 J Clin Aesthet Dermatol. 2018;11(8):35–40
J Clin Aesthet Dermatol. 2018;11(8):35–40
by Niamh Corduff, MBBS, FRACS
Dr. Corduff is with the Cosmetic Refinement Clinic in Geelong, Australia.
Funding: This article was funded by Merz Asia Pacific.
Disclosures: Niamh Corduff is a consultant for MERZ Asia Pacific and Australia.
Abstract: Soft tissue filler augmentation for beautification is a common aesthetic request from women who wish to enhance facial features. These interventions are performed in both younger and older women and can result in exaggerated or over-augmented lips and cheeks. This unsatisfactory outcome in older women might be due to the inappropriate application of filler enhancement principles that are based the characteristics of a young face. These existing principles do not necessarily translate well to an older face due to underlying facial skeletal changes associated with aging. Mature women might prefer subtler corrections that do not significantly alter their faces, but rather refresh and revitalize their current appearance. Here, the author presents a 12-point revitalization guide, based on personal experience, as an approach for the pan-facial application of calcium hydroxylapatite and hyaluronic acid fillers specific to the aging female face that can result in an understated and age-appropriate appearance. Three illustrative cases are also presented.
Keywords: Revitalization, 3D, soft tissue fillers, facial augmentation, aging female face
Contemporary aesthetic medicine has undergone paradigm shifts over the last few years in terms of patient requests and social trends. Beauty standards are now based on individuals in their twenties.2–4 These standards of beauty include full lips, high cheeks, and softer, more oval facial shapes, which are often glamorized or sexualized.5 Specific aesthetic interventions applied to aging women according to these standards of beauty can produce outcomes that are incongruous with the aging face and body. Exaggerated cheek and lip enhancements that look pleasing on a young face can create conspicuous discrepancies in the older patient when the underlying aging skeletal framework and facial soft tissue changes are not addressed. While these cosmetic results might be fashionable in some circles and in the media, most older female patients will likely want to avoid the potential social stigma associated with undergoing obvious cosmetic procedures, and thus might seek more subtle improvements in their appearance that focus on health, vitality, and well-being, not youth. To achieve a more satisfactory outcome for this group of patients, a different approach is needed when applying injectable facial fillers—one that is harmonious with, beneficial to, and respectful of a patient’s age and lifestyle.
As a consequence of aging, the soft, oval facial shape associated with feminimity can become boxy, stern, or tired looking, and/or more masculine in appearance. This is due to bone loss primarily within the mandible and maxilla, associated ligament laxity, and loss of fat.6,7 This article, based on the author’s personal experience, describes a 12-point revitalization guide to filler use that addresses these underlying three-dimensional (3D) structural facial changes in older women. This guide can be used to restore an understated softness to the aging female face that is simultaneously age-appropriate and in harmony with the rest of the face, neck, and body. These recommendations can be individualized according to patient needs. Three illustrative cases are presented.
Methods
The guide presented in this article is viewable online in a video (https://merz.wistia.com/medias/zh5j6h2802).
 Cases. Treatment of the following three female patients (Patient 1, age 54 years; Patient 2, age 42 years; Patient 3, age 36 years) with aging-related facial characteristics are presented. The two younger patients exhibited early signs of facial aging. None of the patients had received fillers in the prior 12 months or botulinum toxin A in the prior six months. The patients had no contraindications to filler injections and consented to needlestick protocols and injections of hyaluronic acid (HA; Belotero®; Merz Aesthetics GmbH, Frankfurt, Germany) and calcium hydroxylapatite (CaHA; Radiesse®; Merz Aesthetics GmbH, Frankfurt, Germany). Full informed consent of injection procedure, including potential complications, and photoconsent were received from all three patients.
Cases. Treatment of the following three female patients (Patient 1, age 54 years; Patient 2, age 42 years; Patient 3, age 36 years) with aging-related facial characteristics are presented. The two younger patients exhibited early signs of facial aging. None of the patients had received fillers in the prior 12 months or botulinum toxin A in the prior six months. The patients had no contraindications to filler injections and consented to needlestick protocols and injections of hyaluronic acid (HA; Belotero®; Merz Aesthetics GmbH, Frankfurt, Germany) and calcium hydroxylapatite (CaHA; Radiesse®; Merz Aesthetics GmbH, Frankfurt, Germany). Full informed consent of injection procedure, including potential complications, and photoconsent were received from all three patients.
