 by Shashank Bhargava, MD; Ujjwal Kumar, MD; and Krishnendra Varma, MD
by Shashank Bhargava, MD; Ujjwal Kumar, MD; and Krishnendra Varma, MD
Bhargava, Kumar, and Varma are with the Department of Dermatology at R.D. Gardi Medical College in Ujjain, India.
FUNDING: No funding was provided for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
ABSTRACT: Background. Acne scars are the most common sequele of the inflammatory process of acne and affects almost 95 percent of the patients with acne vulgaris. Hypertrophic scars and keloid scars result from excessive tissue formation; atrophic scars are characterized by loss or damage of tissue, which are further categorized into ice pick, rolling, and boxcar scars.
Method. A total of 45 patients underwent four sessions, four weeks apart, of subcision and microneedling and were assessed for scar grading three months after the final treatment session.
Results. Overall improvement was seen in 95.6 percent of patients (improvement by at least 1 grade) with slight erythema, edema and pain for 1 to 2 days. The improvement correlated with the patient-reported assessment of improvement in scars; 17.8 percent of patients perceived a 75- to 100-percent improvement in their acne scars, while 24.4 percent of patients perceived an improvement of 50 to 74 percent. The majority of the patients (55.5%) perceived an improvement of 25 to 49 percent in their scars.
Conclusion. Rolling and boxcar scars show more improvement compared to ice-pick scars. This combination is well tolerated in Fitzpatrick Skin Types III, IV and V, with no failure rates. We observed a high level of patient satisfaction and minimal downtime.
KEYWORDS: Atrophic acne scars, dark skin, microneedling, subcision
J Clin Aesthet Dermatol. 2019;12(8):18–22
Acne vulgaris is an extremely common condition and is prevalent in more than 90 percent of adolescents. It can occur in 12 to 14 percent of adults, leading to psychological and social problems.1,2 Acne scars are the most common sequelae of the inflammatory process and affect almost 95 percent of patients with acne vulgaris.3 Hypertrophic and keloid scars are the result of excessive tissue formation, while scars characterized by a loss or damage of tissue are atrophic. These are further categorized into ice pick, rolling, and boxcar scars.4 Atrophic scars can be managed medically and surgically; medical management includes the use of topical and oral retinoids, while surgical methods include punch excision, elliptical excision, punch elevation, or subcision. Different procedures include microdermabrasion, chemical peels, percutaneous collagen induction by microneedling and dermabrasion, soft-tissue augmentation, various ablative and nonablative lasers, and light energies.5 Combination therapies are more effective than solo treatments because patients typically have different types of scars that require volume restoration, tightening, and/or tissue movement (e.g., surgical modalities) along with resurfacing.6 From the aforementioned modalities, treatment should be tailored according to the patient’s needs, tolerance, and goals, while also considering the physician’s assessment, skills, and expectations. Microneedling, which entails rolling a preformed tool backward and forward with some pressure in various directions on the cutaneous areas affected by acne scars, works based on the principle of percutaneous collagen induction (PCI) therapy.7 Subcision is another technique in which a needle is inserted percutaneously adjacent to the scar to manipulate and release fibrous tissue, which pulls the scar down.8 During this process, bleeding is essential to clot formation and filling of the created space, which allows for skin elevation secondary to detachment from the scar tissue underneath.9 Subcision works best for rolling scars and is not an optimal modality for deep boxcar or icepick scars.10 Combining both modalities has a synergistic effect on the atrophic scars while remaining inexpensive and highly efficacious.
