 by Shimona Garg, MD; Jasleen Sandhu, MD; Amrit Kaur, MD; and Raj Pal Singh Punia, MD
by Shimona Garg, MD; Jasleen Sandhu, MD; Amrit Kaur, MD; and Raj Pal Singh Punia, MD
Drs. Garg, Sandhu, Kaur, are with the Department of Dermatology and Venereology and Dr. Punia is with the Department of Pathology, all at the Government Medical College and Hospital in Chandigarh, India.
Funding/disclosures. The authors have no conflicts of interest relevant to the content of this article.
Dear Editor:
The term acquired digital fibrokeratoma (ADFK) was first coined by Bart et al1 in 1968.It has a characteristic clinical presentation and histology. Clinically, ADFK usually presents as a small, solitary, dome or bullet shaped lesion, with a collarette of slightly raised skin at its base. Histopathologically, the lesion shows a fibrous dermal core with both interwoven and parallel arrangements of collagen.2 Here, we report a case of this uncommon entity.
 Case report. A 52-year-old man presented with an asymptomatic, solitary, dome-shaped, pedunculated, firm, 1cm × 0.4cm × 0.2cm lesion, with a color matching the surrounding skin, located on the tip of the right thumb (Figure 1). The patient reported the growth being present for six months; after an initial growth phase of several weeks, the lesion stabilized but did not regress. The lesion was painless and was not associated with itching or bleeding, even after trauma. The patient reported a history of significant trauma to the tip of the thumb prior to onset of the lesion in the same area. The tumor was surrounded by a depression, which had a hyperkeratotic edge. All other physical examination findings were unremarkable.
Case report. A 52-year-old man presented with an asymptomatic, solitary, dome-shaped, pedunculated, firm, 1cm × 0.4cm × 0.2cm lesion, with a color matching the surrounding skin, located on the tip of the right thumb (Figure 1). The patient reported the growth being present for six months; after an initial growth phase of several weeks, the lesion stabilized but did not regress. The lesion was painless and was not associated with itching or bleeding, even after trauma. The patient reported a history of significant trauma to the tip of the thumb prior to onset of the lesion in the same area. The tumor was surrounded by a depression, which had a hyperkeratotic edge. All other physical examination findings were unremarkable.
Histopathological examination revealed epidermal hyperkeratosis and acanthosis with branching rete ridges. The dermis showed an increase in collagen bundles, most of which were vertically oriented with minimal lymphomononuclear infiltrate and a few congested blood vessels (Figure 2). On the basis of clinical and histopathological findings, the patient was diagnosed with ADFK; the condition was treated with shave excision. Recurrence had not occurred at the six-month follow-up visit.
Discussion. ADFK is an uncommon, benign, fibroepithelial tumor that presents as an asymptomatic solitary nodule, usually less than 1cm in diameter, that gradually increases in size over time with no tendency toward spontaneous regression. It is predominantly located on the fingers and toes near the phalangeal joints. Due to its predominant location on the fingers and toes, it was labeled as acral fibrokeratoma by Verallo.3 Although the exact etiology is unknown, trauma to the area of the lesion seems to be a contributing factor.4 Kint et al5 suggested that the condition develops from the neoformation of collagen by fibroblasts, resulting in more capillaries and fibroblasts and coarser elastic fibers than the surrounding dermis. Nemeth and Penneys6 reported the presence of factor XIIIa in ADFK.
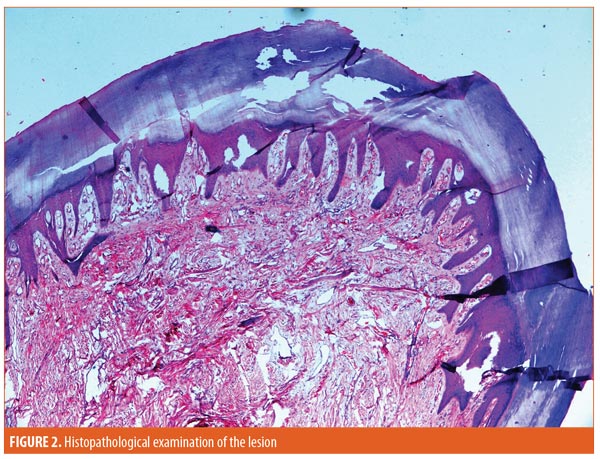 Histopathologic examination of ADFK typically reveals epidermis with hyperkeratosis and irregular acanthosis; the core of the lesion is formed of thick, interwoven bundles of collagen with dilated capillaries predominantly oriented along the long axis of the lesion.2 Based on clinical and histopathologic features, Kint et al4 classified ADFKs into three types: Type I is a dome-shaped lesion that contains fibroblasts between collagen bundles, fine elastic fibers, and numerous capillaries in the dermis; Type II is a tall, hyperkeratotic lesion that contains many more fibroblasts and less elastic fiber than Type I lesions; and Type III is a flat- to dome-shaped lesion that is characterized by poor cellular and edematous structure and no elastic fibers. The tumor in our case had the typical histopathologic findings of Type I ADFK.