Preparation. Faces were cleaned with Cetaphil® (Galderma Laboratories, USA) and 0.5%-chlorhexidine. Lignocaine 1% was injected at cannula entry points. Emla™ cream (AstraZeneca, Australia) was applied to the areas in which multiple injections were planned (Figures 1A and 2A), such as the lips, nasolabial folds (NLF), and marionette lines. Standardized photos were taken pre- and post-injection at baseline, two weeks, and four months post-procedure.
Procedure. Patients sat upright for injections into all gravity-dependent areas and were supine for injections to gravity-independent areas (e.g., lips and temples). For CaHA injections, 1.5mL was reconstituted with 0.3mL of lignocaine 1% per site. For HA injections, products with different rheological characteristics were used. One HA product had high elasticity, viscosity, and cohesivity (Belotero® Intense, abbreviated to HA-EVC), another had high G-prime and plasticity (Belotero® Volume, abbreviated to HA-GP), and a third had low viscosity and high cohesivity (Belotero® Balance; abbreviated to HA-VC). The first six injection points addressed the three-dimensional framework of the face (Figure 1A).
Jawline. A jowl entry-point was created using a 21G needle (Figure 1B), and a 22G cannula was advanced subdermally, inserted just below the lower mandible border toward the mandibular angle. Starting behind the mandibular angle, 0.05 to 0.1mL CaHA deposits (’threads’) were then delivered by retrograde injections and placed underneath the mandible border. This ensured that the width of the lower face mandibular was not increased (Figure 1C and D).
The thread of filler was tapered off in a teardrop shape before reaching the jowl. Up to six CaHA threads (total 0.7–1mL) were then delivered here. To treat the anterior mandible, the cannula was advanced anteriorly through the superficial subdermal plane toward the submentum, the anterior limit being in line with the alar base. Three teardrop-shaped CaHA threads (0.3mL–0.5mL) were deposited in a retrograde manner beneath the mandibular ramus, with more being deposited at the pre-jowl sulcus. Following mental nerve blocking, a submental midline entry point was created (Figure 1D). A 22G cannula was advanced from deep to superficial beyond the mental crease up to the vermillion border in the plane between the orbicularis oris muscle and dermis. Four to 6 CaHA threads (0.3–0.5mL) were deposited in a retrograde fan pattern passing across the mental crease.
Preauricular area. An entry point was created above the mandibular angle at the center of the masseter (Figure 1E). Six CaHA threads (0.5–1mL total) were deposited subdermally by retrograde linear threading and fanning from the preauricular area over the zygomatic arch to the anterior region, in line with the lateral orbital rim.
Frontal bone. A lateral forehead anterior temporal crest entry point was created using a 23G needle (Figure 1F). HA-VC 0.5 to 1mL (per side) was deposited beneath the frontalis muscle using a 25G cannula and transverse retrograde linear threads. On patients with thicker skin, HA-GP was used due to its plasticity and greater lifting capacity. A further entry point in the upper central forehead (Figure 1G) was used to deposit retrograde threads of HA-VC, down to the glabella. Although accessible, physicians should be aware that this is a high-risk area for vascular embolisms. Thus, very slow, low-pressure, retrograde injections using a 22G cannula and careful placement on the periosteum are advised. Exerting pressure over the supratrochlear and supraorbital foramina with a finger while injecting might also reduce embolic flow.
Temple. A 25G cannula was advanced through a zygomatic arch entry point and guided between the superficial temporoparietal fascia and deep temporal fascia (Figure 1H). HA-VC 0.5 to 1mL (per side) was distributed using retrograde linear threads while carefully avoiding the superficial temporal artery and superficial veins passing deeply below them. This superficial approach improves pantemporal contouring. Shallower and anterior temporal hollowing was treated with HA-GP delivered supraperiosteally via a 27G needle (Figure 1I).
Midface. From an entry-point over the body of the zygoma (Figure 1J), a 22G cannula was advanced medially, deep to the orbicularis oculi muscle (OOM) to the area of infraorbital hollowing at the junction of the palpebromalar and nasojugal grooves. HA-GP 0.5 to 1mL per side was deposited.
Ristow’s space. To lift the alar, soften the nasolabial fold, and shorten and lift the upper lip, a 22G cannula was advanced medially from the same puncture site over the body of the zygoma to just under the alar base (Figure 1K). The tough transverse maxillary ligament can be felt just lateral to the alar base. A 0.5 to 1mL bolus of HA-EVC or CaHA was injected deep into the periosteum.
