J Clin Aesthet Dermatol. 2019;12(6):42–44
 by Sydney E. Liang, MD; Gelareh Homayounfar, MD; Edward Heilman, MD; and Tracey N. Liebman MD, FAAD
by Sydney E. Liang, MD; Gelareh Homayounfar, MD; Edward Heilman, MD; and Tracey N. Liebman MD, FAAD
Dr. Liang and Dr. Liebman are with the Ronald O. Perelman Department of Dermatology at the New York University School of Medicine in New York, New York. Dr. Homayounfar and Dr. Heilman are with the Department of Dermatology at the State University of New York (SUNY) Downstate Medical Center in Brooklyn, New York.
FUNDING: No funding was received for this study.
DISCLOSURES: The authors have no conflicts of interest relevant to the content of this article.
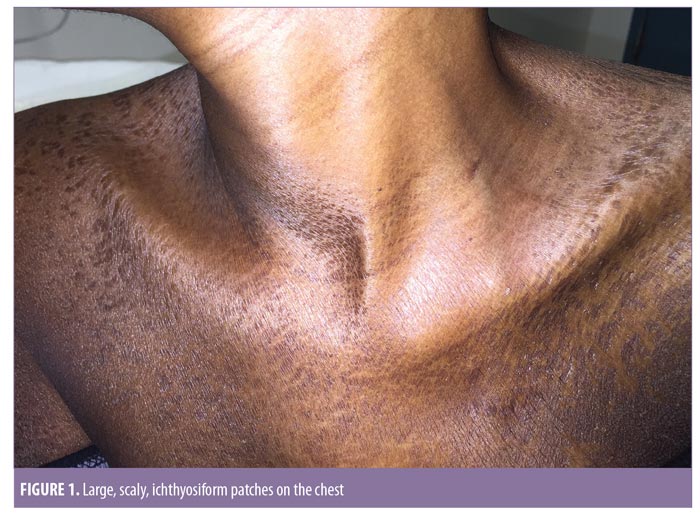
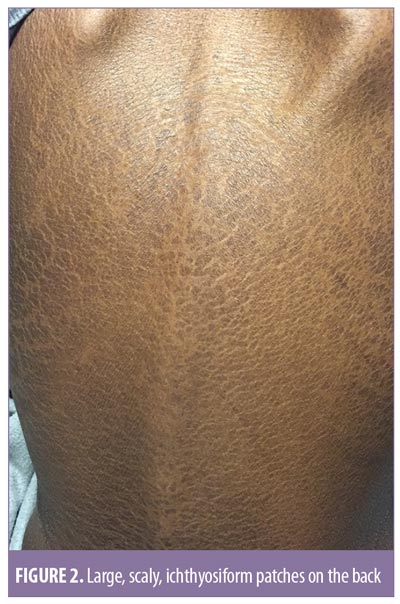
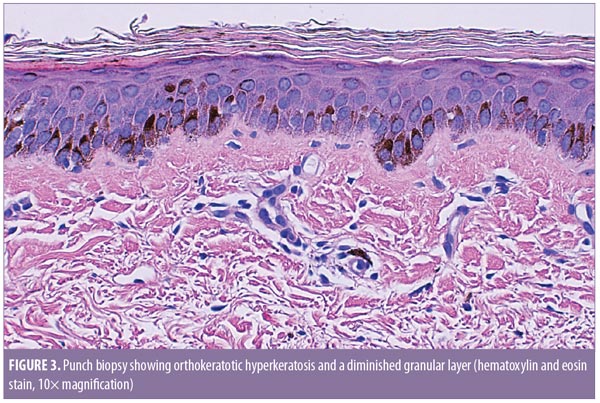
ABSTRACT: Acquired ichthyosis is an uncommon disorder of cornification. It characteristically presents as symmetric scaling of the skin on the trunk and extensor surfaces of the extremities. It is clinically and histologically similar to ichthyosis vulgaris; however, acquired ichthyosis develops later in life and has been associated with various malignancies, infections, medications, autoimmune diseases, metabolic disorders, and malnutrition. We describe a case of a 35-year-old woman with active pulmonary tuberculosis and a history of breast cancer who presented with a several-month history of a widespread, scaly, pruritic skin eruption. Physical examination revealed fine, scaly patches on the extremities with relative sparing of the flexures and larger, scaly, ichthyosiform patches on the chest and back. Skin biopsy revealed orthokeratotic hyperkeratosis and a diminished granular layer, consistent with a diagnosis of acquired ichthyosis. Further evaluation, including positron-emission tomography/computed tomography scan, revealed hypermetabolic infiltrates and cavitation in the lungs, consistent with active pulmonary tuberculosis; there was no evidence of new or recurrent malignancy. The patient was treated with antituberculosis drugs and topical ammonium lactate cream. With incident cases rarely reported in the literature, this case of new-onset ichthyosis in the setting of active pulmonary tuberculosis highlights the distinctive clinical and histologic features of acquired ichthyosis and emphasizes the relationship of acquired ichthyosis with underlying systemic disease, particularly infection.