Materials and Methods
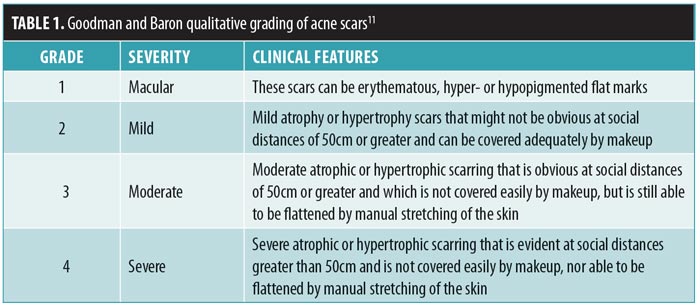
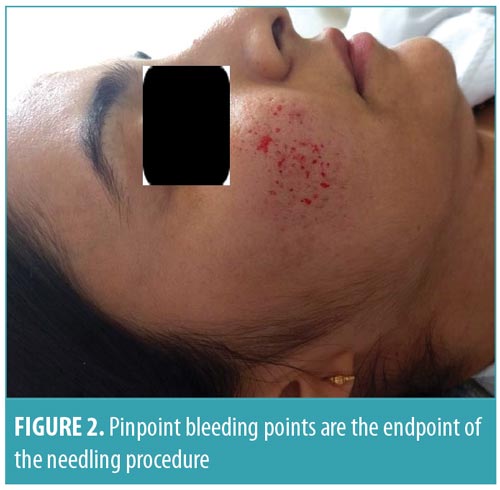
We conducted a prospective study at the Department of Dermatology, Venereology, and Leprosy in a tertiary-care teaching hospital. Fifty patients with atrophic acne scars were enrolled in the study from October 2016 to October 2017, and 45 patients completed all sessions of the treatment. Patients who had active acne, any active infection, were pregnant or lactating, had undergone any surgery or procedure for acne scars in previous three months, keloidal tendency, or unrealistic treatment expectations were excluded from the study. All patients were informed about the surgical intervention and written informed consent was collected. Routine investigations were performed, including complete blood count, bleeding and clotting time, fasting blood glucose, hepatitis B surface antigen, and human immunodeficiency virus tests. Study participants were photographed digitally and assessed clinically for the morphology of their scarring and their grades on the Goodman and Baron scale,11 defined in Table 1. Subcision and microneedling were performed at monthly intervals for four sittings. The affected area with scars was anesthetized using a thick application of topical anesthetic cream (i.e., eutectic mixture of prilocaine and lignocaine) under occlusion for 45 to 60 minutes. Subcision was performed using an 18-gauge, tribeveled, hypodermic needle. Needling was performed using a dermaroller (2-mm needle size, 192 needles) that was rolled on affected skin in vertical, horizontal, and diagonal directions until uniform fine pinpoint bleeding points appeared (Figures 1 and 2). Scar grading was evaluated by a blinded dermatologist three months after the final session. The response was evaluated clinically and aided by before and after photographs. Pretreatment grading of scars was compared with the final appearance of the scars using the Goodman and Baron scale. Patient response was also graded as either poor (0–24% improvement), good (25–49%), very good (50–74%), or excellent (75–100%). The statistical tools used for the analysis were SPSS version 23 (IBM Corp., Armonk, New York), graphical representation, descriptive statistics and the “Z” test for comparing two proportions before the treatment and after the treatment. Post-treatment adverse effects, including erythema, postinflammatory hyperpigmentation, and any interference with daily activities were noted. After the procedure, patients were advised to apply sunscreen over the entire face three times per day.