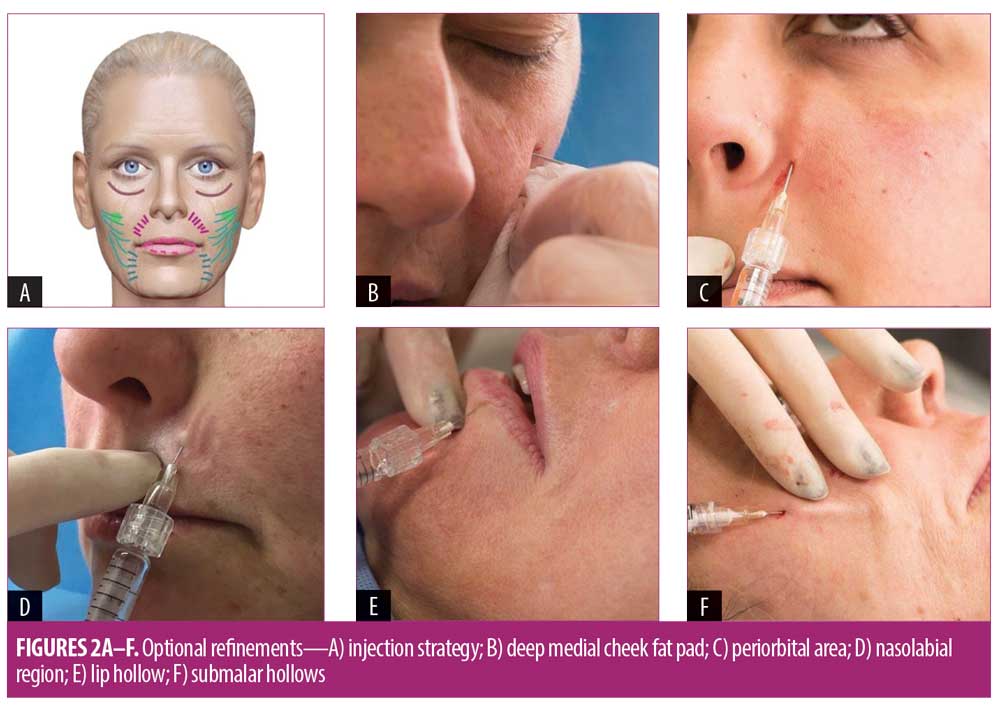
Optional refinements. After three months, additional injections were performed to the following six areas, if required: cheek, peri-orbital/tear trough, nasolabial grooves, marionette lines, lips, aubmalar hollows and and lower face volume loss (Figure 2A). Following the completion of the initial framework injections, less filler volume was used in these secondary areas.
Cheek (Figure 2B). Using a 27G needle, 0.25 to 0.5mL boluses of HA-GP was injected into the deep medial cheek fat compartment of Patients 1 and 3, lateral to the infraorbital foramen, deep in the supraperiosteal plane. It was also injected more laterally onto the zygoma to smooth contours. The patients were seated upright during treatment to facilitate superocranial viewing (i.e., looking down from above the patient) for volume correction.
Periorbit/tear trough (Figure 2C). Correction to this area was performed in Patients 2 and 3 by injecting HA-EVC (0.25mL per side) using a 25G cannula directed upward from the nasolabial fold passing deep to the orbicularis oculi until the cannula tip abutted the orbicularis-retaining ligament where it originates from just below the orbital rim. Drops of filler were injected to support the ligament. Threads of HA-VC (0.25mL per side) were also injected by advancing a 27G cannula supraperiosteally into the palpebromalar groove.
Nasolabial grooves (Figure 2D). Using a 30G needle, transverse intradermal threads of HA-EVC (0.25–0.5mL per crease), which has a high elasticity and tissue integration capacity, were injected across nasolabial grooves of Patients 1 and 2. Filler was dispensed in an anterograde manner at the deep intradermal level from entry-points situated inferomedially and perpendicularly to the grooves.
Marionette lines (Figure 2D). Transverse intradermal threads of HA-EVC, as described for nasolabial grooves, were also injected in the marionette lines of Patients 1 and 2.