Histopathologic examination of ADFK typically reveals epidermis with hyperkeratosis and irregular acanthosis; the core of the lesion is formed of thick, interwoven bundles of collagen with dilated capillaries predominantly oriented along the long axis of the lesion.2 Based on clinical and histopathologic features, Kint et al4 classified ADFKs into three types: Type I is a dome-shaped lesion that contains fibroblasts between collagen bundles, fine elastic fibers, and numerous capillaries in the dermis; Type II is a tall, hyperkeratotic lesion that contains many more fibroblasts and less elastic fiber than Type I lesions; and Type III is a flat- to dome-shaped lesion that is characterized by poor cellular and edematous structure and no elastic fibers. The tumor in our case had the typical histopathologic findings of Type I ADFK.
Prior to diagnosis, ADFK must be differentiated from other conditions such as cutaneous horn, rudimentary supernumerary digit, Koenen’s tumor, pyogenic granuloma, verruca vulgaris, dermatofibroma, superficial acral fibromyxoma, and eccrine poroma. Differentiation is important in order to predict the response to treatment and/or excision and recurrence after treatment. Cutaneous horn is an uncommon epidermal tumor comprising a column of keratin arising from underlying benign, premalignant, or malignant processes.7 Supernumerary digit is a congenital digital anomaly occurring at the base of the fifth finger, usually bilaterally, that contains numerous neural bundles in dermis.8 Koenen’s tumor is a periungual or subungual fibroma, devoid of a hyperkeratotic tip, that contains dilated blood vessels surrounded by fibroblasts and dense collagen.9 Pyogenic granuloma is a rapidly growing papule that often bleeds, originates as a response to trauma, and contains proliferating fibroblasts and budding endothelial cells.10 Verruca vulgaris on the palms of the hands and soles of the feet presents as painful papules with a loss of surface dermatoglyphics, koebnerization, and the presence of parakeratosis, papillomatosis, and koilocytes on histopathology.11 Eccrine poroma is a sweat gland tumor consisting of broad anastomosing bands of uniform cuboidal epithelial cells presenting as a painful papule or nodule protruding from a distinct cup-shaped shallow depression.12 Superficial acral fibromyxoma is a benign fibromyxoid tumour usually present in subungual or periungual regions as a painless nodule after trauma, composed of spindle- and stellate-shaped cells in myxocollagenous stroma with accentuated vascularity.13
Conclusion. Treatment for ADFK includes surgical excision, which is both curative and diagnostic. Usually, there is no recurrence after complete surgical excision. This uncommon entity should be differentiated from other solitary, papulonodular lesions of digits by its characteristic clinical and histopathological features.
References
- Bart RS, Andrade R, Kopf AW, Leider M. Acquired digital fibrokeratomas. Arch Dermatol. 1968; 97(2):120–129.
- Rathi SK, Dogra D, Khanna N. Acquired digital fibrokeratoma. Indian J Dermatol Venereol Leprol. 1998;64(2):78–79.
- Verallo VVM. Acquired digital fibrokeratomas. Br J Dermatol. 1968;80:730–736.
- Altman DA, Griner JM, Faria DT. Acquired digital fibrokeratoma. Cutis. 1994;54(2):93–94.
- Kint A, Baran R, De Keyser H. Acquired (digital) fibrokeratoma. J Am Acad Dermatol. 1985;12(5 Pt 1): 816–821.
- Nemeth AJ, Penneys NS. Factor XIIIa is expressed by fibroblasts in fibrovascular tumors. J Cutan Pathol. 1989;16(5):266–271.
- Copcu E, Sivrioglu N, Culhaci N. Cutaneous horns: are these lesions as innocent as they seem to be? World J Surg Oncol. 2004;2:18.
- Moon SH, Cho SH, Lee JD et al. A case of acquired giant digital fibrokeratoma. J Clin Investigat Dermatol. 2016;4(2):2.
- Devi B, Dash M, Behera B, Puhan MR. Multiple koenen tumors: an uncommon presentation. Indian J Dermatol. 2011;56(6):773–775.
- Piraccini BM, et al. Periungual and subungual pyogenic granuloma. Br J Dermatol. 2010;163(5):941–953.
- Elder DE, Massi D, Scolyer R et al. WHO Classification of skin tumours. 4th ed. Lyon: International Agency for Research on Cancer; 2018. 54.
- Wankhade V, Singh R, Sadhwani V, Kodate P. Eccrine poroma. Indian Dermatol Online J. 2015;6(4):304–305.
- Hashimoto, K., Nishimura, S., Oka, N et al. Aggressive superficial acral fibromyxoma of the great toe: a case report and mini-review of the literature. Mol Clin Oncol. 2018; 9(3): 310–314.