Results
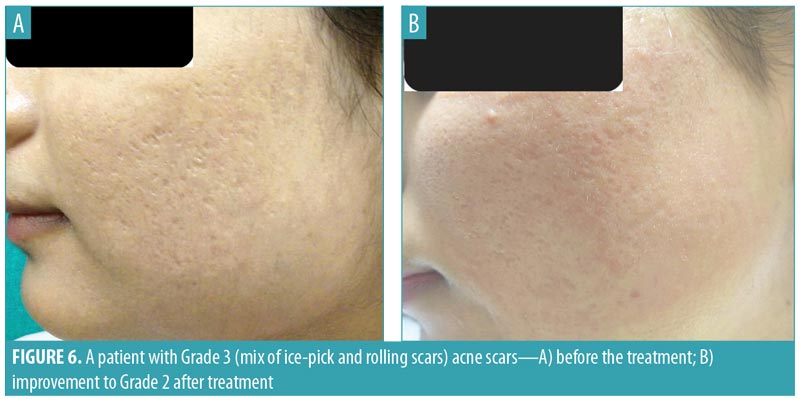
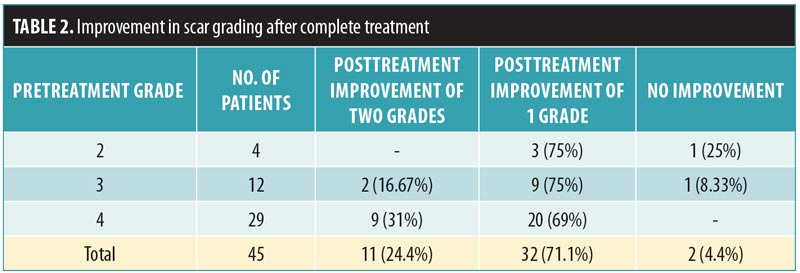
Out of 45 patients who completed the study, 27 (60%) were women and 18 (40%) were men, with an age range of 19 to 37 years and mean age of 24.2 years. Before starting the treatment, 29 patients had Grade 4 acne scars, 12 patients had Grade 3 acne scars, and four patients had Grade 2 acne scars. Among the patients with Grade 4 scars, nine patients (31%) showed improvement by two grades (i.e., their scars improved from Grade 4 to Grade 2; Figure 3). Twenty patients (69%) with Grade 4 scars showed improvement by one grade to Grade 3 (Figures 4 and 5). In the 12 patients with Grade 3 scars, two patients (16.67%) showed improvement by two grades to Grade 1, nine patients (75%) improved by one grade to Grade 2 (Figure 6), and one patient did not show any improvement. Three out of four patients with Grade 2 scars before treatment showed an improvement to Grade 1. Three months after starting the treatment, 95.56 percent of patients showed a reduction in acne scar grade by at least one grade, with no failure rate (Table 2).



Patient-reported assessment of their treatment outcomes were also documented. In patients with Grade 4 scars (Table 3), six patients (20.7%) graded their response to treatment as very good, while 23 patients (79.3%) reported good improvement. In patients with Grade 3 scars, five patients (41.67%) graded their response to treatment as excellent, four patients (33.3%) reported the response as very good, two patients (16.67%) graded their response as good, and one patient reported a poor result. Three patients (75%) with Grade 2 scars graded their response after treatment as excellent and one patient (25%) graded their improvement as very good.
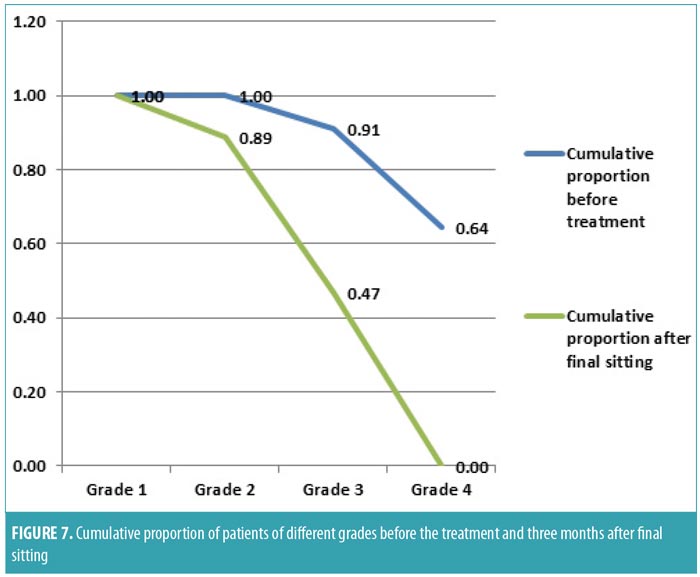
The cumulative probabilities of each grade before the treatment and at three months after the final treatment were also calculated (Figure 7). Before treatment, 64 percent of patients had Grade 4 scars, 27 percent of patients had Grade 3 scars, and nine percent of patients had Grade 2 scars. At three months after the final treatment, the proportion of patients with Grade 4 scars was reduced to zero percent (Z=3.88; p<0.001), patients with Grade 3 scars had increased from 27 to 47 percent (Z=1.58; p=0.06), the proportion of patients with Grade 2 had increased from 9 to 42 percent (Z=3.12; p<0.001), and patients with Grade 1 scars had increased from 0 to 11 percent (Z=2.75; p=0.02). Hence, with the treatment, the number of patients with Grade 1, 2, and 3 scars increased significantly, while patients with Grade 4 scars were significantly reduced.