Lips (Figure 2E). Lips with ideal shape (Patient 1) were subtly volumized using HA-VC. Aged lips requiring more shaping (Patient 2) received high-elasticity HA-EVC. A 31G needle was inserted at four points just outside the vermillion border and directed anteriorly to the level of the wet-dry junction (Figure 2F). Filler was deposited anteriorly in the superficial muscle in multiple fanned drops of 0.02 to 0.03mL. One-quarter of this filler volume was deposited in the commissures. A total of 0.5 to 1mL was used.
Submalar hollows and lower face volume loss (Figure 2F). These were subcutaneously treated in Patient 1 with a subdermal wash of hyperdiluted CaHA (1:1 dilution) to stimulate neocollagenesis and improve skin quality.8 CaHA (1.5mL per face side) was injected through a 25G cannula advanced subdermally in areas with volume loss or requiring skin matrix structural support. Subdermal placement can indirectly cause mechanical stretching that produces a biostimulatory effect (neocollagenesis).9
Assessment
At two-weeks and four-months post-treatment follow-up visits, patients were assessed, using the Global Aesthetic Improvement Scale (GAIS), for clinical effectiveness by the investigator, the patients themselves, and a blinded independent rater. The GAIS is a five-point scale that grades global improvements in appearance compared to baseline.10 Improvements were scored as worse= –1, no change=0, improved=1, much improved= 2, and very much improved= 3. Each treatment area was scored at baseline and during each follow-up appointment, with results compared to baseline. All outcomes were assessed via photographs taken at two weeks and four months post-treatment. The investigator, blinded evaluator and patients performed these assesments.Effectiveness endpoints were improvements in GAIS scores at two weeks and four months from baseline. All adverse events were recorded.
Results
All three patients presented with reduced jaw height and chin projection, hollowing of preauricular and temple areas, scalloping of the frontal bone, and moderate volume loss in the midface (Figure 3A, 3C, 3E).
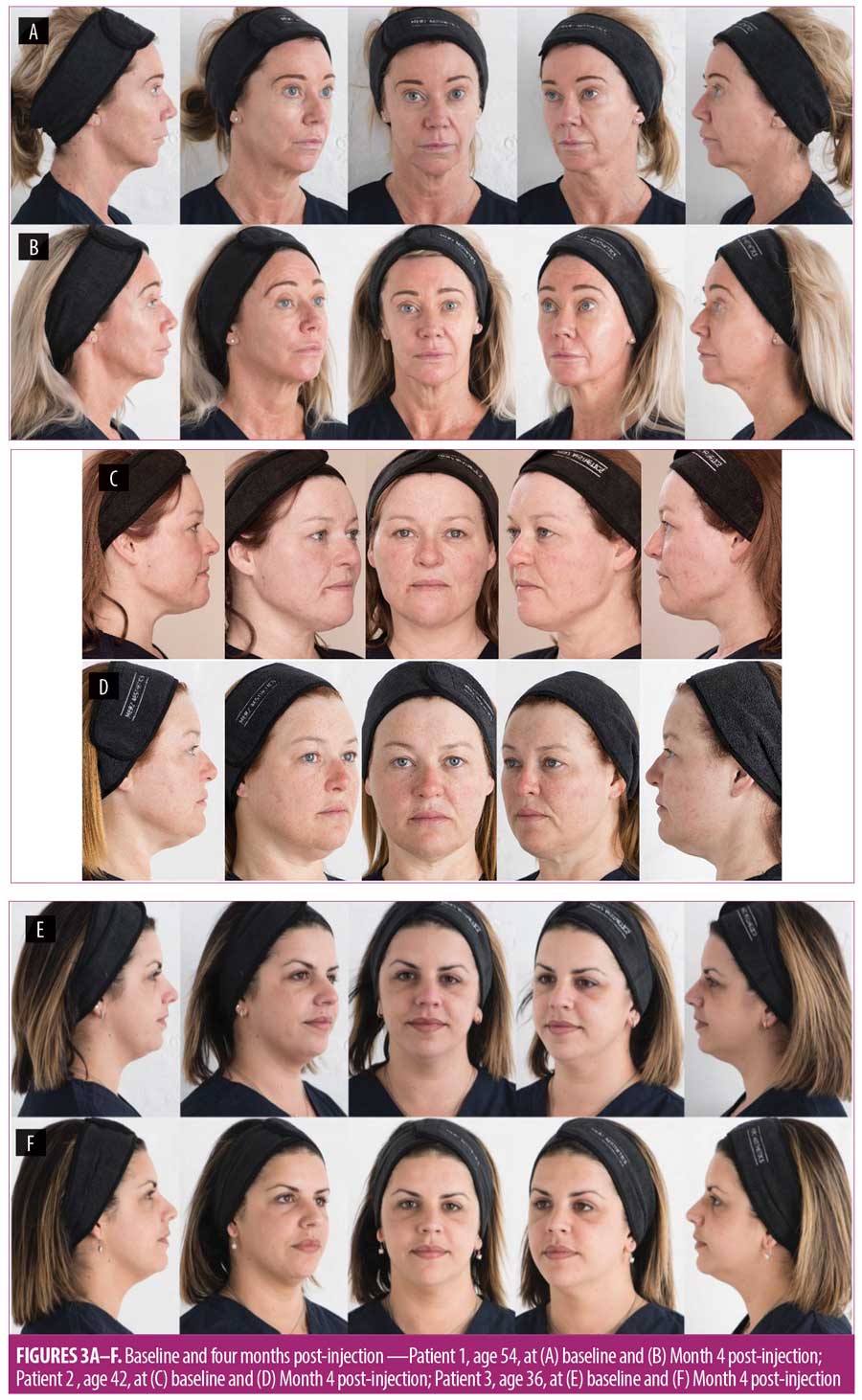
Filler threads in the jawline restored the lower curve of the oval and lengthened the central mandible. Adding a fan of threads over the anterior mandible from a point under the chin increased anterior projection of the lower mandible while also filling the submental crease area up to the lower lip (Figures 3A–F). This balanced approach adds volume anteriorly to the mandible and length and height to restore midline volume in the face.