KEYWORDS: Active pulmonary tuberculosis, acquired ichthyosis, new-onset
Ichthyoses are a group of cutaneous disorders of keratinization that can be congenital or acquired.1 They are clinically characterized by dry, rough skin with prominent scaling.2 Acquired ichthyosis, which is nonhereditary and uncommon, typically presents as symmetric scaling of the skin on the trunk and extensor surfaces of the extremities.3 While clinically and histologically similar to ichthyosis vulgaris, an autosomal dominant hereditary ichthyosis, acquired ichthyosis (AI) develops later in life and is often associated with various conditions, including infections, malnutrition, malignancies, metabolic disorders, and autoimmune diseases.3–8 Several medications have also been associated with the development of AI.3,4,9–11 Here, we present a case of AI in a patient with active pulmonary tuberculosis.
Case Presentation
A 35-year-old woman with active pulmonary tuberculosis and a history of breast cancer presented with a several-month history of a widespread, scaly, pruritic skin eruption. Upon physical examination, it was noted that there were fine, scaly patches on the bilateral upper and lower extremities, with relative sparing of the flexural areas. Physical examination also revealed larger, scaly, ichthyosiform patches on the chest and back (Figures 1 and 2). There was no organomegaly or lymphadenopathy. Use of over-the-counter emollients provided no improvement. There was no personal or family history of ichthyosis. She had a remote history of breast cancer, which was in complete remission status following radiation and chemotherapy. At the time of presentation, she was being treated for active pulmonary tuberculosis with rifampin, isoniazid, pyrazinamide, and ethambutol. She was not taking any other medications and had no known drug allergies. The patient was human immunodeficiency virus (HIV)-negative.
Punch biopsy of the skin revealed orthokeratotic hyperkeratosis and a diminished granular layer (Figure 3), consistent with a diagnosis of AI. Further evaluation, including positron-emission tomography/computed tomography scan, was performed at an outside hospital and showed hypermetabolic infiltrates and cavitation in the lungs, consistent with active pulmonary tuberculosis. There was no evidence of new or recurrent malignancy. The patient was diagnosed with AI in the setting of active pulmonary tuberculosis. In addition to treatment with antituberculosis drugs, she was treated with topical ammonium lactate cream.
Unfortunately, the patient did not follow-up after her tuberculosis treatment was completed. Therefore, it is unknown whether the AI completely resolved.
Discussion
AI most commonly occurs in adulthood and is often a sign of systemic disease.4 Clinically and histologically similar to the autosomal dominant ichthyosis vulgaris, AI occurs when there is a disruption in the process of cornification, resulting in hyperkeratosis, scaling, and abnormalities of the skin’s barrier function.3,4 Although the underlying pathophysiologic mechanism remains unclear, low levels of vitamin A, cholesterol deficiency, impaired lipogenesis, increased levels of tumor necrosis factor alpha, and other alterations in the host’s immune system have all been proposed as potential mechanisms of the skin disease.1,4,12,13
Clinically, AI classically presents as xerosis with symmetric, prominent scaling.3 The severity of skin lesions can range from minor roughness and dryness to desquamation of large, plate-like scales.2 AI primarily affects the trunk and extremities, with relative sparing of the flexural areas, palms, and soles. Histologically, AI characteristically demonstrates compact orthohyperkeratosis, a diminished or absent granular layer, a reduced rete-papilla pattern, and the absence of an inflammatory infiltrate in the dermis.3,11
Often a sign of internal disease, AI is most frequently described in the setting of malignancy.3 Hodgkin’s disease, the first malignancy reported in association with AI, is the most common.4 Other malignancies, including non-Hodgkin’s lymphoma, leiomyosarcoma, mycosis fungoides, multiple myeloma, Kaposi’s sarcoma, and carcinomas of the breast, lung, and cervix have been reported.8,14,15 Therefore, a thorough investigation for underlying disease, including malignancy, is critical to perform once AI has been identified. Although the patient in this case had a remote history of breast cancer, her current presentation of AI was not considered to be associated with her previous diagnosis of breast cancer, as she was in complete remission when the ichthyosis initially developed. Furthermore, upon closer investigation, she had no evidence of recurrent or new malignancy.
AI has also been identified in the setting of systemic conditions other than malignancies, such as infections, metabolic disorders, autoimmune diseases, and nutritional disorders.3–5 However, despite its association with various infections, including leprosy and HIV/acquired immunodeficiency syndrome (AIDS), incident cases of AI in the setting of tuberculosis have been rarely reported in the literature.6–8 To our knowledge, only two cases of AI secondary to tuberculosis have been described in the modern literature.16,17 In both cases, AI revealed underlying extrapulmonary (lymph node and hepatic) tuberculosis, and neither patient had active pulmonary tuberculosis upon evaluation.16,17 In a third case of an elderly man with pleural tuberculosis, AI developed not in the setting of the tuberculosis infection itself but rather in the setting of isoniazid therapy, as the ichthyosis resolved when isoniazid treatment was stopped and recurred upon reintroduction of therapy.9 Our patient, who was also receiving treatment with isoniazid for her active pulmonary tuberculosis, developed the ichthyosis several months prior to the initiation of antituberculosis therapy.