The rolling and boxcar scar types showed good response to treatment, while little improvement was observed for icepick scars. Side effects were mild and transient. Posttreatment, transient erythema and edema were associated with pain. These lasted for 1 to 2 days, with no interference in the daily routines of our patients.
Discussion
Treatment modalities for acne scars can be classified depending upon the needs they satisfy, such as resurfacing, lifting/volumization, tightening, or surgical removal/movement of tissue that is required for the correction of the scarring.
Microneedling. Microneedling has demonstrated efficacy for improving acne scars, with improvements of at least 1 grade achieved in more than 90 percent of subjects in previous studies.12–14 Fabbrocini et al15 and Asif et al16 found that platelet-rich plasma combined with microneedling was more effective in treating acne scars than microneedling alone. Percutaneous collagen induction using microneedling creates thousands of micro clefts through the epidermis into the papillary dermis. The microwounds activate fibroblasts, resulting in collagen deposition. The needles also rupture old collagen strands in the most superficial layer of the dermis that tether scars and/or wrinkles.14 It has been postulated that needles have their own electrical potential, which triggers the proliferation of fibroblasts. Skin needling does not cause any damage to the stratum corneum or any other layers of the epidermis. Melanocyte number is not altered, which justifies the use of microneedling in Fitzpatrick Skin Types III to V.18
Subcision. Subcision is a technique that releases the fibrous tissue, resulting in scar elevation.8 Additionally, the induced dermal trauma results in clot formation and neocollagenesis with subsequent filling of the created space, which further enhances scar elevation. Deeper, wider, and more noticeable rolling scars improve more dramatically after subcision than do scars that were initially small or shallow, and boxcar scars improve much less than rolling scars.10 Aalami et al17 observed marked improvement using a combination of subcision with skin-suctioning therapy for atrophic acne scars. Furthermore, subcision has demonstrated increased efficacy when used synergistically with other modalities, such as fractional CO2 laser, fractionated microneedling radiofrequency, platelet rich plasma (PRP).19–22
Our study produced good results in patients with severe Grades 4 and 3 acne scars. Overall improvement was seen in 95.6 percent of patients (improvement by at least one grade) with slight erythema, edema, and pain lasting for 1 to 2 days. Overall, 24.4 percent patients had excellent improvement, while 71.1 percent patients showed a good response to the treatment. The improvement correlated with patient-reported assessments of the improvement in their scars: 17.8 percent of patients reported a 75 to 100-percent improvement in their acne scars, while 24.4 percent of patients reported an improvement of 50 to 74 percent. The majority of the patients (55.5%) reported an improvement of 25 to 49 percent. The procedure was well-tolerated by all patients.
Conclusion
As the demand for less-invasive, highly effective cosmetic procedures for acne scarring increases, the present combination of treatment for acne scars has shown efficacy not only in Grade 2 but also in more severe Grades 4 and 3 acne scars. Rolling and boxcar scars showed more improvement compared to icepick scars. This combination was well-tolerated in Fitzpatrick Skin Types III, IV, and V with no failure rates. There was a high level of patient satisfaction with minimal downtime.
Further studies with long-term follow-up are needed to confirm the results of our present study. Due to a paucity of minimally invasive multimodality therapy studies addressing acne scarring in dark skin, this present study might encourage safer treatment of severe acne scarring with minimally invasive multimodality approaches.
References
- Ghodsi SZ, Orawa H, Zouboulis CC. Prevalence, severity, and severity risk factors of acne in high school pupils: a community-based study. J Invest Dermatol. 2009;129(9):2136–2141.