Fillers in the preauricular area and temples restored lateral volume loss. Volume added centrally to the infraorbital hollows and around the piriform fossa restored central facial projection, together creating a soft curvature from the facial midline out and back to the lateral face. Filling of a scalloped frontal bone produced a smooth forehead curve and lifted the brow slightly.
Using the described approach, patients with wider, bulkier faces (Patients 2 and 3) can experience a slimming and softening effect (Figures 3D and F).
Four months post-injection, effectiveness endpoints were achieved in the three presented cases, all three patients also achieved their requested subtle improvements with a GAIS score of 2 or 3 (Tables 1 and 2). Skin tone, color, and texture benefits were reported by all three patients, as they were noted by their friends and colleagues, and all three patients reported satisfaction with subtle improvements without excessive filler use. At four months post-injection and following carrier gel reabsorption, volumization persisted without detectable loss by patients, investigator, or blinded evaluator. No adverse events were reported at any time.
Discussion
Theoretical concepts of beauty, such as the Ogee curves, Golden Ratio, and Phi were based on the facial shapes and proportions seen in young people.11,12,13 Many facial rejuvenation strategies use these concepts as guides, including addressing volume loss through filler augmentation in the mid-face, the lower face, and the lips or cheeks.14–19 Mature patients might request age-appropriate treatments that result in the appearance of health, vitality, and well-being (i.e., revitalization) over the appearance of youth. Revitalization of the aging face that does not focus on the facial characteristics of younger women, but rather takes into account the natural structural changes that occur with aging, is necessary for optimal results in older women.
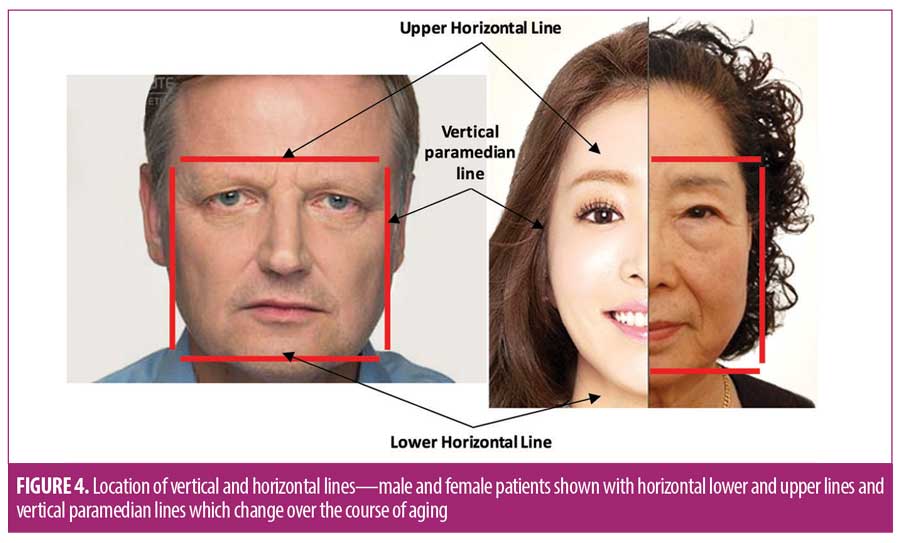
Mature patients can have depleted maxilla, mandible, and frontal bones, and diminished central face bony support.7,20–23 They also can have soft tissue movement, ligament loosening, and attenuation of facial fat. Attenuating soft tissues can fall toward the strong true ligaments in the face, including orbital, zygomatic, masseteric, and mandibular, producing a vertical paramedian line (Figure 4) with peripheral volume loss, and an effaced central face secondary to central bone loss. The loss of forehead bony support for soft tissues can result in the brow dropping and straightening, forming an upper horizontal edge. With loss of mandible height and jowl development, a lower horizontal edge can also form. These changes can produce a cuboid three-dimensional face shape that aging women might find unappealing. In aging faces of women, a cheek augmentation alone can improve nasolabial folds, infraorbital hollows, and fullness, but might not provide optimal results.