A unique variant of AI, pityriasis rotunda, which classically presents as scaly, circular, sharply demarcated patches, has been reported in the literature in a number of patients with pulmonary tuberculosis.4 In South Africa, tuberculosis has been found to be the most prevalent condition associated with pityriasis rotunda.18 Our patient, however, did not present with the characteristic cutaneous lesions of pityriasis rotunda and instead demonstrated the widespread, scaly skin eruption typical of generalized AI.
The management of AI can be challenging and complex given the number of associated diseases and medications. Treatment should be directed at the underlying disease if one is identified upon evaluation.3 Generally, treatment of the underlying disorder will result in regression of the ichthyotic lesions.1,4 However, hydration, lubrication, and keratolysis with topical agents such as urea and salicylic, lactic, and glycolic acids can be useful to help improve xerosis and remove scaling.1 Additionally, prophylactic measures, such as antiseptic soaps, should also be considered, since patients with AI are predisposed to skin infections secondary to the impaired barrier function of the skin.3
AI, an uncommon disorder of cornification, has been rarely reported among patients with tuberculosis in the modern literature. The present case of AI in the setting of active pulmonary tuberculosis augments the current literature on AI and further emphasizes the significance of AI as a cutaneous marker of an underlying internal disease, particularly infection. The relationship of AI with underlying systemic disease should always be considered when evaluating adult patients presenting with new-onset ichthyosis, and given the variety of diseases, medications, and physiologic conditions reported in association with AI, a comprehensive diagnostic investigation for internal disease is essential.
References
- Okulicz JF, Schwartz RA. Hereditary and acquired ichthyosis vulgaris. Int J Dermatol. 2003;42(2): 95–98.
- Word AP, Cayce R, Pandya AG. Beware of underlying malignancy: acquired ichthyosis. Am J Med. 2014;127(3):202–204.
- Patel N, Spencer LA, English JC, Zirwas MJ. Acquired ichthyosis. J Am Acad Dermatol. 2006;55(4):647–656.
- Griffin LJ, Massa MC. Acquired ichthyosis and pityriasis rotunda. Clin Dermatol. 1993;11(1): 27–32.
- Holzman SB, Durso SC. Nutritional deficiency and acquired ichthyosis. J Gen Intern Med. 2017;32(10):1161–1162.
- Goodman DS, Teplitz ED, Wishner A, et al. Prevalence of cutaneous disease in patients with acquired immunodeficiency syndrome (AIDS) or AIDS-related complex. J Am Acad Dermatol. 1987;17(2 Pt 1):210–220.
- Schulz EJ. Ichthyosiform Conditions Occurring in Leprosy. Br J Dermatol. 1965;77:151–157.
- Young L, Steinman HK. Acquired ichthyosis in a patient with acquired immunodeficiency syndrome and Kaposi’s sarcoma. J Am Acad Dermatol. 1987;16(2 Pt 1):395–396.
- Kouismi H, Bourkadi JE, Iraqi G. Cutaneous ichthyosis secondary to isoniazid. Egypt J Chest Dis Tuberc. 2013;62:3.
- Xu H, Busam KJ, Mauro MJ, Markova A. Ponatinib-induced ichthyosiform drug eruption: insights into acquired ichthyosis. Dermatol Online J. 2017;23(10). pii: 13030/qt2zf9r6vw.
- Errichetti E, Stinco G, Pegolo E, Patrone P. Acquired ichthyosis during acitretin therapy for psoriasis vulgaris. J Eur Acad Dermatol Venereol. 2016;30(1):181–182.
- Akpinar TS, Ozkok A, Bakkaloglu OK, Saka B. Acquired ichthyosis as a presenting finding of Hodgkin’s lymphoma. Int J Hematol. 2012;96(4):401–402.
- Moore RL, Devere TS. Epidermal manifestations of internal malignancy. Dermatol Clin. 2008;26(1):17–29, vii.
- Flint GL, Flam M, Soter NA. Acquired ichthyosis. A sign of nonlymphoproliferative malignant disorders. Arch Dermatol. 1975;111(11): 1446–1447.
- Tan AR. Cutaneous manifestations of breast cancer. Semin Oncol. 2016;43(3):331–334.
- Rabhi M, Ennibi K, Berady S, et al. [Acquired ichthyosis revealing hepatic and lymph node tuberculosis]. Presse Med. 2006;35(12 Pt 1):1839–1841.
- Vagamon B, Dupuy A, Fontaine J, et al. [Acquired circinated ichthyosis revealing a lymph node tuberculosis]. Ann Dermatol Venereol. 2003;130(6–7):635–637.
- Swift PJ, Saxe N. Pityriasis rotunda in South Africa—a skin disease caused by undernutrition. Clin Exp Dermatol. 1985;10(5):407–412.

