune system to detect dermatophyte antigens. Immunotherapy by stimulating an immune response has shown good results with reduced chances of recurrence. Homologous autoimplantation appears to be a safe and effective single-sitting procedure, which can be used either alone or in combination with other modalities for the treatment of recalcitrant dermatophytosis. Randomized, controlled studies with larger sample sizes and longer follow-up periods are required to confirm the results observed in our case series.
References
- Liu D, Coloe S, Baird R, Pedersen J. Application of PCR to the identification of dermatophyte fungi. J Med Microbiol.`2000;49(6):493–497.
- Sahoo AK, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis: a comprehensive review. Indian Dermatol Online J. 2016;7(2):77–86.
- Jerajani H, Janaki C, Kumar S, Phiske M. Comparative assessment of the efficacy and safety of sertaconazole (2%) cream versus terbinafine cream (1%) versus luliconazole (1%) cream in patients with dermatophytoses: a pilot study. Indian J Dermatol. 2013;58(1):34–38.
- Ranganathan S, Menon T, Selvi SG, Kamalam A. Effect of socioeconomic status on the prevalence of dermatophytosis in Madras. Indian J Dermatol Venereol Leprol. 1995;61(1):16–18.
- Sardana K, Kaur R, Arora P, et al. Is antifungal resistance a cause for treatment failure in dermatophytosis: A study focused on tinea corporis and cruris from a tertiary centre?. Indian Dermatol Online J. 2018;9(2):90–95.
- Naglot A, Shrimali DD, Nath BK, et al. Recent trends of Dermatophytosis in Northeast India (Assam) and interpretation with published studies. Int J Curr Microbiol App Sci. 2015;4(11):111–120.
- Verma S, Madhu R. The great Indian epidemic of superficial dermatophytosis: an appraisal. Indian J Dermatol. 2017;62(3):227–236.
- Ajello L. Present day concepts in the dermatophytes. Mycopatho Myco Appl. 1962;17:315–339.
- Havlicava B. Epidemiological trends in skin mycoses worldwide. Mycoses. 2008;51 Suppl 4:2–15.
- Mahajan K, Sharma S, Sardana K, Gupta A. Superficial fungal infections. In: Sardana K, Mahajan K, Mrig PA, editors. Fungal infections: Diagnosis and treatment. 1st ed. New Delhi: CBS; 2017; 52–178.
- Rajagopalan M, Inamadar A, Mittal A, et al. Expert consensus on the management of dermatophytosis in india (ECTODERM India). BMC Dermatol. 2018;18(1):6
- Shivakumar V, Okade R, Rajkumar V. Autoimplantation therapy for multiple warts. Indian J Dermatol Venereol Leprol. 2009;75(65):593–595.
- Swaroop MR, Sathyanarayana BD, Vasudevan P, et al. Evaluation of efficacy and safety of modified technique of auto wart implantation in the treatment of multiple, recurrent and recalcitrant warts. Indian J Clin Exp Dermatol. 2016;2(2):27–31.
- Gupta K, Bareth A, Agarwal N. Autoimplantation therapy for the management of extensive molluscum contagiosum: a novel treatment approach. Inj J Res Med Sci. 2016;4(5):1392–1396.