While this 12-point revitalization strategy was developed with the aging female face in mind, it can be applied to female patients of any age. This technique can produce more subtle outcomes by gradually replacing lost volume in key central and peripheral facial areas, restoring a natural, soft, and age-appropriate appearance.
Although the evaluation scores of the investigator and independent assessor in the presented cases were lower than that of the patients, satisfactory improvements in appearance were observed by all three patients who reported that their friends and family could not discern that an injectable procedure had been performed. This degree of subtlety might have enhanced the patients’ self-assessment scores.
In the presented cases, all injections were performed during one or two treatment sessions. However, treatment plans, including injection stages, should be created on an individual basis and according to each patient’s needs, during initial consultation. We have found that the preauricular and jawline deficiencies can usually be treated in one session, followed by the central and upper face at subsequent session(s). Further refinements should then be addressed. The volume of filler that is injected should be based on each patient’s individual requirements.
Analyzing facial shapes from a 3D perspective rather than the familiar two-dimensional (2D) view can help to achieve more natural looking results, thus potentially avoiding stigma associated with cosmetic facial procedures.24 For example, cheek augmentation improves the face when viewed in 2D.25 But this procedure might accentuate the paramedian edge between the hypoplastic maxilla centrally and any volume loss peripherally in the preauricular area, creating an unnatural cheek appearance, especially when viewed from behind. Lip augmentation can over-emphasize maxilla volume loss around the piriform fossa and create a distorted look, particularly when viewed laterally or from the posterior. This is caused by treating only one localized area in isolation in order to achieve a perceived greater return on investment. These distortions and contrasts, often associated with common rejuvenation techniques, become more obvious as the facial skeleton and overlying soft tissues age into the fifth and sixth decades of life. The holistic 3D revitalization strategy described here can produce more natural looking results, which potentially can increase patient satisfaction with outcomes.
Limitations. This report discusses the use of the 12-point revitalization guide on a limited number of patients; thus, further study on a larger group of patients is needed to support our results. In addition, the appraisal of a single investigator and patient self-reporting were used to assess treatment outcomes, which limits the determination of effectiveness endpoints. Thus, assessments by blinded, unbiased investigators are needed to produce more robust findings of treatment efficacy.
Conclusion
The described 12-point revitalization guide primarily addresses older female patients desiring the appearance of health, vitality, and well-being over the appearance of youth. By considering the aging female patient’s face holistically, implementing multidimensional assessments and interventions, prioritizing peripheral and central filler placement, and refraining from excessive localized treatments, physicians can create a visible but subtle, 3D, pan-facial improvement.
References
- Prendergast PM. Augmentation with injectable fillers. In: Peter M. Prendergast, Melvin A, editors. Aesthetic Medicine. Germany: Springer Verlag Heidelberg, 2011:297.
- Oranges CM, Schaefer KM, Gohritz A, Haug M, Schaefer DJ. The mirror effect on social media self-perceived beauty and its implications for cosmetic surgery. Plast Reconstr Surg Glob Open. 2016;4(11):e1088.
- Pastorek NJ. The female beautiful face. JAMA. 2017;317(12):1198–1200.
- MacCallum F, Widdows H. Altered images: understanding the influence of unrealistic images and beauty aspirations. Health Care Anal. 2016;1–11.