- Williams C, Layton AM. Persistent acne in women: implications for the patient and for therapy. Am J Clin Dermatol. 2006;7(5):281–290.
- Layton AM, Henderson CA, Cunliffe WJ. A clinical evaluation of acne scarring and its incidence. Clin Exp Dermatol. 1994;19(4):303–308.
- Jacob CI, Dover JS, Kaminer MS. Acne scarring: a classification system and review of treatment options. J Am Acad Dermatol. 2001;45(1): 109–117.
- Rivera AE. Acne scarring: a review and current treatment modalities. J Am Acad Dermatol. 2008;59(4):659–676.
- Bhargava S, Cunha PR, Lee J, Kroumpouzos G. Acne scarring management: systematic review and evaluation of the evidence. Am J Clin Dermatol. 2018;19(4):459–477.
- Aust MC, Fernandes D, Kolokythas P, et al. Percutaneous collagen induction therapy: An alternative treatment for scars, wrinkles and skin laxity. Plast Reconstr Surg. 2008;121(4): 1421–1429.
- Orentreich DS, Orentreich N. Subcutaneous incisionless (subcision) surgery for the correction of depressed scars and wrinkles. Dermatol Surg. 1995;21(6):543–549.
- Nilforoushzadeh M, Lotv E, Nickkholgh E. Can subcision with the cannula be an acceptable alternative method in treatment of acne scars?. Med Arch. 2015;69(6):384–386.
- Alam M, Omura N, Kaminer MS. Subcision for acne scarring: technique and outcomes in 40 patients. Dermatol Surg. 2005;31(3):310–317.
- Goodman GJ, Baron JA. Postacne scarring: a qualitative global scarring grading system. Dermatol Surg. 2006;32(12):1458–1466.
- Majid I. Microneedling therapy in atrophic facial scars: an objective assessment. J Cutan Asthet Surg. 2009;2(1):26–30.
- Pandey A, Swain J P, Minj A. Assessment of microneedling therapy in the management of atrophic facial acne scars. J Evid Based Med Healthc. 2015;2(57):8911–8913.
- Varma K, Bhargava S, Kumar U. Microneedling for atrophic post acne scars: Is it effective? A prospective study of 36 patients at tertiary care centre. Hong Kong J Dermatol Venereol. 2018;26(2):52–57.
- Fabbrocini G, De Vita V, Pastore F, et al. Combined use of skin needling and platelet-rich plasma in acne scarring treatment. Cosmet Dermatol. 2011;24(4):177–183.
- Asif M, Kanodia S, Singh K. Combined autologous platelet-rich plasma with microneedling verses microneedling with distilled water in the treatment of atrophic acne scars: a concurrent split-face study. J Cosmet Dermatol. 2016;15(4):434–443.
- Aalami HS, Balighi K, Lajevardi V, Akbari E. Subcision-suction method: a new successful combination therapy in treatment of atrophic acne scars and other depressed scars. J Eur Acad Dermatol Venereol. 2011;25(1):92–99.
- Sharad J. Combination of microneedling and glycolic acid peels for the treatment of acne scars in dark skin. J Cosmet Dermatol. 2011;10(4): 317–323.
- Anupama YG, Wahab AJ. Effectiveness of CO2 laser with subcision in patients with acne scars. J Cosmet Laser Ther. 2016;18(7):367–371.
- Nilforoushzadeh MA, Faghihi G, Jaffary F, et al. Fractional carbon dioxide laser and its combination with subcision in improving atrophic acne scars. Adv Biomed Res. 2017;6:20.
- Faghihi G, Poostiyan N, Asilian A, et al. Efficacy of fractionated microneedle radiofrequency with and without adding subcision for the treatment of atrophic facial acne scars: a randomized split-face clinical study. J Cosmet Dermatol. 2017;16(2): 223–229.
- Bhargava S, Kroumpouzos G, Varma K, Kumar U. Combination therapy using subcision, needling and platelet rich plasma in the management of Grade 4 atrophic acne scars: A pilot study. J Cosmet Dermatol. 2019;18(4):1092–1097.