- Yan Y, Bissell K. The globalization of beauty: how is ideal beauty influenced by globally published fashion and beauty magazines? J Intercult Commun Res. 2014;43(3):194–214.
- Farkas JP, Pessa JE, Hubbard B, Rohrich RJ. The science and theory behind facial aging. Plastic and Reconstructive Surgery Global Open. 2013;1(1):
e8–e15. - Mendelson B, Wong CH. Changes in the facial skeleton with aging: implications and clinical applications in facial rejuvenation. Aesthetic Plast Surg. 2012;36(4):753–760.
- Yutskovskaya YA, Kogan EA. Improved neocollagenesis and skin mechanical properties after injection of diluted calcium hydroxylapatite in the neck and décolletage: a pilot study. J Drugs Dermatol. 2017.1;16(1):68–74.
- Wang F, Garza LA, Kang S, et al. In vivo stimulation of de novo collagen production caused by cross-linked hyaluronic acid dermal filler injections in photodamaged human skin. Arch Dermatol. 2007;143(2):155–163.
- Savoia A, Onori N, Baldi A. Efficacy of Skinfill plus filler in the management of facial aging: a multicenter, post-marketing clinical study. Biomed Dermatol. 2018;2: 2. https://doi.org/10.1186/s41702-017-0019-y.
- Swift A, Remington K. BeautiPHIcation™: a global approach to facial beauty. Clin Plast Surg. 2011;38(3):347–77,
- Pallett PM, Link S, Lee K. New “golden” ratios for facial beauty. Vision Res. 2010;50(2):149–154.
- Holland E. Marquardt’s Phi mask: pitfalls of relying on fashion models and the golden ratio to describe a beautiful face. Aesthetic Plast Surg. 2008;32(2): 200–208.
- Ferneini EM, Hapelas S, Watras J, et al. Surgeon’s guide to facial soft tissue filler injections: relevant anatomy and safety considerations. J Oral Maxillofac Surg. 2017 Dec;75(12):2667.e1–e5.
- de Maio M, DeBoulle K, Braz A, Rohrich RJ. Alliance for the Future of Aesthetics Consensus Committee. Facial assessment and injection guide for botulinum toxin and injectable hyaluronic acid fillers: focus on the midface. Plast Reconstr Surg. 2017 Oct;140(4):540e–550e.
- de Maio M, DeBoulle K, Braz A, Rohrich RJ. Alliance for the Future of Aesthetics Consensus Committee. Facial assessment and injection guide for botulinum toxin and injectable hyaluronic acid fillers: focus on the lower face. Plast Reconstr Surg. 2017 Oct;140(4):393e–404e.
- de Maio M, DeBoulle K, Braz A, Rohrich RJ. Alliance for the Future of Aesthetics Consensus Committee. Facial assessment and injection guide for botulinum toxin and injectable hyaluronic acid fillers: focus on the upper face. Plast Reconstr Surg. 2017 Oct;140(4):265e–276e.
- Wollina U. Facial rejuvenation starts in the midface: three-dimensional volumetric facial rejuvenation has beneficial effects on nontreated neighboring esthetic units. J Cosmet Dermatol. 2016 Mar;15(1):82–88.
- Moradi A, Watson J. Current concepts in filler injection. Facial Plast Surg Clin North Am. 2015 Nov;23(4):489–494.
- Pessa JE, Slice DE, Hanz KR, et al. Aging and the shape of the mandible. Plast Reconstr Surg. 2008;121:196–200.
- Pessa JE. An algorithm of facial aging: verification of Lambros’s theory by three-dimensional stereolithography, with reference to the pathogenesis of midfacial aging, scleral show, and the lateral suborbital trough deformity. Plast Reconstr Surg. 2000;106:479–488 (discussion 489–490).
- Shaw RB Jr, Kahn DM. Aging of the midface bony elements: a three-dimensional computed tomographic study. Plast Reconstr Surg. 2007;119:675–681.
- Pessa JE. The effect of skeletal remodeling on the nasal profile: considerations for rhinoplasty in the older patient. Aesthet Plast Surg. 1999;23(4): 239–242.
- Chen W, Qian W, Wu G, et al. Three-dimensional human facial morphologies as robust aging markers. Cell Res. 2015;25(5):574–587.
- Rohrich RJ, Pessa JE, Ristow B. The youthful cheek and the deep medial fat compartment. Plast Reconstr Surg. 2008;121(6):2107–2112.

